Case report
I.H. Bouraoui,1 O. Essid,1 H. Boughammoura,2 N. Arifa,1 R. Frikha,2 H. Jemni 1 and K.T. Graiess 1
1Department of Radiology; 2Department of Orthopaedics, Sahloul Hospital, Sousse, Tunisia (Correspondence to I.H. Bouraoui: This e-mail address is being protected from spambots. You need JavaScript enabled to view it )
Received: 03/03/10; accepted: 07/06/10
emhj, 2011, 17(12): 994-995
Introduction
Primary musculoskeletal hydatidosis is very rare and represents 1%–5% of all cases of echinococcosis [1]. Patients are typically asymptomatic and the cyst presents as a slow growing soft tissue tumour [2].
The diagnosis is usually easy in imaging by ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI). Sometimes, unusual imaging appearance because of complicated cysts can make diagnosis difficult [3].
We report here a case of forearm hydatid cyst with an unusual presentation.
Case report
A 23-year-old woman presented to Sahloul Hospital, Sousse in February 2009 with a history of a slow-growing mass on her forearm over the past 65 days. The patient resided rurally and had not consulted a doctor previously. She had been putting olive oil on and massaging her forearm many times.
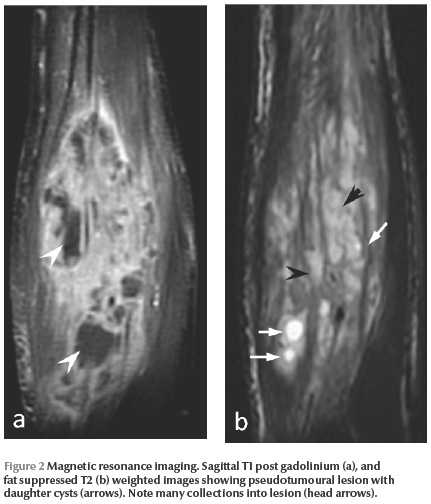
On physical examination, the mass was 14 × 7 × 6 cm, painful, warm and erythematous. Her fingers were retracted and Volkmann syndrome was suspected (Figure 1). US showed an echogenic solid and lobulated mass and a diagnosis of a tumour or abscess was made. MRI showed an impotent and heterogeneous soft tissue lesion with intermediate T1 and hyperintense T2 signals. T1 weighted images with fat suppressed and gadolinium injection demonstrated diffuse and considerable enhancement of the lesion suggestive of a tumour. T2 weighted images showed a low-density area in the lesion compatible with an abscess and fat suppressed T2 images showed 3 small cysts suggestive of hydatid disease (Figure 2 ). There were no bone abnormalities.

Laboratory tests and CT of the thorax and abdomen were all normal.
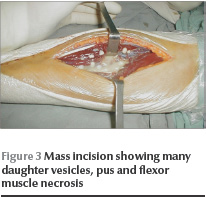
Surgery was performed to remove the mass because the cyst was infected and there was a risk of spread of the disease. At surgery, hydatidosis was confirmed. Many daughter vesicles were identified and flexor muscle necrosis and fibrosis were noted (Figure 3). At 3-year follow-up there was no evidence of local or distant recurrence but the patient still had obvious unsatisfactory finger stretching.
Discussion
In our case, while US showed a pseudotumoural lesion and MRI showed an impotent lesion enhancement and abscesses, the presence of some small daughter cysts led to a diagnosis of hydatid cyst.
Musculoskeletal echinococcosis is very rare because few embryos can escape the capillary filtrating systems of the liver and lung [1,2]. It has been suggested that muscle is inhospitable for hydatid infestation and provides a poor environment for the parasite because of the presence of lactic acid [4,5].
A combination of epidemiological, clinical, laboratory and radiographical findings is necessary to make the diagnosis. Echinococcosis should be considered when slowly growing soft tissue is developing in patients from rural areas, especially in endemic countries [5]. In case of complication (fissuring or infection) the cyst mimics an abscess or a soft-tissue tumour [3].
The preoperative radiological diagnosis is important to avoid biopsy and prevent serious complications, such as local recurrence and risks of anaphylaxis. Radiographs eliminate bone involvement and may shows calcifications in 38% of the cases [1]. US is the most useful mean of diagnosis, showing the pathognomonic signs of the hydatid cysts: echogenic hydatid sand (“snowflake sign”), unilocular cysts with daughter cysts (“honeycomb sign”) and cysts with a detached floating laminated membrane (“waterlily sign”) [1,5].
In CT, complicated cases represent a real diagnostic problem, as in US a soft tissue tumour cannot be excluded [3].
MRI is the imaging method of choice for the differential diagnosis. Rim sign and multicystic appearance are typical features of hydatid cyst [3,6]. The lesion usually has a high signal intensity on T2 and low intensity on T1 typically with daughter cysts. The rim sign, a low intensity rim on both T1 and T2, is not specific to hydatidosis and can also be seen in tumours with fibrous capsule. Pericystic enhancement can be seen and is often moderate [5] but in our case the enhancement was weak and diffuse because of the infection of the cyst. If the cyst is complicated, it is very important to search for daughter cysts, especially in fat suppressed T2 weighted images [4].
Pretherapeutic serology can be negative. Seronegativity does not exclude the diagnosis hydatidosis, but seropositivity may be helpful if diagnosis is difficult, especially when the cyst mimics a tumour or abscess and imaging appearance is not specific [1,7].
Surgical excision of the cyst has long been considered the only effective treatment and is still the treatment of choice [5]. However, the removal of the main cyst mass may not be effective, and drainage together with hypertonic saline irrigation is necessary. Currently complementary chemotherapy (albendazole) and percutaneous treatments have become widely recommended [5,7].
Human hydatidosis should be considered in the differential diagnosis of every soft tissue mass, especially in countries endemic for Echinococcus.
References
- Basarir K et al. Primary muscular hydatidosis mimicking soft tissue tumour: a report of five cases. Journal of Orthopaedic Surgery, 2008, 16:368–372.
- Ozkoc G et al. Primary hydatid disease of the quadriceps muscle: a rare localization. Archives of Orthopaedic and Trauma Surgery, 2003, 123:314–316.
- Alouini Mekki R at al. Kyste hydatique des tissus mous : apport de l’IRM (à propos de trois observations) [Hydatid cyst of soft tissues: MR imaging findings (Report of three cases)]. Journal de Radiologie, 2005, 86:421–425.
- Garcia-Diez AI et al. MRI evaluation of soft tissue hydatid disease. European Radiology, 2000, 10:462–466.
- Mseddi M et al. Kyste hydatique musculaire: a propos de 11 cas [Hydatid cysts in muscles: eleven cases]. Revue de chirurgie orthopédique, 2005, 91:267–271.
- Alexiadis G et al. Primary muscular hydatidosis. US, CT and MR findings. Acta Radiologica, 2002, 43:428–430.
- Buyukbebeci O et al. Combined treatment of primary hydatid disease of the vastus lateralis muscle. Orthopedics, 2004, 27:621–622.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)