M.E. Razavi,1 R.B. Abotoraby,2 R.D. Kakhki,1 S.Z. Ghanavati,1 P. Layegh,2 M. Taghavi2 and M.T. Rajabian2
التقيـيم السريري لاعتلال العين في داء غريفز في شمال شرق جمهورية إيران الإسلامية
محمد اعتضاد رضوي، رباب أبو ترابي، رامين دانشور كاخكي، سيامك زارعي قنواتي، بروين لايق، مرتضى تقوى، رضا رجبيان
الخلاصـة: تقيِّم هذه الدراسة معدل انتشار ووخامة التظاهرات العينية في داء غريفز لدى 68 مريضاً ممن راجعوا عيادات الغدد الصماء في جامعة مشهد للعلوم الطبية في المدة من كانون الأول/ديسمبر 2002 إلى أيلول/سبتمبر 2005. وقد كان العمر الوسطي للمرضى 38 عاماً (الانحراف المعياري: 14.0 عاماً والمجال: 15 - 71 عاماً). وكانت الشكوى الأكثر شيوعاً هي الإحساس بوجود جسم غريب (54.0%) وانتفاخ الأجفان (48.4%) أما الاضطراب الأكثر شيوعاً ووضوحاً فكان انكماش الجفن لدى 64.2% من المرضى (ثنائي الجانب في 95.3% منهــم). وقـد كـان لـدى المرضى درجـات أحـراز متوسطـة وفـق تصنيف ويرنـر لاعتـلال العيـن في داء غريفــر (NO SPECS) وقد بلغت 3.00 (بانحراف معياري مقداره 1.46). وقد كانت الدرجـات الـمحرزة لدى الذكور [3.58 (بانحراف معياري 1.44)] أعلى بشكل يعتد به إحصائياً مما هو عليه لدى الإناث [2.63 (بانحراف معياري مقداره 1.35)]، وكانت أيضاً مترابطة ترابطاً إيجابياً مع العمر.
ABSTRACT: This study evaluated the prevalence and severity of ophthalmic manifestations in all Graves disease patients (n = 68) presenting to endocrine clinics at Mashad University of Medical Sciences between December 2002 and September 2005. The mean age of patients was 38.0 (SD 14.0) years, range 15 to 71 years. The most common complaints were foreign body sensation (54.0%) and puffy eyelids (48.4%). The most common apparent abnormality was lid retraction in 64.2% of patients (bilateral in 95.3% of cases). The patients had a mean modified Werner’s NO SPECS classification score of 3.00 (SD 1.46). The score was significantly higher in males than females [3.58 (SD 1.44) versus 2.63 (SD 1.35)] and was positively correlated with age.
Évaluation clinique de l’ophtalmopathie basedowienne dans le nord-est de la République islamique d’Iran
RÉSUMÉ: Cette étude a évalué la prévalence et la gravité des manifestations ophtalmologiques chez les patients atteints de la maladie de Graves-Basedow (n = 68) qui se sont présentés au service de consultations externes d’endocrinologie de l’Université des Sciences médicales de Mashad entre décembre 2002 et septembre 2005. L’âge moyen de ces patients était de 38,0 (écart type 14,0) ans, avec des extrêmes de 15 et 71 ans. Les sujets se plaignaient le plus souvent de sensation de corps étranger (54,0 %) et de gonflement des paupières (48,4 %). L’anomalie apparente la plus courante était la rétraction palpébrale chez 64,2 % des patients (bilatérale dans 95,3 % des cas). Les patients avaient un score moyen de 3,00 selon la classification NOSPECS de Werner modifiée (écart type 1,46). Ce score était significativement plus élevé chez les hommes que chez les femmes (3,58 [écart type 1,44] contre 2,63 [écart type 1,35]) et positivement corrélé à l’âge.
1Department of Ophthalmology, Khatam-Al-Anbia Eye Hospital; 2Department of Endocrinology, Ghaem Hospital, Medical University of Mashad, Mashad, Islamic Republic of Iran (Correspondence to M.E. Razavi:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
Received: 16/02/06; accepted: 10/04/06
EMHJ, 2008, 14(4):841-849
Introduction
The relationship between exophthalmos and thyroid disease was first recognized by the Iranian scientist Sayyid Ismail Al-Jurjani in the 12th century [1,2]. Graves ophthalmopathy (GO) is a chronic, debilitating infiltrative eye and orbital disease that is often associated with Graves disease. About 50% of patients with Graves disease will develop GO and severe forms affect 3% to 5% of patients. The onset of the ophthalmopathy is in most cases concomitant with the onset of hyperthyroidism, but eye disease may precede or follow hyperthyroidism [3]. GO was found to affect females 6 times more frequently than males (86% versus 14% of cases, respectively), but the female:male ratio was reduced to 4:1 in severe forms of eye disease [4]. The age-adjusted incidence was 16 cases per 100 000 population per year for females and 2.9 cases per 100 000 population per year for males. The peak incidence rates were bimodal, occurring in age groups 40–44 years and 60–64 years in females and 45–49 years and 65–69 years in males [5].
The ocular changes associated with thyroid dysfunction have been recognized for many years, yet controversy remains regarding the pathogenesis, pathophysio-logy, and management of this disease [6,7]. Newer studies have brought possible significant insights to the understanding of the pathogenesis of GO. It has been found that thyroid-stimulating hormone (TSH)-receptors are also present in retrobulbar tissue [8,9], which is why it is suspected that TSH-receptor antibodies contribute to the development of GO by the stimulation of these retro-orbital tissue TSH-receptors.
General health-related quality of life is markedly impaired in patients with GO, and could be even worse than in patients with other chronic conditions such as diabetes, emphysema or heart failure [10]. In addition, severe forms of GO can lead to sight-threatening complications. Evaluation of the epide-miologic characteristics and severity of GO in each region can help to inform better decisions about increased quality of life and adequacy of education and counselling in patients with GO.
There have been few studies to evaluate the prevalence and severity of GO in Iranian patients [11]. Due to this lack of data, we aimed to investigate the prevalence and severity of ophthalmopathy in Graves patients in our area (north-east of the Islamic Republic of Iran). We therefore examined a large number of patients with Graves disease for the prevalence of GO, as well as the influence of various factors, such as age, sex and thyroid status, on the severity of ophthalmopathy. In addition, the clinical presentation of our patients was compared and contrasted with that of previously reported studies.
Methods
This was a multi-centre, prospective, descriptive study between December 2002 and September 2005. All patients with confirmed diagnosis of Graves disease attending the endocrine clinics of the Mashad University of Medical Sciences during the study period were recruited to the study. The diagnosis of Graves disease was based on clinical and laboratory findings of diffuse enlargement of thyroid gland, free triiodothyronine (T3) and thyroxine (T4) levels, T3 resin uptake, raised free T4 or T3 levels, suppressed TSH levels. The study had no exclusion criteria and all patients with documented history of hyperthyroidism with any age, onset or type of intervention were included.
Information about age, occupation, family history, ocular symptoms and associated systemic diseases was obtained. The records of patients were reviewed to evaluate the recent thyroid disease status and the treatment regimen.
A comprehensive ophthalmic examina-tion was performed in a standardized way for all patients. Best corrected visual acuity was documented by Snellen chart. A visual field test was requested in any case suspec-ted of optic nerve dysfunction.
Intraocular pressure (IOP) was measured by applanation tonometer in the primary position and with upward gaze. Eyelid, conjunctiva and ocular motility status were assessed. Tear status was evaluated with Shirmer test and tear break-up time. We considered Schirmer 2 mm. Corneal involvement was assessed with fluorescein staining under slit lamp biomicroscopy. Fundus examination was done for evaluation of disc and retina. Also computed tomography (CT) or magnetic resonance imaging (MRI) was taken when required.
The classification of GO was based on Werner’s classification, as endorsed by the American Thyroid Association [12] (Table 1). The relation of the thyroid functions and ocular manifestations were also evaluated.
Results
A total of 68 patients were studied during the period December 2002 to September 2005: 24 men (36%) and 43 women (64%) (data missing for 1 patient). The mean age of the patients was 38.0 [standard deviation (SD) 14.0] years (range 15 to 71 years). The mean age for females was 34.8 (SD 13.3) years and for males 44.3 (SD 13.4) years.
The mean duration of systemic thyroid disease was 2.5 (SD 2.4) years (range 6 months to 11 years). The majority of patients had hyperthyroidism at the initial pre-sentation to the ophthalmologist (86.2%); only 3% of patients were hypothyroid and the remainder were euthyroid. While 76.7% of patients were receiving methimazole, 11.7% of patients were under treatment with levothyroxine. A history of radioactive iodine treatment was present in 23.3% of patients.
The most common presenting comp-laints of patients were foreign body sensa-tion (54.0%) and puffy eyelids (48.4%). Ocular and periocular pain was the complaint in 45.2% of patients and the eyeball was the most prominent site of pain in the majority (78.5%). Other symptoms included: tearing (40.3%), photophobia (35.5%), staring (31.7%), blurred vision (29.0%) and diplopia (17.7%).
Mean Snellen visual acuity was 0.90 (SD 0.17). The most prevalent sign was increased intraocular pressure on upgaze (88.2%), which was clinically significant (≥ 5 mmHg) in 13.2% of patients. The mean intraocular pressure in the primary position was 15.90 (SD 3.56) mmHg, which inc-reased to 18.76 (SD 4.57) mmHg on up-gaze. The increment in intraocular pressure on upgaze was statistically significant (P < 0.0001).
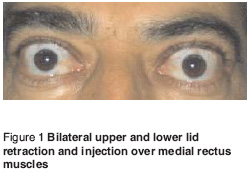
The most common apparent abnormality was lid retraction, which was noticed in 64.2% of patients (Table 2). Lid retraction was bilateral in 95.3% of cases. Exophthalmos was present in 53.0% of patients and was bilateral in the majority of cases (85.6%). Injection over the insertion of horizontal recti was noticed in 48.5% of patients, which was more prominent over the insertion of medial rectus (Figure 1). Limited ocular movements were present in 19.1% of patients. Most of the patients had limitation on upgaze and abduction (16.2%), and unexpectedly the downgaze was the least limited gaze (5.9%).
Tear break-up time had a mean of 11.61 (3.46) seconds (range 4–20 seconds). It was abnormal in 55.9% of patients (< 5 seconds in 1.5% and 5–10 seconds in 54.4% of patients). With a mean of 17.76 (SD 6.18) mm (range 4–30 mm), the Schirmer test was abnormal in 10.3% of patients. Increased IOP on upgaze had a statistically significant correlation with limitation of extraocular movements (4.57 mmHg versus 2.56 mmHg in the presence and absence of gaze limitation, respectively; P = 0.03). Also, a clinically significant increase in IOP was more common in patients with limited gaze (P = 0.01).
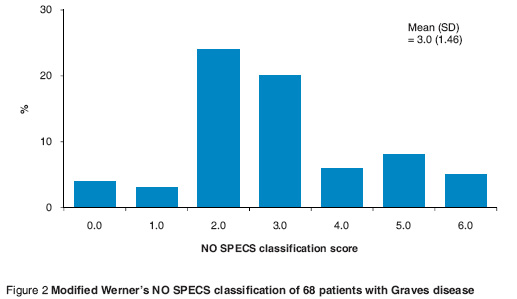
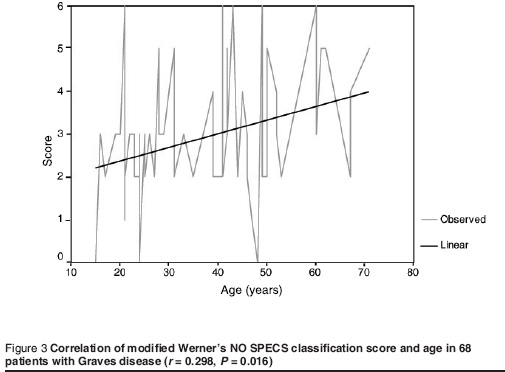
The patients had a mean modified Werner’s NO SPECS classification score of 3.00 (SD 1.46) (Figure 2). The mean score was significantly higher in males [3.58 (SD 1.44)] than females [2.63 (SD 1.35)] (P < 0.01). The score was positively correlated with the age of the patient (r = 0.298, P = 0.016) (Figure 3). A correlation between the score and disease duration or TSH level could not be shown.
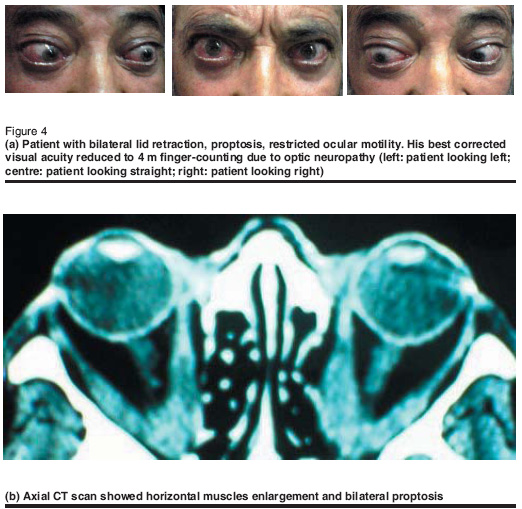
Clinically detectable optic neuropathy was found in 1 of our patients (Figure 4 a - b). This patient had the complete constellation of classic findings at the same time: eyelid retraction, exophthalmos, optic nerve dysfunction, extraocular muscle involvement, and hyperthyroidism. Visual impairment (visual acuity and visual field changes) was the main symptom of optic neuropathy.
Discussion
Our study, conducted with a relatively large number of patients, can be compared with other similar studies. GO was found to be more common among women. However, in other studies the female: male ratio was between 4:1 and 6:1 [5,13,14], whereas in our sample it was less than 2:1 (64% of cases were females versus 36% males). On average, females presented 10 years earlier than males; the mean age of females in our study was 34.8 years and for males 44.3 years. As the majority of affected patients were middle-aged women, the importance of the functional and cosmetic consequen-ces should be considered in the context of early diagnosis and treatment.
The most common complaints of our pa-tients were foreign body sensation (54.0%) and puffy eyelids (48.4%), followed by ocular and periocular pain (45.2%), tearing (40.3%), photophobia (35.5%), staring (31.7%), blurred vision (29.0%) and diplopia (17.7%).
The most common ocular signs among patients with thyroid ophthalmopathy in this study were increased IOP on upgaze (88.2%), lid retraction (64.2%), exophthalmos (53%) and periorbital swelling (50.0%). The rate of lid retraction in our study was lower than the rates reported by Bartley et al. [5] (90.0%), Vangheluwe et al. [15] (90.0%), and Teshome and Seyoum [16] (83.8%).
Strabismus is common in GO and usual-ly presents in the hypotropic or esotropic forms. In our study, 13.3% of patients had strabismus, the majority of whom had hypotropia or esotropia.
The prevalence of restrictive myopathy in the studies by Vangheluwe et al. [15] and Bartley et al. [5] were 40% and 43% respectively. In our study, the prevalence of extraocular muscle involvement with limited gaze was 19.1%, whereas frank strabismus was noted in only 13.3%.
Clinically detectable optic neuropathy was found in 1 of our patients. Visual impairment (visual acuity and visual field changes) was the main symptom. However, other methods used to detect optic neuropathy are more sensitive than vision tests alone and also take into consideration early forms of optic nerve damage [17]. Using visual evoked cortical potentials, Salvi et al. found signs indicative of optic neuropathy in 21 out of 88 patients (23.8%) [18]. Considering the high prevalence of optic neuropathy found by these authors, it is surprising that clinically significant optic neuropathy (with visual deterioration) was much rarer in our patients. However, the diagnosis of optic neuropathy in our patients was by clinical examination only, based on visual deterioration and visual field defects. More sensitive methods were not available and therefore the actual occurrence of optic neuropathy is probably underestimated.
GO is frequently associated with eleva-ted IOP on upgaze. In this study, 88.2% of patients had abnormal IOP on upgaze which was ≥ a 5 mmHg rise in 13.2%. This finding is similar to those of Gamblin et al. [19]. Increased IOP on upgaze had a significant correlation with limitation of extraocular movements (4.57 mmHg versus 2.56 mmHg in the presence and absence of gaze limitation respectively; P = 0.03). However, the usefulness of measuring IOP change on upgaze in clinical practice remains controversial. In Reader’s study on 100 healthy eyes, the mean increase in IOP at 20 degree upgaze was 1.75 (SD 1.49) mmHg [20]. A total of 5 patients had an increase in IOP of 4 mmHg and 1 patient had a 6 mmHg increase. Therefore, the pressure elevation has to be interpreted very carefully.
Similar to Perros et al.’s study [13], age and sex influenced the severity of thyroid-associated ophthalmopathy. In our cases the score was significantly higher in males than females (3.58 versus 2.63 respectively; P < 0.01) and was positively correlated with the patients’ age (r = 0.298, P = 0.016). Although we included the patients’ smoking history in our study, the number of smokers was small and a definitive conclusion regarding the relation between smoking and thyroid eye disease could not be made from this study.
Marcocci et al. showed no clear rela-tionship between treatment of hyperthy-roidism and the course of ophthalmopathy [21]. Antithyroid drugs may improve ocular manifestations, whereas prescription of radioactive iodine and thyroidectomy cause worsening of ophthalmopathy. In our cases while 76.7% were receiving methimazole, 11.7% of patients were under treatment with levothyroxine. A history of radioactive iodine treatment was present in 23.3% of patients. The majority of patients had hyperthyroidism at the time of first presentation (86.2%), 3% of patients had a hypothyroidic state and the remainder were euthyroid. These interventions may change the course of ophthalmopathy in our patients.
Conclusion
The epidemiological characteristics and clinical course of ophthalmopathy in Graves disease has been the subject of many studies. Our study of a relatively large patient sample revealed the known epidemiological facts regarding Graves ophthalmopathy in north-east of Islamic Republic of Iran. Our results correspond with numerous other studies with slight epidemiological variations. The prevalence of most of the ocular complications increased with increasing age. The incidence of higher severity score of ophthalmopathy was significantly greater among older patients.
Acknowledgements
This study was supported by grant number 82061 awarded by the Research Committee of Mashad University of Medical Sciences.
References
- Rolleston HD. The endocrine organs in health and disease, with an historical review. London, Oxford University Press, 1936.
- Netland PA. Dallow KL. Thyroid ophthal-mopathy. In: Albert DM, Jakobiec FA, editors. Principles and practice of ophthal-mology. Volume 5. Philadelphia, WB Saunders Company, 1994:2937–51.
- Coday MP, Netland PA, Dallow LD. Thyroid-associated ophthalmopathy (Graves’ disease). In: Albert DM et al., eds. Principles and practice of ophthalmology, 2nd ed. Philadelphia, WB Saunders, 2000:4742–59.
- Wiersinga WM, Bartalena L. Epidemio-logy and prevention of Graves’ ophthal-mopathy. Thyroid, 2002, 12:855–60.
- Bartley GB. The epidemiologic cha-racteristics and clinical course of ophthal-mopathy associated with autoimmune thyroid disease in Olmsted Country, Minnesota. Transactions of the American Ophthalmology Society, 1994, 92:477–588.
- Waldhausen JH. Controversies related to the medical and surgical management of hyperthyroidism in children. Seminars in pediatric surgery, 1997, 6:121–7.
- Barrie WE. Graves’ ophthalmopathy. Western journal of medicine, 1993, 158:591–5.
- Major BJ, Cures A, Frauman AG. The full length and splice variant thyrotropin receptor is expressed exclusively in skeletal muscle of extraocular origin: a link to the pathogenesis of Graves’ ophthalmopathy. Biochemical and biophysical research communications, 1997, 230:493–6.
- Heufelder AE. Involvement of the orbital fibroblast and TSH receptor in the pathogenesis of Graves’ ophthalmopathy. Thyroid, 1995, 5:331–40.
- Wiersinga WM, Prummel MF, Terwee CB. Effects of Graves’ ophthalmopathy on quality of life. Journal of endocrinological investigation, 2004, 27(3):259–64.
- Besharati MR, Rastegar A. Clinical study of ophthalmopathy in patients with Graves’ disease. Asian journal of ophthalmology, 2005, 7:108–12.
- Werner SC. Classification of the eye changes of Graves’ disease. Journal of clinical endocrinology and metabolism, 1969, 29:982–4.
- Perros P et al. Age and gender influence the severity of thyroid-associated ophthalmopathy: a study of 101 patients attending a combined thyroid eye clinic. Clinical endocrinology, 1993, 38:367–72.
- Noth D et al. Graves’ ophthalmopathy: natural history and treatment outcomes. Swiss medical weekly, 2001, 131:603–9.
- Vangheluwe O et al. Prevalence de l’ophtalmopathie au cours de la maladie de Basedow. A propos d’une etude prospective portant sur 85 cas [Preva-lence of eye diseases in Basedow diseases. Apropos of a prospective study with 85 cases]. Journal francais d’ophtalmologie, 1992, 15:469–73.
- Teshome T, Seyoum B. Graves’ thyroid ophthalmopathy in Ethiopian patients. Ethiopian medical journal, 2001, 39:1–8.
- Neigel JM et al. Dysthyroid optic neuropathy. The crowded orbital apex syndrome. Ophthalmology, 1988, 95:1515–21.
- Salvi M et al. The study of visual evoked potentials in patients with thyroid-associated ophthalmopathy identifies asymptomatic optic nerve involvement. Journal of clinical endocrinology and metabolism, 1997, 82:1027–30.
- Gamblin GT et al. Prevalence of increased intraocular pressure in Graves’ disease—evidence of frequent subclinical ophthalmopathy. New England journal of medicine, 1983, 308(8):420–4.
- Reader AL. Normal variations of intraocular pressure on vertical gaze. Ophthalmology, 1982, 89:1084–7.
- Marcocci C et al. Relationship between Graves’ ophthalmopathy and type of treatment of Graves’ hyperthyroidism. Thyroid, 1992, 2:171–8.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)