I. Ghaly,1 F.H. Hussein,2 S. Abdelghaffar,1 G. Anwar1 and R.M. Seirvogel3
العمر الأمثل للنضج الجنسي في الأطفال المصريين
ايزيس غالي - فوزية حسين - شيرين عبد الغفار - غادة أنور - روجر سرفوجل
الخلاصـة: تم تحديد مراحل "تانر " للنضج لمعرفة العمر الأمثل للنضج الجنسي في الأطفال المصريين، وذلك في عدد من الأطفال والمراهقين (1550 فتاة و1563 فتىً) تراوحت أعمارهم في ما بين 6.5 و18.5 عاماً. وكان العمر المتوسط لنمو شعر العانة (المرحلة الثانية) 10.46 عاماً (بانحراف معياري قدره 1.36) بالنسبة للفتيات و11.86 (بانحراف معياري قدره 1.45) بالنسبة للفتيان. أما شعر الإبط (المرحلة أ 2) فكان العمر المتوسط هو 11.65 عاماً (بانحراف معياري قدره 1.62) في الفتيات، و13.55 عاماً في الفتيان (بانحراف معياري قدره 1.52). وكان العمر المتوسط لبدء الإحاضة لدى الفتيات هو 12.44 عاماً ونمو الثديين 10.71 عاماً (المرحلة ب 2) (بانحراف معياري قدره 1.30)، كما دل حجم الخصيتين بالجس على أن العمر المتوسط للمرحلة التناسلية G2 للفتيان هو 10.56 عاماً (بانحراف معياري قدره 1.40). ومن شأن ما أسفرت عنه الدراسة من نتائج أن يساعد في تقييم النضج الجنسي واضطرابات البلوغ لدى المراهقين المصريين.
ABSTRACT: To establish the optimal age of sexual maturation in Egyptian children, Tanner’s maturity stages were determined for a sample of children and adolescents (1550 girls, 1563 boys) ranging from 6.5 to 18.5 years. The mean age for attainment of pubic hair (stage PH2) was 10.46 (SD 1.36) years for girls and 11.86 (SD 1.45) years for boys. For axillary hair (stage A2), mean age was 11.65 (SD 1.62) years for girls and 13.55 (SD 1.52) years for boys. The mean age at menarche in girls was 12.44 years and for breast development (stage B2) was 10.71 (SD 1.30) years. Testicular volume by palpation showed that the mean age of genital stage G2 for boys was 10.56 (SD 1.40) years. The study results can aid in the assessment of sexual maturation and pubertal disorders in Egyptian adolescents.
Âge optimal de la maturation sexuelle chez les enfants égyptiens
RÉSUMÉ: Afin d’établir l’âge optimal de la maturation sexuelle chez les enfants égyptiens, on a déterminé les stades de maturité de Tanner pour un échantillon d’enfants et d’adolescents (1550 filles et 1563 garçons) dont l’âge s’échelonnait entre 6 ½ ans et 18 ½ ans. L’âge moyen de l’apparition de la pilosité pubienne (stade P2) était de 10,46 (écart type 1,36) ans pour les filles et de 11,86 (écart type 1,45) ans pour les garçons. En ce qui concerne la pilosité axillaire (stade A2), l’âge moyen était de 11,65 (écart type 1,62) ans pour les filles et de 13,55 (écart type 1,52) ans pour les garçons. L’âge moyen de la ménarche chez les filles était de 12,44 ans et l’âge du développement mammaire (stade S2) était de 10,71 (écart type 1,30) ans. Le volume testiculaire à la palpation montrait que l’âge moyen du stade génital G2 pour les garçons était de 10,56 (écart type 1,40) ans. Les résultats de l’étude peuvent aider à évaluer la maturation sexuelle et les troubles pubertaires chez les adolescents égyptiens.
1Diabetic Endocrine Metabolic Paediatric Unit, Children’s Hospital, Faculty of Medicine, University of Cairo, Cairo, Egypt (Correspondence to S. Abdelghaffar:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
)
2National Research Centre, Cairo, Egypt.
3Lifespan Health Research Centre, Department of Community Health, School of Medicine, Wright State University, Ohio, United States of America.
Received: 08/02/06; accepted: 10/07/06
EMHJ, 2008, 14(6):1391-1399
Introduction
Previous studies have clearly demonstrated the influence of genetic as well as environmental factors on pubertal development; these can be explained to some degree by the effect of socioeconomic level as well as the extent of physical activity [1,2].
A secular trend in the age of sexual maturation has been observed in many industrialized countries [1,3]. The age of onset of puberty has decreased dramatically over the past 150 years, at a rate of 2–3 months per decade. This has been attributed to a decline in the incidence of infectious diseases and improvements in health care, vaccination programmes, socioeconomic conditions and nutrition [4]. Racial differences across nations and even in the same country have been reported [5–8]. Therefore, the use of standards for sexual maturation from other countries is not useful. On the other hand, studies of sexual maturation in Egypt are scarce and inadequate. The aim of this study was to obtain data about the optimal age of sexual maturity in Egyptian children and adolescents, data which could be considered as a baseline for assessment of different pubertal disorders.
Methods
Sample
A total of 1563 boys and 1550 girls were assessed for sexual maturation as part of a much larger cross-sectional study to establish standard growth curves for Egyptian infants, children and adolescents. The ages of the children in this substudy ranged from 6.5 to 18.5 years. The duration of the study was from July 1997 to December 2001.
Ideally, national growth curves would be based on a representative sample of children from every governorate of Egypt. However, the great majority of Egyptians live in the Nile valley, where a geographical gradient is assumed to exist in the genetic composition of Egyptians. Moreover, the inhabitants of Cairo, the capital city, amount to one-fifth of the Egyptian population, and many are migrants from areas throughout Egypt. For these reasons, the sample was chosen from the population of Cairo.
To establish standard growth curves from which comparisons to the norm can be made it was necessary to obtain data from children with optimum growth opportunities. Therefore, the sample for this study was restricted to children from upper and middle socioeconomic groups attending fee-paying schools, who could be presumed to experience optimum conditions for growth and maturation. Inclusion criteria were normal healthy children whose mothers had a normal delivery of a normal-birth-weight baby after a normal pregnancy. Exclusion criteria included major genetic or organic diseases known to cause deviation from normal growth patterns. All schools and children fitting the inclusion criteria were included. Only non-qualifying subjects or those who refused were excluded.
Data collection
Ethical consent
Approval of the concerned authorities was obtained. Explanatory meetings by the principal investigator of the project and board members were held with parents, school headmasters and physicians. Schools were approached by formal letters and personal interviews. Orientation was performed about the project and its importance, and informed consent was obtained from all participating parents as well as participating adolescents. Interviews and examinations took place at schools with the help of the school administration who offered the location and facilities.
Training and quality control
The team members included 54 highly trained personnel, 41 of whom were physicians. Each team comprised 1 supervisor, 3 practitioners, 1 social worker and 1 assistant. Each team received 20 hours of classroom instructions over a 10-day period plus practical training for 4 hours per day for 2 weeks. This training was provided by the coinvestigators from the Diabetes Endocrine Metabolic Paediatric Unit, Children’s Hospital, University of Cairo and the Anthropology and Child Health Department, National Research Centre, Cairo.
Each team member was responsible for specific tasks associated with data collection. The supervisor monitored the accuracy of the measurements that were performed, reviewed the pooled sheets, excluded non-qualifying subjects and replaced them with qualifying ones of appropriate sex and age group. Two physicians assigned to each team acquired the clinical history and performed the physical examination, anthropometric measurements and pubertal assessment. A social worker completed the family and social data questionnaires. Finally, an assistant dressed and undressed the children, and helped the practitioners to perform the measurements. The accuracy of each team’s measurements was evaluated during the training course and during the field study by their respective supervisors.
Protocol
For each child, the parents completed a questionnaire about the child’s personal and social data as well as previous medical history. A complete clinical examination as well as anthropometric measurements and pubertal examination were performed, the latter was done for boys and girls 6 years or older by male and female physicians respectively. During the survey fieldwork, the actual assessments were done during a general physical examination, after obtaining consent from the parents.
Assessment of sexual maturity
Pubertal evaluation of the secondary sexual characteristics of both sexes was done by inspection, and classified by Tanner stages (Table 1) [9,10]. Maturity stages were assigned to breast development in females and pubic and axillary hair in males and females. Five Tanner stages were defined for pubic hair and breast development, examined accurately by both inspection and palpation by female physicians. Direct questioning of the girl was used to record the attainment of menarche at the time of examination. For males, in addition to assessment of pubic and axillary hair, left and right testicular volume was recorded by palpation of the testes using a Prader orchidometer. This examination was done by male physicians, well-trained in anthropometry and pubertal evaluation. A testicular volume of 4 mL of the larger testis represented the first clear sign of the onset of puberty (genital stage G2), volume 8 mL was G3, volume 12 mL G4 and volume 15–25 mL was G5; the latter was considered as the last pubertal event reached by all normal boys, as previously established [10].
Statistical analysis
Descriptive statistics for age by sex and Tanner stage were computed separately for male and female pubic and axillary hair, female breast development and male testicular size. One-way analysis of variance (ANOVA) was used to test for any overall significant differences among mean ages of the Tanner stages within each sex.
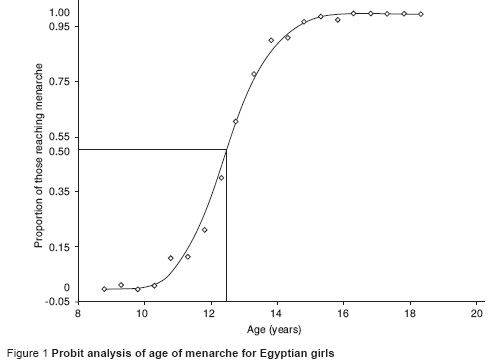
For menarche data, female subjects were divided into 24 age groups ranging from 6.5 to 18.5 years of age. Groups were created in half-year intervals from 6.5 to 7.0 years up to 18.5 years of age. The midpoint of each age group was used as the reference value for that group. For instance, in the 6.5 to 7.0 year age group, 6.75 years was used as the reference value. The proportion of those females obtaining menarche was calculated within each age group. A probit analysis was then completed and the average age at menarche obtained. The empirical proportions were plotted and a function of the natural log was used to model the proportion of those who had obtained menarche.
All tests were run using SAS, version 6.12 [11], procedure PROC GLM, assuming a type-1 error rate of 0.05.
Results
Table 2 shows the ages at attainment of male and female axillary and pubic hair as well as female breast development. The mean age for attainment of pubic hair (stage PH2), was 10.46 [standard deviation (SD) 1.36] years for girls and 11.86 (SD 1.45) years for boys. For axillary hair (stage A2), the mean age was 11.65 (SD 1.62) years for girls and 13.55 (SD 1.52) years for boys. The mean age at the lowest maturity level of pubic hair was the same for both males and females (8.65 and 8.64 years respectively), but for the highest maturity level it was 15.76 years for males and 14.72 years in females respectively. The mean age upon reaching adult maturity for pubic and axillary hair was about 1 year earlier in females than in males.
The results for breast development in girls show that the mean age for the attainment of stage B2 was 10.71 (SD 1.30) years, range 8.11–14.23 years. Stage B3 occurred as early as 7.56 years.
Figure 1 shows the probit plot for age at menarche of girls. The point at which 50% of the girls reported achieving menarche, i.e. the average age at menarche, was 12.44 years.
The first sign of breast development (stage B2) occurred about 1.7 years before menarche, for pubic hair (stage PH2) about 2 years before menarche, while for axillary hair it was 0.79 years before menarche.
Table 3 shows mean ages for each of the 12 testicular sizes measured by palpation. Testicular volume by palpation showed that the mean age of testicular stage T4 (i.e genital stage G2) was 10.56 (SD 1.40) years. The duration of male puberty from the beginning of testicular enlargement to testicular stage T15 (i.e. G5) was about 4 years.
Discussion
The study presents the sexual maturity stages of 3113 Egyptian students (1550 girls and 1563 boys).
For girls, the mean age for the attainment of breast development stage B2 was 10.71 years. Of interest is the observation that the minimum age for stage B3 was 7.56 years, indicating that the onset of puberty in this sample of girls occurred as early as 7 years. Age at menarche is a more reliable event for determining sexual maturity in girls than the appearance of secondary sexual characteristics [12–14]. In our study, the average age at menarche was 12.44 years, which is lower than another study in Egypt in 1978 that reported the mean menarcheal age in Egyptian girls was 12.59 years among girls of high social class and 13.89 years in the low social class [15]. Another cross-sectional study in 1984 ascertained the morphological, metric and developmental norms of Egyptian children [16]. The sample comprised 591 schoolgirls, drawn mainly from the middle and low social classes with ages ranging from 9 to 18 years. The mean menarcheal age was 13.24 years, which is 9 months older than in the present study. The difference in menarcheal age between these 2 studies and ours cannot be explained by the occurrence of secular trends over the past 18 years because of the difference in social class. It has been previously shown that a relatively large difference exists (1.3 years) between the mean menarcheal age of high and low social classes [15].
For boys, the mean age of start of puberty was 10.56 years and the duration of male puberty from the beginning of testicular enlargement to stage T15 was about 4 years. Comparison with other studies worldwide demonstrates the effect of genetic factors and environment in different geographical regions and intrauterine growth on start and progression of sexual maturation [17]. In the Netherlands, Fredriks et al. showed that the start of puberty T4 occurred at 11.5 years [5], later than our Egyptian boys. In the United States of America, the onset of pubic hair growth occurred at a mean age of 12.0, 11.2 and 12.3 years for white, African–American and Mexican–American boys respectively [18]. The data indicated significant differences in these 3 racial ethnic groups in the age at onset of sexual maturation. Compared with these data, Egyptian boys started pubic hair development earlier than white Americans and Mexican–Americans, but later than African–American boys. For testicular development (stage T4), it started at a mean age of 10.56 years in Egyptian boys, later than white American and African–American, but at a similar age to Mexican–American boys. On the other hand, Egyptian boys completed their genital development earlier than American boys. However, it is worth mentioning that comparison of genital development with other studies across nations is difficult because of the different methods used for clinical assessment of pubertal development: photography [10], genital development by inspection [18], self-assessment [19], the use of biological maturation and peak height velocity (PHV) skeletal age [20].
The aim of the present study was to report on the optimal age of sexual maturation in Egyptian adolescents. For that reason, subjects were recruited from the middle and high social classes. The strengths of the study include the adequate sample size, the adequate age range from 6.5 to 18.5 years, which can detect the early stages of sexual maturation, and the accuracy of physical examination by well-trained physicians with estimation of testicular volume by palpation. The results may aid in the diagnosis of pubertal disorders in Egyptian adolescents.
Future studies should aim to discover if there is a secular trend in sexual maturation in Egyptian children, as has already been observed in many industrialized countries. This trend has been attributed to improvements in health care, decreasing incidence of infectious diseases, vaccination programmes, better socioeconomic conditions and improved nutrition [21–23].
Acknowledgements
The team of this project acknowledges the comprehensive and continuous support received from the Supreme Council of Universities and the Foreign Relations Coordination Unit and the help provided by international consultants Mendez England and Associates over all phases of the project. The funding and support received from the USAID programme to realize this project is highly appreciated. The project team would like to express its deepest gratitude to the Egyptian Minister of Education and to all the schools, nurseries, hospitals, infants, children, adolescents and parents who contributed in the implementation of this national project.
The following persons and institutions participated in the national Egyptian growth: curves study: N. Salah, M. Hafez, M. Atteya, M. Mamdouh, A. Hamed, S. Mansour (Cairo University, Faculty of Medicine, Diabetes Endocrine Metabolic Pediatric Unit); M. Erfan, M.O. El Ruby, I. Mazen, S. Abdel Dayem, N.E. Hassan S. Ismail, L.A. Hosny, N. Ibrahim, R. Bassiouni, M.S. Zaki,M.S. Aglan, E.R. Abdel Raouf, S.A. El Masry, W.A. Kandeel, M.A. El Gammal, A.M. Ahmad, M. Fawzi, A. Moussa, T.F. El Shaer, S.G. Abanob (National Research Centre, Cairo Egypt); S. Bakeer, A. Zekry Sobhy, A. Amin, I. Fekry, N. Gohar, A. Kamal, A. Abdel Monem, A. El Sayed, H. Gaber, E. Abdel Kader (Ministry of Health, Cairo, Egypt); C.M. Schubert, V. Wentling, S.S. Guo, C. Chumlea (Lifespan Health Research Center, Department of Community Health, School of Medicine, Wright State University, Ohio, United States of America.
References
- Plamert MR, Boepple PA. Variation in the timing of puberty: clinical spectrum and genetic investigation. Journal of clinical endocrinology and metabolism, 2001, 86:2364–8.
- Kalberg J. Secular trends in pubertal development. Hormone research, 2002, 57(Suppl. 2):19–30.
- Vizmanos B et al. Age of pubertal onset affects the intensity and duration of pubertal growth peak but not final height. American journal of human biology, 2001, 13:409–16.
- Davidson KK, Susman EJ, Birch LL. Percent body fat at age 5 predicts earlier pubertal development among girls at age 5. Pediatrics, 2003, 111(4):815–21.
- Fredriks AM et al. Continuing positive secular growth change in the Netherlands 1955–1997. Pediatric research, 2000, 47:316–23.
- Rosenfield RTL, Bachrach LK, Chernausek SD. Current age of onset of puberty. Pediatrics, 2000, 106:622–3.
- Anderson SE, Dallal GE, Must A. Relative weight and race influence. Average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart. Pediatrics, 2003, 111(4):844–50.
- Herman-Giddens ME, Kaplowitz PB, Wasserman R. Navigating the recent articles on girls’ puberty in pediatrics. What do we know and where do we go from here? Pediatrics, 2004, 113(4):911–7.
- Tanner JM. Growth at adolescence. Oxford, Blackwell Scientific Publications, 1962.
- Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in girls. Archives of disease in childhood, 1969, 44:291–303.
- SAS/STAT user’s guide, version 8, 4th ed. Carey, North Carolina, SAS Institute Inc., 1999.
- Herman-Giddens ME et al. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings network. Pediatrics, 1997, 99:505–12.
- Parent A-S et al. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocrine reviews, 2003, 24(5):668–93.
- Cameron N. Assessment of growth and maturation during adolescence. Hormone research, 1993, 39(Suppl. 3):9–17.
- Attalah NL. Age at menarche in school girls in Egypt. Annals of human biology, 1978, 5:185–9.
- Hussein FH et al. Age at menarche in Egyptians. In: Borms J, et al., eds. Human growth and development. New York, Plenum Press, 1984.
- Ibanez L et al. Early puberty: rapid progression and reduced final height in girls with low birth weight. Pediatrics, 2000, 106(5):72–7.
- Herman-Giddens ME, Wang L, Koch G. Secondary sexual characteristics in boys. Estimates from the National Health and Nutrition Examination Survey III, 1988–1994. Archives of pediatrics & adolescent medicine, 2001, 155:1022–8.
- Duke PM, Litt IF, Gross RT. Adolescents’ self-assessment of sexual maturation. Pediatrics, 1980, 66(6):918–20.
- Lee PA, Kulin HE, Guo SS. Age of puberty among girls and the diagnosis of precocious puberty. Pediatrics, 2001, 107(6):1493.
- De Muinich SM, Mul D. Trends in pubertal development in Europe. Human reproduction update, 2001, 7:287–91.
- Liu YX, Albertsson-Wikland K, Karlberg J. New reference for the age at childhood onset of growth and secular trend in the timing of puberty in Swedish. Acta paediatrica, 2000, 89:637–43.
- He Q, Karlberg J. BMI in childhood and its association with height gain, timing of puberty, and final height. Pediatric research, 2001, 49:244–51.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)