» Different classifications of influenza Q&As
» Influenza Q&As
What is seasonal influenza?
Seasonal influenza (or “flu”) is most often caused by type A or B influenza viruses. Symptoms include sudden onset of fever, cough (usually dry), headache, muscle and joint pain, sore throat and a runny nose. The cough can be severe and can last 2 or more weeks. Most people recover from fever and other symptoms within a week without requiring medical attention. However, influenza can cause severe illness or death in high risk groups (see Who is most at risk? below).
Seasonal epidemics occur mainly during winter, from October to March in the northern hemisphere and April to September in the southern hemisphere. In tropical and subtropical countries, seasonal influenza can happen all year round.
How can I avoid getting the flu?
The best way to avoid getting the flu is to get the flu vaccine every year. Influenza viruses evolve constantly, and twice a year WHO makes recommendations to update the vaccine compositions. For the 2016-2017 northern hemisphere influenza season, the vaccine formulation was updated in February 2016 to contain two types, A viruses (H1N1 and H3N2), and a type B virus.
WHO recommends annual vaccination for high-risk groups including health care workers. People should ideally get vaccinated just before the influenza season begins for the most effective coverage, although getting vaccinated at any time during the influenza season can still help prevent flu infections.
Who is most at risk?
People most at risk for severe seasonal influenza are:
pregnant women at any stage of pregnancy
children younger than 5 years
people older than 65 years
people with chronic medical conditions such as HIV/AIDS, asthma, heart and lung diseases and diabetes
people with increased risk of exposure to influenza, which includes health care workers.
How is it treated?
People with the flu should drink plenty of water and rest. Most people will recover within a week. Antiviral drugs for influenza can reduce severe complications and deaths although influenza viruses can develop resistance to the drugs. They are especially important for high-risk groups. Ideally, these drugs need to be administered early (within 48 hours of the onset of symptoms). Antibiotics are not effective against influenza viruses.
How do you stop it from spreading?
Influenza can spread quickly between people when an infected person coughs or sneezes, dispersing droplets of the virus into the air. It can be also spread by hands contaminated by the virus.
Precautionary measures should be taken to limit transmission. People should cover their mouth and nose with a tissue when coughing, then throw it out and wash their hands thoroughly and regularly.
Is seasonal influenza linked to pandemic flu?
Seasonal influenza outbreaks are caused by small changes in viruses that have already circulated, and to which many people have some immunity.
A pandemic occurs when an influenza virus emerges that most people do not have immunity from because it is so different from any previous strain in humans. This enables the strain to spread easily between people.
Seasonal influenza viruses may contribute to the emergence of a pandemic virus; and once a pandemic virus has been established, as with the pandemic A(H1N1) in 2009, it can become a seasonal virus.
Different classifications of influenza Q&As
What is influenza?
Influenza is a respiratory virus that can infect the nose, throat and sometimes the lungs. It can be found in both humans and animals.
What is pandemic influenza?
Pandemic influenza is an influenza virus that most people do not have immunity from because it is so different from any previous strain in humans. This allows the strain to spread easily between people.
What is avian influenza?
Avian influenza viruses normally spread between birds. However, some viruses have been found to infect humans. When avian influenza infects humans, symptoms may range from mild upper respiratory infection (fever and cough) to severe pneumonia, acute respiratory distress syndrome (difficulty breathing), shock and even death.
What is zoonotic influenza?
Zoonotic influenzas generally spread within animals. One of the most well known is swine influenza viruses that circulate between pigs. However, other animals such as horses and dogs can be infected with their own influenza viruses (e.g. canine influenza viruses, equine influenza viruses, etc.). Sometimes these zoonotic influenzas can infect humans. For example, some countries have reported cases of human infection from certain swine influenza viruses. Close proximity to infected pigs or visiting locations where pigs are exhibited has been reported for most human cases, but some limited human-to-human transmission has occurred.
What is seasonal influenza?
Seasonal influenza (or “flu”) is most often caused by type A or B influenza viruses. Symptoms include sudden onset of fever, cough (usually dry), headache, muscle and joint pain, sore throat and a runny nose. The cough can be severe and can last 2 or more weeks. Most people recover from fever and other symptoms within a week without requiring medical attention. However, influenza can cause severe illness or death in high-risk groups.
Seasonal epidemics occur mainly during winter, from October to March in the northern hemisphere and April to September in the southern hemisphere. In tropical and subtropical countries, seasonal influenza can happen all year round.
How is seasonal influenza linked to the other types of influenza?
Seasonal influenza outbreaks are caused by small changes in viruses that have already circulated, and to which many people have some immunity.
Seasonal influenza viruses may contribute to the emergence of a pandemic virus; and once a pandemic virus has been established, as with the pandemic A(H1N1) in 2009, it can become a seasonal virus.
Are the symptoms different of different influenzas?
No, the symptoms are not different for different influenzas. Avian, zoonotic and pandemic influenza can have more severe outcomes as they are generally new and you are unlikely to have existing immunity to protect you.
Influenza vaccines Q&As
Who should take the influenza vaccine this year?
With the persistence of the COVID-19 pandemic and concerns that influenza infections may increase the burden on health care systems, WHO recommends that health care workers and older adults be given top priority for the influenza vaccine this year, especially where there is limited supply. Health care workers are at high risk of getting infected through their regular contact with patients and the influenza vaccine will contribute to minimizing absenteeism due to influenza and decrease disruption to the workforce.
Older adults are at much greater risk of severe disease and death from influenza when compared to younger adults, so the vaccine will help decrease the risks for that population. If the influenza vaccine supply still allows for others to get vaccinated, then individuals with underlying health conditions, pregnant women and children should be prioritized next in no particular order.How effective is the influenza vaccine?
The influenza vaccine is the best tool we have for preventing influenza and reducing the risk of serious complications and even death. The effectiveness of the vaccine can vary from one year to another, depending on the types of influenza viruses circulating and how well they match with the vaccine. It also depends on the health status and age of the person vaccinated, as well as time since vaccination. On average, the vaccine prevents around 60% of infections in healthy adults aged 18–64 years. Influenza vaccines become effective about 14 days after vaccination.
Do people need to be vaccinated against influenza every winter?
Yes. Influenza viruses constantly change and different strains can circulate each year. In addition, people’s immunity against influenza decreases over time. Seasonal influenza vaccines are therefore updated to reflect the most commonly circulating strains each year in order to provide the people who take them the highest possible immunity against these strains.
Is the influenza vaccine safe?
Yes. Seasonal influenza vaccines have been in use for more than 50 years. They have been administered to millions of people and have a good safety record. Every year, national medicines regulatory authorities carefully examine each influenza vaccine before it is licensed. Systems are in place to monitor and investigate any reports of adverse events following influenza immunization.
Does the influenza vaccine decrease immunity against other diseases like COVID-19?
No. The purpose of any vaccine is to train the immune system on how to respond if it encounters the real disease in the future. This training does not affect the immune system against other diseases but rather strengthens it against the target disease. This immunity may last for a short period of time or for many years depending on the type of disease and type of vaccine. The influenza vaccine is considered good for one year, after which immunity against the disease decreases.
Does the influenza vaccine protect against COVID-19?
No, because influenza and COVID-19 are two different diseases. But because both respiratory diseases can impact the health of those infected in severe ways, getting immunized against influenza can decrease the impact of this disease on someone who may already be struggling with COVID-19. It is better for patients and health systems to be dealing with one respiratory illness instead of two.
Should I take the influenza vaccine if I am showing symptoms of COVID-19, or if I have COVID-19?
There are no known medical contraindications to vaccinating persons who have COVID-19. However, to minimize risk of COVID-19 transmission when taking the vaccine, individuals with suspected or confirmed COVID-19 should be isolated and cared for until they are no longer infectious since the act of seeking immunization may increase the spreading of the infection to others. For that reason, these individuals should defer vaccination until they are released from isolation. Afterwards, it is advised that they take the influenza vaccine in order to decrease the possibility of severe disease from influenza.
If I wasn’t vaccinated with the influenza vaccine before, would it be safe to take the influenza vaccine during the pandemic?
Yes. There are no known medical contraindications to vaccinating persons who have COVID-19. WHO advises that high risk groups should take the influenza vaccine during the COVID-19 pandemic in order to decrease the possibility of severe respiratory illness from the cocirculating viruses this influenza season and to decrease the burden on health care systems. This advice is regardless of whether the person has been vaccinated before against influenza, since the influenza strains circulating today may be different from the ones that circulated in previous years.
What can I do if the influenza vaccine is not available where I live?
Most countries are able to provide the influenza vaccine in limited quantities only, which is why WHO advises prioritizing high risk groups, starting with health care workers and the elderly. Some countries may not have been able to procure the vaccine at all this year.
Whether you are able to find the vaccine or not, you can still decrease the chances of catching or spreading influenza by following the same public health and social measures recommended for COVID-19:
- Maintain hand hygiene through frequent hand washing with soap and water, or hand sanitizer.
- Keep a physical distance of at least one metre from others and wear a mask when that is not possible.
- Observe respiratory etiquette by coughing and sneezing into your elbow.
- Seek medical advice if you develop respiratory symptoms and especially if you fall within the high-risk category.
- Self-isolate if you get sick or self-quarantine if you have come into contact with infected individuals.
Do I need to get the influenza vaccine if I have had influenza recently?
It is still recommended to get the influenza vaccine if you have had the flu this season. You can get the flu more than once in a season because there can be more than one flu strain circulating. This means that you may not have immunity to other strains and get sick again.
I’m pregnant, is it safe to take influenza vaccination?
Yes, it is safe to take influenza vaccination when you are pregnant. When you are pregnant you are at greater risk for getting more severe disease. Influenza vaccination while you are pregnant can protect you and also your baby through the antibodies that you give them when you breastfeed.
COVID-19 and influenza Q&As
Does the influenza vaccine decrease immunity against other diseases like COVID-19?
No. The purpose of any vaccine is to train the immune system on how to respond if it encounters the real disease in the future. This training does not affect the immune system against other diseases but rather strengthens it against the target disease. This immunity may last for a short period of time or for many years depending on the type of disease and type of vaccine. The influenza vaccine is considered good for one year, after which immunity against the disease decreases.
Does the influenza vaccine protect against COVID-19?
No, because influenza and COVID-19 are two different diseases. But because both respiratory diseases can impact the health of those infected in severe ways, getting immunized against influenza can decrease the impact of this disease on someone who may already be struggling with COVID-19. It is better for patients and health systems to be dealing with one respiratory illness instead of two.
Should I take the influenza vaccine if I am showing symptoms of COVID-19, or if I have COVID-19?
There are no known medical contraindications to vaccinating persons who have COVID-19. However, to minimize risk of COVID-19 transmission when taking the vaccine, individuals with suspected or confirmed COVID-19 should be isolated and cared for until they are no longer infectious since the act of seeking immunization may increase the spreading of the infection to others. For that reason, these individuals should defer vaccination until they are released from isolation. Afterwards, it is advised that they take the influenza vaccine in order to decrease the possibility of severe disease from influenza.
How are COVID-19 and influenza viruses similar?
1. COVID-19 and influenza are both respiratory diseases.
Both viruses share similar symptoms, including cough, runny nose, sore throat, fever, headache and fatigue. People may have varying levels of illness with both COVID-19 and influenza. Some may have no symptoms, mild symptoms or severe disease. Both influenza and COVID-19 can be fatal.
2. COVID-19 and influenza spread in similar ways.
Both COVID-19 and influenza are spread by droplets and aerosols when an infected person coughs, sneezes, speaks, sings or breathes. The droplets and aerosols can land in the eyes, nose or mouth of people who are nearby -- typically within 1 metre of the infected person, but sometimes even further away. People can also get infected with both COVID-19 and influenza by touching contaminated surfaces, then touching their eyes, nose or mouth without cleaning their hands.
3. Some of the same groups have a higher risk for severe illness from COVID-19 and influenza. While all age groups can be infected with both the COVID-19 virus and influenza virus, these people are at higher risk for severe disease and death from both COVID-19 and influenza:
older adults;
people of any age with chronic medical conditions (such as chronic cardiac, pulmonary, renal, metabolic, neurologic, liver or hematologic diseases); and
people with immunosuppressive conditions (such as HIV/AIDS, patients receiving chemotherapy or steroids, or malignancy)
Healthcare workers are at high risk of getting infected by COVID-19 and at high risk of getting infected by influenza.
Pregnant people and those who have recently given birth are at high risk for experiencing severe influenza and severe COVID-19.
4. The same protective measures are effective against COVID-19 and influenza.
To protect against COVID-19 and influenza, follow these public health and social measures:
Maintain at least a 1-metre distance from others and wear a well-fitted mask when that’s not possible;
Avoid crowded and poorly ventilated places and settings;
Open windows or doors to keep rooms well ventilated;
Cough or sneeze into a bent elbow or tissue and throw the tissue into a closed bin;
Clean your hands frequently
Avoid touching your eyes, nose and mouth;
Stay home if you don’t feel well; and
Contact your medical provider if you have any of the following severe symptoms of COVID-19, including:
Shortness of breath,
Loss of appetite,
Confusion,
Persistent pain or pressure in the chest,
High temperature (above 38 °C)
Vaccination is an important part of preventing severe disease and death for both COVID-19 and influenza. Follow the advice of your local authorities on getting the influenza and COVID-19 vaccines. WHO recommends the influenza vaccine for older individuals, young children, pregnant people, people with underlying health conditions, and health workers.
COVID-19 vaccines are safe for most people 18 years and older, including those with pre-existing conditions of any kind, including auto-immune disorders. These conditions include: hypertension, diabetes, asthma, pulmonary, liver and kidney disease, as well as chronic infections that are stable and controlled.
If supplies are limited in your area, discuss your situation with your care provider if you:
Have a compromised immune system
Are pregnant or nursing your baby
Have a history of severe allergies, particularly to a vaccine (or any of the ingredients in the vaccine)
Are severely frail
People with mild symptoms of both COVID-19 and influenza can usually be cared for safely at home.
For more information about caring for someone safely at home with COVID-19, watch this episode of Science in 5.
5. There are safe and effective vaccines for both COVID-19 and influenza.
COVID-19 vaccines have been proven to protect against severe illness and death caused by COVID-19 disease. Millions of people around the world have safely received COVID-19 vaccines, and the vaccines have met rigorous standards for safety, effectiveness and quality. Getting vaccinated may also protect the people around you. If you are protected from getting COVID-19, you are less likely to infect someone else. COVID-19 vaccines do not protect against influenza.
WHO recommends vaccinations each year to prevent severe influenza disease in high-risk groups: pregnant people, individuals with underlying health conditions, older adults, health workers, and young children.
How are COVID-19 and influenza viruses different?
1. Treatments for COVID-19 and influenza are different.
The treatment options in use for COVID-19 at medical facilities include oxygen, corticosteroids, and IL6 receptor blockers for severely ill patients. Treatment for people with severe respiratory illness includes advanced respiratory support such as the use of ventilators. Several other treatment options for COVID-19 are currently in clinical trials.
Antiviral drugs for influenza can reduce severe complications and death, and they are especially important for high-risk groups. It’s important to remember that antibiotics are not effective against influenza or COVID-19 viruses.
People with mild symptoms of both diseases can usually be treated safely at home. Click here for more information about caring for someone with COVID-19 safely at home.
2. Vaccines for COVID-19 and flu are different.
Vaccines developed for COVID-19 do not protect against influenza, and similarly, the flu vaccine does not protect against COVID-19. Follow the advice of your local authorities on getting the influenza and COVID-19 vaccines.
If I have had my influenza shot, do I also need COVD-19 vaccine?
Yes. You need both vaccinations.
Can someone be infected with COVID-19 and influenza at the same time?
Yes, it is possible to catch both diseases at the same time. The most effective way to prevent hospitalization and severe COVID-19 and influenza is vaccination with both vaccines. Continue to follow prevention measures, such as maintaining at least a 1-metre distance from others, wearing a well-fitted mask when keeping your distance is not possible, avoiding crowded and poorly ventilated places and settings, opening windows and doors to keep rooms well ventilated and cleaning your hands frequently.
How can I protect myself against COVID-19 and influenza?
The most effective way to protect yourself from both influenza and severe COVID-19 is to get vaccinated with both influenza and COVID-19 vaccines.
The most effective way to prevent infection with the virus that causes COVID-19 is to get vaccinated and follow prevention measures: maintaining at least a 1-metre distance from others, wearing a well-fitted mask when keeping your distance is not possible, avoiding crowded and poorly ventilated places and settings, opening windows and doors to keep rooms well ventilated and cleaning your hands frequently.
Follow the advice of your local authorities on getting the influenza and COVID-19 vaccines.
How do I tell if I am sick with COVID-19 or influenza?
Both COVID-19 and influenza cause respiratory illness. Based on symptoms alone, you cannot tell which one you have. You can only tell through testing for the virus (e.g. PCR, RATs, RDTs, etc.).
Is there a vaccine that can protect me from both COVID-19 and influenza?
Currently no, but there is research ongoing to see if it is possible to create a combination vaccine.
If I have influenza, does it protect me from COVID-19?
No, they are different viruses so if you have influenza you generate immunity for this virus, not COVID-19



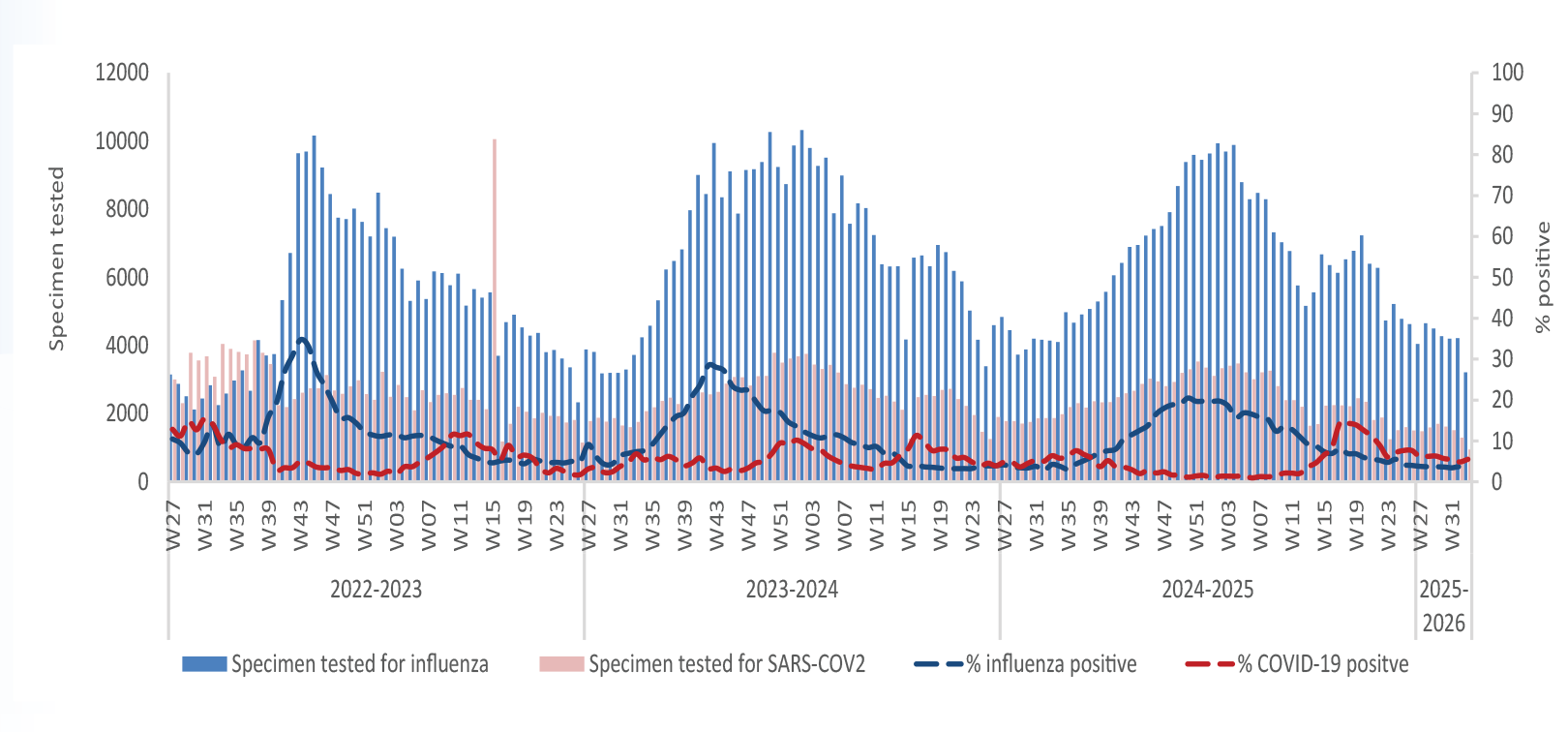
 Influenza surveillance is the collection, compilation and analysis of information on influenza activity in a defined population. This could be a country, specific population groups or a region. Data are collected over a defined period of time and reported for the purposes of monitoring influenza activity to facilitate the undertaking early actions to stop or minimize its transmission. The purpose of systematic surveillance of influenza activity is to:
Influenza surveillance is the collection, compilation and analysis of information on influenza activity in a defined population. This could be a country, specific population groups or a region. Data are collected over a defined period of time and reported for the purposes of monitoring influenza activity to facilitate the undertaking early actions to stop or minimize its transmission. The purpose of systematic surveillance of influenza activity is to: For the purposes of influenza surveillance globally, WHO uses the following case definitions for the 2 conditions that constitute influenza case definition: influenza-like illness (ILI) and severe acute respiratory infections (SARI).
For the purposes of influenza surveillance globally, WHO uses the following case definitions for the 2 conditions that constitute influenza case definition: influenza-like illness (ILI) and severe acute respiratory infections (SARI). Due to the constant evolving nature of influenza viruses, the
Due to the constant evolving nature of influenza viruses, the  The most commonly used influenza vaccines are injected inactivated influenza vaccines. These come in a trivalent (3 strains; TIV) and quadrivalent (4 strains; QIV) design. For the QIV formulation there are also high-dose versions that are primarily designed for use in people 65 years or over. There are other types of influenza vaccine; adjuvanted, live-attenuated (LAIV) and more recently recombinant influenza vaccines.
The most commonly used influenza vaccines are injected inactivated influenza vaccines. These come in a trivalent (3 strains; TIV) and quadrivalent (4 strains; QIV) design. For the QIV formulation there are also high-dose versions that are primarily designed for use in people 65 years or over. There are other types of influenza vaccine; adjuvanted, live-attenuated (LAIV) and more recently recombinant influenza vaccines. The presence of these symptoms, whether they are for influenza or for COVID-19, varies in people depending on their level of immunity. It is important to note that the prevention measures, such as washing hands, wearing masks, and maintaining physical distancing are very effective for both diseases. Both seasonal influenza and COVID-19 are preventable through following these measures.
The presence of these symptoms, whether they are for influenza or for COVID-19, varies in people depending on their level of immunity. It is important to note that the prevention measures, such as washing hands, wearing masks, and maintaining physical distancing are very effective for both diseases. Both seasonal influenza and COVID-19 are preventable through following these measures.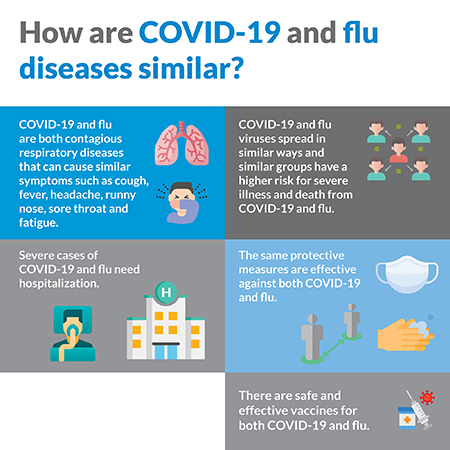 Both COVID-19 and influenza disease share similar symptoms, including cough, runny nose, sore throat, fever, headache and fatigue. People infected with either virus can have varying levels of illness; some having no symptoms, mild symptoms or severe disease. People with mild symptoms of both COVID-19 and influenza can usually be cared for safely at home. Both diseases can be fatal, with certain people at higher risk for severe disease and death.
Both COVID-19 and influenza disease share similar symptoms, including cough, runny nose, sore throat, fever, headache and fatigue. People infected with either virus can have varying levels of illness; some having no symptoms, mild symptoms or severe disease. People with mild symptoms of both COVID-19 and influenza can usually be cared for safely at home. Both diseases can be fatal, with certain people at higher risk for severe disease and death.
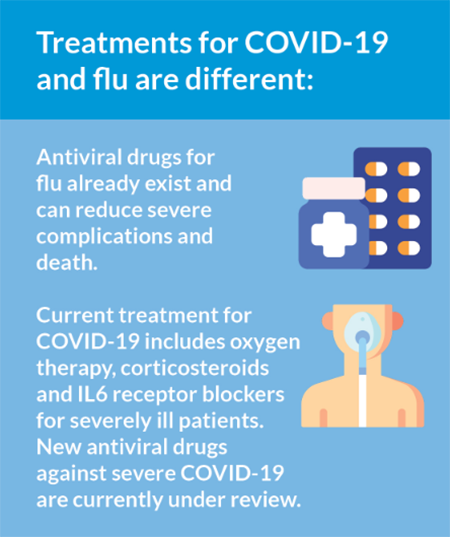 Different treatments are available for both influenza and COVID-19, but both in the initial stages are treated by addressing symptoms such as fever. Both viruses can cause severe disease, leading to hospitalization where more supportive treatment is needed such as a ventilator. For some patients, medications may help lessen the symptoms, severity and shorten the duration of COVID-19 or influenza illness.
Different treatments are available for both influenza and COVID-19, but both in the initial stages are treated by addressing symptoms such as fever. Both viruses can cause severe disease, leading to hospitalization where more supportive treatment is needed such as a ventilator. For some patients, medications may help lessen the symptoms, severity and shorten the duration of COVID-19 or influenza illness.