Research article
S.A. Ibrahim,1 M.A. Samy,1 M.K. Matter 1 and A.O.L. Saleh1
كثافة المعادن في العظام بين المصريين القصار القامة من المراهقين والبالغين: نتائج المسح الوطني
سحر علي إبراهيم حمودة، مايسة أحمد سامي، مي كامل مطر، عزة عمر صلاح
الخلاصة: لا يُعرف سوى القليل حول الكتلة العظمية في المراهقين القصار القامة الذين لم يحققوا النمو المُعتاد من حيث الطول. وقد أُجريَ مسحٌ وطني لكثافة المعادن في العظام بين المراهقين والبالغين القصار القامة. واختيرت عينة عشوائية متعددة الشرائح 2500 أسرة (8476 من المراهقين وآبائهم) تم انتقاؤهم من ست محافظات من مختلف المناطق الجغرافية في مصر. وتمَّ جمع السوابق السريرية، والقياسات البشرية، وقياس كثافة المعادن في العظام باستخدام قياس امتصاص الأشعة السينية المزدوج الطاقة. وكان متوسط الأحراز - T أقل على نحو يُعْتَدُّ به إحصائياً بين البالغين والمراهقين القصار القامة بالمقارنة مع أصحاب الطول النظامي. وكانت المنبئات بحالة العظام التي اعتُمد عليها في الفِتيان المراهقين هي العمر، ومَنْسَب كتلة الجسم BMI، والطول المكتسب (الحَرَز - Z)، والحَرَز - T للأمهات، أما المُراهقات الفَتَيات فكانت المنبئات بحالة العظام فيهنّ هي مَنْسَب كتلة الجسم، والعمر عند بدء الإحاضة، والحَرَز - T والحرَز - Z في الوالدَيْن. يُعاني المراهقون القصار القامة من قلة كثافة كتلة العظام، في حين أن البالغين القصار القامة يُعانون من زيادة انتشار تخلخل العظام.
ABSTRACT: Little is known about bone mass acquisition among stunted adolescents who did not achieve their growth in height. A national survey was made of bone mineral density among stunted adolescents and adults. A multistage stratified random sample of 2500 families (8476 adolescents and their parents) was selected from 6 governorates in different geographical areas of Egypt. Clinical history, anthropometry and measurement of bone mineral density using dual energy X-ray absorptiometry was done. Mean T-scores were significantly lower among both adults and adolescents with short stature compared with those of normal height. The predictors of bone status among adolescent boys were age, body mass index (BMI), height attained (z-score) and maternal T-score and for girls were BMI, age at menarche, paternal T-score and z-score. Stunted adolescents suffered from low bone mass density and low stature adults suffered a high prevalence of osteoporosis.
Densité minérale osseuse chez des adolescents et des adultes égyptiens de petite taille : résultats d’une enquête nationale
RÉSUMÉ: Les connaissances sont rares en matière d’acquisition de la masse osseuse chez les adolescents souffrant d’un retard de croissance et n’ayant pas atteint leur taille cible. Une enquête nationale a été réalisée sur la densité minérale osseuse des adolescents et des adultes atteints d’un retard de croissance. Un échantillon aléatoire stratifié à plusieurs degrés de 2500 familles (8476 adolescents et leurs parents) a été sélectionné dans six gouvernorats de plusieurs zones géographiques d’Égypte. Les antécédents médicaux ont été notés, les mesures anthropométriques ont été prises et une ostéodensitométrie a été réalisée au moyen d’une absorptiométrie biénergétique aux rayons X. Les T-scores moyens étaient significativement inférieurs chez les adultes comme chez les adolescents de petite taille par rapport aux scores observés chez les personnes de taille normale. Les facteurs prédictifs du statut osseux chez les adolescents de sexe masculin étaient l’âge, l’indice de masse corporelle, la taille atteinte (Z-score) et le T-score maternel ; chez les adolescentes, les facteurs prédictifs étaient l’indice de masse corporelle, l’âge à l’apparition des premières règles, et les T-scores et Z-scores paternels. Les adolescents atteints d’un retard de croissance souffraient d’une densité minérale osseuse faible et les adultes de petite taille présentaient une forte prévalence d’ostéoporose.
EMHJ, 2011, 17(8): 687-693
1National Nutrition Institute, Cairo, Egypt (Correspondence to S.A.Ibrahim:
Introduction
Growth stunting constitutes the most common evidence of marginal malnutrition throughout the world [1]. In Egypt, the prevalence of linear growth retardation among adolescents aged 10–18 years is estimated to be 22% [2]. Bone mineralization is an important development stage accomplished during childhood and adolescent growth. Bone mass accumulation generally parallels linear growth; thus a large percentage of total skeletal mass is achieved during the adolescent growth spurt. Failure to achieve an adequate bone mass during adolescence is a risk factor for osteoporosis [3].
Osteoporosis has long been considered a health problem unique to older adults. Yet children and adolescents with chronic illness, primary bone disease, or poor nutrition are also predisposed to impaired skeletal health [4]. Osteoporosis is characterized by a decrease in the amount of normally mineralized bone, leading to bone fragility and susceptibility to fracture. In addition to causing pain, osteoporotic fractures can lead to deformity, permanent disability, loss of independence and even death [5]. We have previously reported on the prevalence of osteoporosis among stunted children attending the stunting outpatient clinic of the Egyptian National Nutrition Institute [6]. Yet there is no adequate information about bone density among stunted adolescents on a national level. The objective of this study was to investigate the levels of bone mineral density (BMD) among Egyptian stunted and normal height adolescents and adults.
Methods
The present study reports data from Egyptian adolescents and adults who were participants in the national study for assessment of BMD among Egyptian adults and adolescents conducted by the National Nutrition Institute in Cairo [7].
Study sites and sample
The total sample included in this survey was 4002 adolescents aged 10–18 years and 4474 of their fathers and mothers who were included for assessment of genetic and lifestyle factors affecting BMD. The age range of mothers was 28–61 years and of fathers was 29–63 years. Exclusion criteria included: pregnancy, all forms of motor disability and inability to stand erect, genetic syndromes, past or present endocrine disorders (other than diabetes), any known skeletal or bone deformities, chronic diseases, drug intake (e.g. corticosteroids or other hormones, antiepileptic drugs, nonsteroidal anti-inflammatories, antacids, tetracyclines, antidiuretic drugs, vitamin supplements, calcium supplements, anticancer drugs) or metabolic conditions that can affect BMD.
Sample selection was done as follows. Cairo was selected as it is the capital and the main metropolitan area of Egypt. The other governorates were divided into 2 main strata. The first was upper Egypt plus the Red Sea and New Valley governorates. This stratum included 10 governorates. Two governorates were randomly selected from this stratum (Red Sea and Sohag governorates). The second stratum encompassed lower Egypt in addition to North Sinai and South Sinai governorates. Three governorates were selected from this stratum (Sharqiya, Beheira and Dakahlia). The 2500 sample units were distributed across the 6 governorates according to their relative sizes. In the field the family lists prepared by family health centres were utilized and 30 families daily in each site were randomly selected from the list.
In all, families were randomly selected from contrasting socioeconomic standards. Sample design and size allowed estimations to be obtained on the national level. These estimates were obtained for rural and urban areas, males and females and for the 3 social classes. Social status was assessed according to the education and occupation of both the father and the mother. A score was given and the families were divided into 3 groups: low, middle and high. The targeted families were listed and 30 in each site were selected randomly and interviewed.
Data collection
BMD was measured in the non-dominant side of the body at the calcaneal process by dual energy X-ray absorptiometry (DEXA) (Norland Apollo TM bone densitometry, Norland Medical System).
Although the World Health Organization (WHO) criteria for diagnosis of osteoporosis (T-score) were not established to be applied to children and adolescents, they were used in this study as a guide to differentiate between adequate level of BMD (normal: BMD 1– > 2.5 SD below the young adult mean) and severe reduction in BMD (osteoporosis: BMD ≥ 2.5 SD below the young adult mean). A patient with 1 or more low-trauma fractures is considered to have osteoporosis regardless of the BMD value [8]. The term osteopenia used here indicates that the adolescent was less advanced in reaching his/her peak bone mass (relative osteopenia). Very low BMD values (osteoporosis) are probably a reflection of underlying pathology but are referred to here as relative osteoporosis.
Weight and standing height were taken from each subject using standard techniques [9]. Height-for-age z-score (HAZ) was calculated and body mass index (BMI) using the computer software Anthro, version 1.01.
Ethical approval for the study was obtained from both the Ministry of Heath and Population (Egypt) and the General Organization for Teaching Hospitals and Institutes.
Data processing and analysis
The data of all participants were divided into 2 groups according to their heights. Short stature was defined as HAZ < –2SD for adolescents, adult height < 163.6 cm for males and < 151.8 cm for females [10]. The BMI of all adults were classified as under, normal, overweight or obese in accordance with WHO classification for BMI for adults and percentile BMI-for-age for adolescents [11].
Data were analysed in the data management and statistical unit of the National Nutrition Institute. Descriptive analysis using means, standard deviation (SD) and Student t-test was done using SPSS, version 10.0, including frequency distribution and cross-tabulation. Means were compared using analysis of variance (ANOVA). Differences were considered significant at P < 0.05.
Results
Adolescents
The total number of enrolled adolescents was 4002 (2003 boys and 1999 girls). The mean level of BMD was significantly lower among the stunted males and females compared with the normal height adolescents of the same sex. The results were the same for all age groups and among both sexes (Table 1).
Table 1 Mean level of bone mineral density (BMD) of the normal height and stunted adolescents by age and sex
The mean T-scores were –1.7 (SD 0.9) for the stunted adolescents compared with –1.1 (SD 1.0) for the normal height group (P < 0.001). Among stunted boys, 31.1% had relative osteoporosis, 44.7% relative osteopenia and only 24.1% had normal bone density. Among normal height boys 14.9% had relative osteoporosis, 45.2% relative osteopenia while 39.9% had normal bone density (Figure 1).
Only 0.5% of normal height girls and 5.4% of stunted girls had relative osteoporosis, while relative osteopenia was prevalent among 26.5% of normal height and 54.2% of stunted girls. Normal bone density was found among 73.0% of normal height and only 40.5% of stunted adolescent girls (Figure 1).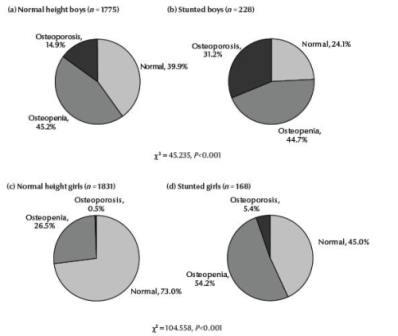
Figure 1Distribution of T-scores in the categories normal, osteopenia and osteoporosis (according to the World Health Organization 1998 cut-offs) among the normal height and stunted boys and girls
Using T-scores as the dependent variable, the predictors of bone status among adolescent boys were age, BMI, height attained (HAZ score) and maternal T-score and for girls were BMI, age at menarche, paternal T-score and HAZ score (Table 2). This table shows that the age of male adolescents was the most influential among the tested variables. BMI was also influential and adolescents with high BMI values had higher T-scores than those with low BMI. HAZ score had an impact on BMD, so that the greater the height attained for age, the higher the T-score. Among females T-score was affected significantly by BMI, whether the girl had reached menarche or not, and HAZ score.
Table 2 Predictors of bone status among the studied adolescents using T-score as the dependent variable
Adults
The total number of adults examined was 4474 (2028 fathers and 2446 mothers of the adolescents).
Short stature was prevalent among 18.8% of adult males. Of this group 24.9% had osteoporosis compared with 12.9% of normal height males. Osteopenia was prevalent among 17.3% of the short compared with 13.3% of normal height men (P < 0.001) (Figure 2).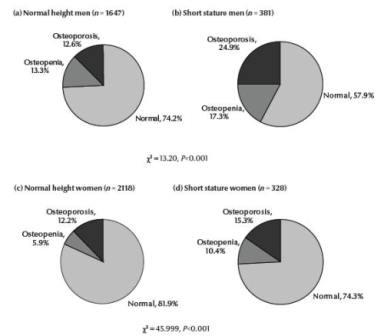
Figure 2 Distribution of T-scores in the categories normal, osteopenia and osteoporosis (according to the World Health Organization 1998 cut-offs) among the normal height and short stature men and women
Among adult females, short stature was found in 13.4%. Of this group 15.3% had osteoporosis compared with 12.2% of normal height women. Osteopenia was prevalent among 10.4% of the short compared to 5.9% of normal height women (P < 0.001) (Figure 2).
In both males and females adult height was significantly correlated with BMD (r = 0.073, P < 0.001 and r = 0.073, P < 0.001 for males and females respectively). The mean levels of the studied parameters among adults are presented in Table 3. There was a significant difference (P < 0.001) between the mean T-scores in both normal height and short stature adults (males or females). Mean value of BMD were significantly higher (P < 0.001 ) among normal height males, while the mean levels of BMI were significantly higher (P < 0.001 ) among short stature females.
Table 3 Mean levels of the bone mineral density (BMD), T-scores and body mass index (BMI) among adults
Discussion
In the past decade there has been considerable interest in the assessment of BMD in children. This has been driven partly by recognition of the fact that the risk of osteoporosis in adults is influenced by peak bone mass, which is largely achieved during childhood and adolescence [12]. Children with chronic disease may have compromised bone growth and bone mineral accrual, increasing the lifetime risk of osteoporosis [13]. It has been suggested that measurement of BMD by DEXA is influenced by bone size and therefore DEXA results need to be interpreted with caution in children who are growth retarded [14]. The present study revealed that stunted adolescents had lower levels of bone mineralization at adolescents with an adequate height for their age. It seems unlikely that bone size is the reason for this low BMD, as 24.1% and 40.5% of stunted boys and girls had normal BMD. A previous study of stunted adolescents at the same institute found that some had normal BMD, some had osteopenia and others had osteoporosis. Age and HAZ score did not differ between the groups but serum levels of calcium and magnesium and dietary intake of fat, zinc, copper, vitamin A and folic acid were significantly lower in the stunted group with osteoporosis compared with stunted adolescents with adequate BMD [15]. Our team has also reported mild trauma fractures and repeated fractures among stunted adolescents in a previous study. We found no significant difference in BMD between short and normal height adolescents of the same BMI, and speculated that the markedly reduced BMD among the stunted group was mainly due to reduced body weight and delayed puberty associated with stunted growth [6]. We can suggest that both osteoporosis and some cases of stunted growth may have the same etiology.
In the present study, an independent predictor of low BMD among the adolescents was high BMI. This result agrees with those of Ibrahim et al., Matter et al. [16] and Henrick [17], who found that weight was predictive of adolescent BMD. HAZ was also found to be predictive of bone status. Children with idiopathic short stature were reported to have low BMD that increased after 1 year of growth hormone therapy [18].
In this study among adults there was a positive association between height and BMD. In both males and females, osteoporosis was more prevalent among those with short stature; a condition that clearly starts at a younger age. The clinical implications of the above findings are important. Calcium supplementation may be a treatment for both stunted growth and osteoporosis. In a previous study, height gain in stunted adolescents was found to increase significantly after calcium and multiple micronutrient supplements as compared with placebo. Those suffering from osteoporosis at the start of the trial had marked height improvement. Unfortunately, the study did not assess changes in BMD after supplementation [19]. Further longitudinal studies are required to understand the evolution of reduced BMD in young people and adults with short stature.
Conclusion
Stunted adolescents suffer from low BMD, and short stature adults suffer a high prevalence of osteoporosis. Osteoporosis may be one of the remote complications of stunted growth.
Acknowledgements
The study was sponsored by the General Organization for Teaching Hospitals and Institutes, Ministry of Health and Population, Egypt.
References
- The state of the world’s children 2006: excluded and invisible. Geneva, United Nations Children’s Fund, 2006.
- Final report on the national study: prevalence of obesity in Egypt. Cairo, Egypt National Nutrition Institute, 2004.
- Leonard MB, Zemel BS. current concepts in paediatric bone disease. Paediatric gastroenterology and nutrition. Pediatric Clinics of North America, 2002, 49:143–173.
- Henwood MJ, Binkovitz L. Update on pediatric bone health. Journal of the American Osteopathic Association, 2009, 109:5–12.
- Broadus AE. Physiologic functions of calcium, magnesium and phosphorus. In: Favus MJ, ed. Primer on the metabolic bone diseases and disorders of mineral metabolism. Washington DC, American Society of Bone and Mineral Research, 1993:41.
- Ibrahim SA et al. Bone mineral density and bone markers among stunted Egyptian adolescents. Journal of Nutritional and Environmental Medicine, 2003, 3:93–101.
- National survey for determination of bone mass density among adolescents and adults in Egypt. Final report. Cairo, Egypt National Nutrition Institute, 2004.
- Definition of osteoporosis and related terms. In: Guidelines for preclinical and clinical trials in osteoporosis. Geneva, World Health Organization, 1998:5–25.
- Jelliffe DB. The assessment of the nutritional status of the community: with special reference to field surveys in developing regions of the world. Geneva, World Health Organization, 1989.
- Measuring changes in nutritional status. Guidelines for assessing the nutritional impact of supplementary feeding programmes for vulnerable groups. Geneva, World Health Organization, 1983.
- Obesity: preventing and managing the global epidemic. Geneva, World Health Organization, 1997.
- Schoenau E et al. The bone mass concept: problems in short stature. European Journal of Endocrinology, 2004, 151:S87–91.
- Bachrach LK. Consensus and controversy regarding osteoporosis in the pediatric population. Endocrine Practice, 2007, 13:513–520.
- Langman CB, Levine MA, Sylvester F. Osteoporosis clinical updates. Osteoporosis in children and adolescents. Washington DC, National Osteoporosis Foundation 2005.
- Ibrahim SA et al. Nutritional deficiencies as risk factors for low BMD in stunted adolescents. Importance of food supplements and nutrition education. Nutrafood, 2007, 6(1):25–30.
- Mattar MK et al. Bone mineral density and nutrient intake among stunted Egyptian adolescents. Medical Journal of Cairo University, 2003, 71(1) (Suppl.):45–51.
- Henrick D. Bone mass in young adults—determinants and fracture prediction. Malmo, Sweden, Department of Orthopaedics, University of Malmo Hospital, 1997.
- Lanes R et al. Growth velocity, final height and bone mineral metabolism of short children treated long term with growth hormone. Clinical Endocrinology, 2002, 57:725–730.
- Ibrahim SA et al. Could micronutrient supplementation increase the growth of stunted Egyptian children? Egyptian Journal of Nutrition (Cairo), 2003, 18: 000–000.








