Review
P. Metzger,1 N.A. Baloch,2 G.N. Kazi1 and K.M. Bile1
مكافحة السل في باكستان: استعراض عقد من النجاح والتحدِّيات
بيتـر متزيقار، نور أحمد بلوش، غلام نبي قاضي، خليف بلّه محمود
الخلاصـة: شهدت باكستان توسعاً هائلاً في رعاية المصابين بالسل خلال العقد المنصرم، فازداد التبليغ عن الحالات من 050 11 عام 2000، إلى 115 248 في عام 2008. فقد تلقَّى ما يزيد على مليون مصاب بالسل الرعاية منذ عام 2000، وبمعدل نجاح المعالجة 91% في عام 2007. وتقدم هذه الورقة القرارات الاستـراتيجية ومجالات التحسن في البنية الأساسية التي أدت إلى هذه النجاحات، مثل تنفيذ تغطية شاملة للمعالجة القصيرة الأمد تحت الإشراف المباشر، وتوسيع نطاق شبكات المختبرات، ونُظُم إدارة الأدوية الفعَّالة، واستـراتيجيات التواصل المحسَّنة، وإدخال الأطباء الممارسين والمختبرات والمستشفيات في برنامج مكافحة السل من خلال استـراتيجية تجمع القطاعَيْن العام والخاص. كما ترسم الورقة ملامح التحدِّيات التي تواجه توسيعاً أكثر لنطاق مكافحة السل ضمن القطاع الخاص، وضمن مؤسسات الرعاية الصحية خارج القطاع الحكومي، وتعزيز شبكة المختبرات لتشخيص السل المقاوم للأدوية، وضمان الإمداد المتواصل بالأدوية المضادة للسل الرفيعة الجودة، وكل هذه الملامح تـتطلَّب دعماً متواصلاً ومنسَّقاً تقنياً ودعماً من المانحين.
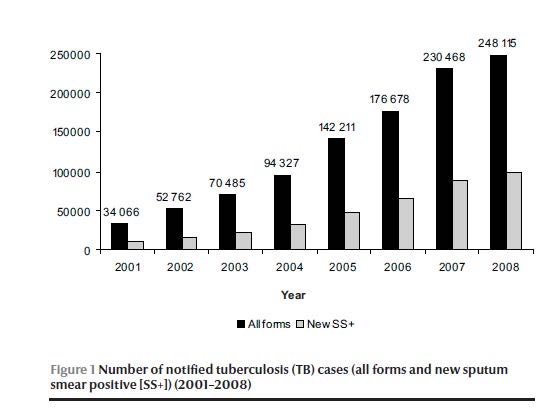
ABSTRACT Pakistan has shown drastic expansion of tuberculosis (TB) care during the past 10 years, increasing case notifications from 11 050 in 2000 to 248 115 in 2008. Over 1 million TB patients have been cared for since 2000, with a treatment success rate of 91% in 2007. This paper examines the strategic decisions and infrastructure improvements underlying this achievement, such as the implementation of universal DOTS coverage, expansion of the laboratory network, effective drug management systems, improved communication strategies, and inclusion of private practitioners, laboratories and hospitals in the TB control programme through the public–private mix strategy. The paper also outlines challenges faced in further expanding TB control within the private sector and parastatal health care institutions; strengthening the laboratory network for diagnosis of drug-resistant TB; and ensuring uninterrupted supply of quality anti-TB drugs, all requiring continued and coordinated technical and donor support.
Lutte contre la tuberculose au Pakistan : analyse d’une décennie de succès et de difficultés
RÉSUMÉ Au cours des dix dernières années, les soins concernant la tuberculose se sont considérablement développés au Pakistan. Ainsi, les cas signalés sont passés de 11 050 en 2000 à 248 115 en 2008. Plus d’un million de patients atteints de tuberculose ont été soignés depuis 2000, avec un taux de réussite thérapeutique de 91 % en 2007. Cet article étudie les décisions stratégiques et les améliorations des infrastructures à l’origine de cette réussite, comme la mise en œuvre d’une couverture universelle pour le traitement de brève durée sous surveillance directe, le développement du réseau de laboratoires, des systèmes efficaces pour la gestion des médicaments, l’amélioration des stratégies de communication et l‘intégration de praticiens, de laboratoires et d’hôpitaux privés dans le programme de lutte antituberculeuse, dans le cadre d’une stratégie associant secteurs public et privé. L’article met également l’accent sur les difficultés rencontrées dans l’extension de la lutte antituberculeuse au sein du secteur privé et des établissements de soins semi-publics, le renforcement du réseau de laboratoires pour le diagnostic de la tuberculose pharmacorésistante et la garantie d’une fourniture continue en médicaments antituberculeux de qualité. Ces trois points requièrent un soutien technique et un appui des bailleurs de fonds continus et coordonnés.
1World Health Organization, Country Office, Islamabad, Pakistan (Correspondence to P. Metzger:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
2National Tuberculosis Control Programme, Islamabad, Pakistan.
EMHJ, 2010, 16(Supplement) : S47-S53
Introduction
Tuberculosis (TB) is globally the second most common cause of death from infectious diseases, killing almost 2 million people annually. An estimated 8 million new TB cases occur every year, of which 80% are among people in the most economically productive age groups [1], representing a major economic burden for individuals and countries [2]. Twenty-2 high-burden countries account for about 80% of the total TB disease burden worldwide. Although sub-Saharan Africa has the highest incidence rate, Bangladesh, China, India, Indonesia and Pakistan together account for half of the global TB burden [3].
The 2008 estimated incidence in Pakistan of 181 cases of TB per 100 000 population, or 297 000 cases, and of 81 new sputum smear positive (SS+) cases per 100 000 population, or 133 000 cases, is likely an underestimate of the true burden of disease [3]. The 2008 estimates have recently been revised through a consultative process with the country, applying a new methodology that takes into account the “missed” cases and, in the absence of a prevalence survey, uncertainties in estimates reflected in large confidence intervals.
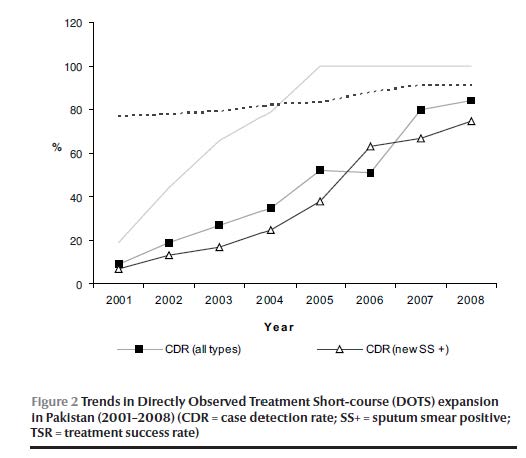
According to previous estimates, the case detection rate for all TB cases gradually improved from 19% in 2002 to 84% in 2008; for new SS+ cases the case detection rate increased from 13% to 74%. However, with the recent higher estimates of TB incidence, the case detection rate for all TB cases is about 60% and for new SS+ cases is about 58% [4].
Nevertheless, the Pakistan National Tuberculosis Programme (NTP) has achieved a remarkable and steady improvement in numbers of TB cases detected, from 11 050 in 2000 to 248 115 in 2008, and treatment success rates reached 91% in 2007. This has been achieved through extraordinary commitment and financial inputs by the Government and health development partners, providing support for strategic and infrastructure improvements by the NTP.
The World Health Organization (WHO) Directly Observed Treatment Short-course (DOTS) strategy for TB was adopted and piloted in Pakistan from 1995 onwards, but major progress in TB control was only achieved after the revival of the NTP in 2001 when TB had been declared a national public health emergency through the “Islamabad Declaration”. The NTP functions under the Ministry of Health and is responsible for overall coordination, policy direction and technical guidance for TB control, while actual implementation is the responsibility of the Provincial TB Programmes (PTPs) and district health authorities. The NTP central unit links closely with PTP managers and district TB coordinators.
TB services are integrated into the primary public health care system at district level. However, the private sector is regarded as the first point of entry to the health care delivery system for most users, and the majority of private providers are not following NTP guidelines [5–7]. A 2003 survey conducted by the NTP and PTPs in Lahore and Rawalpindi districts found that less than 3% of general practitioners (GPs) were following the national guidelines for diagnosis and management of TB, while 90% of GPs were relying on chest radiography for diagnosis [8,9].
At the end of July 2009, 115 463 doctors were registered with the Pakistan Medical and Dental Council while 42 700 registered facilities were providing formal and informal medical services, of which 69% were clinics and pharmacies, while 550 were private hospitals.
Parastatal health services form another point of entry outside the public health care system and NTP regulation. Overall, 32 federal ministries and the cabinet secretariat with 208 autonomous (parastatal) bodies provide health services to 389 923 employees and their dependants [10], not including the Ministry of Defence, which has its own specific budgetary outlay for health services.
In recent years, a high priority has been given to developing viable partnerships with health care providers in the private sector, adopting a systematic approach consistent with WHO guidelines [11]. Additional initiatives such as an improved surveillance and laboratory network and improved follow-up and treatment modalities, funded by global and national sources, have contributed to the significant improvement in case detection and treatment success rates outlined above. The objective of this review is to highlight the achievements of Pakistan’s NTP over the past decade and to outline the outstanding priorities and challenges for the future.
Methods
An extensive literature review was undertaken. Research papers on TB in Pakistan, NTP annual reports, donor reports, joint partner review reports, technical guidelines and project proposals were analysed.
Results
Epidemiology of TB
TB is highly epidemic in Pakistan. According to the latest WHO estimations, the incidence, prevalence and mortality of TB in Pakistan are 230 per 100 000, 310 per 100 000 and 39 per 100 000, respectively. This indicates 410 000 incident cases of TB and 69 000 TB deaths in Pakistan every year. Pakistan is the sixth highest TB burden country in the world and by far the largest among the 22 countries of WHO’s Eastern Mediterranean Region. The NTP and partners are planning to conduct a disease prevalence survey for TB in Pakistan in 2010 in order to have more precise and comprehensive information on the disease burden.
The 248 115 cases of all types (Figure 1) notified in 2008 included 99 670 new SS+ cases (Table 1). The treatment success rate of 91% of new SS+ cases notified during 2007 exceeded the WHO target of 85% (Figure 2) due to a reduction of the default rate to under 4%, and low death, failure and transfer out rates (2%, 1% and 2%, respectively). However, the increase in notifications has slowed down since 2007, with only Punjab province reporting a substantial increase in notified cases and the majority of districts showing either stagnant or declining case notifications (Table 1).
Programme planning and strategic framework
Following the “Islamabad Declaration” the Government of Pakistan called upon its development partners to make concerted efforts to control the disease. A 5-year plan was devised leading to universal DOTS coverage in the public sector towards the end of 2005. The funding was lined up efficiently by the federal Ministry of Health and provincial Departments of Health, with responsibilities delineated and TB control activities integrated into the primary health care system. DOTS implementation was characterized by challenges concerning human resources, suboptimal quality of services at public health outlets and lack of commitment at peripheral levels. District implementation plans were developed and executed through a phased approach until the expansion of DOTS services to all tiers of the district health system was achieved. The devolution process necessitated liaison with district governments to ensure sufficient allocations for the procurement of anti-TB treatment (ATT) drugs, as 90% of drug procurement was performed by provinces and districts.
Universal DOTS coverage (DOTS All Over) was achieved in the public sector in 2005. Reaching DOTS All Over signified the availability of free diagnosis and treatment for TB patients in all districts in the public sector health care delivery network. Subsequently, the government approved the NTP federal workplan (PC-1) for 5 years starting from the financial year 2006/2007 and allocated 1.181 billion Pakistan rupees (PKR), equivalent to US$ 14 million, for TB-related activities, including staff training, expansion of the laboratory network, availability of quality drugs, surveillance, monitoring and evaluation, intra- and intersectoral partnerships, research and development, public– private mix (PPM) and behaviour change communication. In order to effectively complete these activities, the NTP has expanded its central unit with relevant expertise in laboratory, monitoring and evaluation, programme planning and management, as well as in advocacy, communication and social mobilization and research.
Partnership building
An interagency coordinating committee guides donor support and the multiple partners’ technical assistance for the programme. The NTP and PTPs organize annual joint programme reviews on TB care in Pakistan, in collaboration with all partners [Department for International Development (DFID), Family Health International (FHI), German Leprosy and Relief Association (GLRA), German Development Bank (KfW), German Technical Cooperation (GTZ), Japan Anti-Tuberculosis Association/Research Institute for Tuberculosis (JATA/RIT), Japanese International Cooperation Agency (JICA), Royal Netherlands Association for the Prevention of Tuberculosis (KNCV Tuberculosis Foundation), International Union Against Tuberculosis and Lung Disease (The Union), United States Agency for International Development (USAID)] through WHO support. The recommendations of these reviews guide the follow-up action at the relevant operational level. A country coordination mechanism has also been formulated to facilitate partners’ coordination, particularly for the implementation of grants from the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM).
Case detection through quality-assured bacteriology
The laboratory network for TB diagnosis by sputum smear microscopy (SSM) and bacteriology is comprised of the National Reference Laboratory in Islamabad (operational since September 2009), 4 Provincial Reference Laboratories, 3 intermediate (regional) laboratories, 112 district intermediary laboratories and over 1100 peripheral laboratories including 92 operated by not-for-profit civil society organizations. Laboratory services are integrated in primary health care facilities at district level, serving an average of 140 000 individuals per facility. Through PPM activities, another 52 commercial laboratories are collaborating with the network, raising their participation from less than 50 in 2001 to over 900 in 2005.
Subsequently, the focus shifted from expansion to consolidation and improvements in quality, with external quality assurance of SSM emerging as a high priority. External quality assurance by blinded rechecking was initiated in 2005 (JICA/NTP) and the system was then piloted in 40 districts (Canadian International Development Agency/WHO) before being universally rolled out. Currently, external quality assurance expansion is ongoing through GFATM R-6 with WHO support, covering 90% of SSM laboratories at the end of December 2009.
Standardized treatment with supervision and patient support
According to NTP guidelines, treatment is delegated from the diagnostic centre (rural health centres or hospitals) to the basic health unit (BHU) level. Lady health workers are regarded as the main treatment supporters. A standardized 8-month treatment regimen for new cases, with 6 months’ ethambutol and isoniazid (EH) in the continuation phase, is still in place. In all the provinces since 2008, a substantial proportion of the management of the BHUs has been delegated to the Peoples’ Primary Health Initiative, a nongovernmental entity to which most of the BHUs of the country were outsourced, requiring coordination links to be established for DOTS implementation. The Peoples’ Primary Health Initiative was launched initially by the Ministry of Industries and Special Initiatives and is currently managed by the Cabinet Division. In Punjab, the Punjab Rural Support Programme runs BHUs in a number of districts.
Effective supply and drug management system
The NTP and provincial governments have ensured the availability and accessibility of first-line ATT drugs at all levels of the PHC system through locally produced drugs purchased through the federal and provincial budgets or through interim grants from the Global Drug Facility.
Monitoring, evaluation and impact measurement
The NTP is responsible for monitoring the overall programme performance. WHO programme officers, based at national, provincial and district levels since 2003, play a critical role in monitoring TB control activities and providing technical capacity building support to provincial and district health authorities and professionals through district TB coordinators, who have the primary responsibility of implementing and supervising TB control activities at the diagnostic centres. Quarterly surveillance meetings at district, provincial and national level ensure data verification and validation between implementing partners. Findings and lessons learnt from external joint partner reviews conducted annually by WHO, local and international partners assist the NTP and PTPs in revising their implementation strategies.
Public–private mix (PPM)
To introduce TB control according to NTP guidelines into the lagging private sector, the NTP engaged 4not-for-profit organizations for the implementation of PPM DOTS pilot projects in 30 selected districts (co-funded by GFATM R-2 and R-3). Public sector funds were allocated in 2003 for implementation of 1 district-led PPM model, currently being implemented in 6 districts. In addition, the Greenstar Social Marketing Pakistan (Guarantee) Limited model was introduced in 5 metropolitan cities through GFATM R-3, involving private laboratories for SSM, where more than 1000 GPs have been engaged in TB DOTS. Further expansion of PPM was based on a situational analysis and design of a range of PPM models suitable for private care providers, encompassing nongovernmental organization clinics, GPs and private hospitals.
A 2008 WHO-assisted mission found that in the preceding year (2007), PPM initiatives contributed to nearly 20% of total notifications (all cases and new SS+). Table 2 presents data from 3 provinces with 90% of all notified cases in 2007. In the 3 provinces combined, 51% of all cases detected by non-NTP providers were new SS+ cases, while among those detected in the public sector, only 39% were new SS+ cases.
Another PPM strategy is “hospital DOTS linkage” which is currently implemented in 27 out of 67 public and private tertiary care hospitals by enhancing laboratory services for SSM, introducing standardized treatment and developing referral systems between the hospitals and peripheral treatment centres through DOTS centres (established under GFATM R-6). Data from districts where DOTS linkages have been introduced showed an increase of up to 50% in case notifications during 2009.
Drug-resistant TB
After achieving countrywide DOTS coverage in 2005, the NTP Pakistan expanded the scope of its activities to include multidrug-resistant tuberculosis (MDR-TB) interventions, as recommended in the new Stop TB Strategy.
Network for culture and drug susceptibility testing of Mycobacterium tuberculosis
A few private and parastatal laboratories located in Karachi, Islamabad and Rawalpindi are externally quality assured for culture and drug susceptibility testing (DST). The NTP is collaborating with the microbiology laboratory of Aga Khan University Hospital, Karachi for capacity building of the public sector.
TB/HIV
Sixteen sentinel sites have been strengthened through collaborative efforts of the NTP, the National AIDS Control Programme and nongovernment partners for screening, care and support of TB/HIV coinfected patients.
Advocacy, communication and social mobilization
Extensive advocacy, communication and social mobilization activities in 57 districts have laid the foundation for initiating MDR-TB and TB/HIV coinfection interventions. Engagement of mass media took place to improve awareness and reduce stigma. A national advocacy, communication and social mobilization strategic framework, monitoring and evaluation framework, and trainer/trainee manuals for quality assurance on interpersonal communication have been developed and disseminated.
Operational research
Operational research was a core component of the national strategic and operational plans. The NTP has constituted 1 national and 4 provincial research groups and developed partnerships with the Pakistan Medical Research Council and linkages with international academic and research institutions. WHO supported the programme through its initiatives of EMRO/Tropical Diseases Research (TDR) Small Grants Scheme) and priority public health areas, involving more than 20 research studies relating to DOTS expansion, defaulter tracing, drug management, external quality assurance, treatment support and drug side-effects. Two new methodologies for indirect estimation of disease burden have been piloted. The research findings were translated into policy through the necessary changes in protocols and guidelines.
Discussion
The significant achievements of the NTP in expanding DOTS to the public sector of every district, initiating PPM strategy [12,13], and steadily increasing case notification and treatment success rates [14,15] hinge on sustained Government commitment and funding for TB control, and technical and financial support from national and international partners, including WHO, USAID, DFID, GTZ/KfW, JICA, World Bank and GFATM.
A number of research studies conducted in Pakistan have significantly added value to the knowledge and operational capacity of the programme, including the TB health-seeking behaviour and practices of the general population, and have facilitated the design of effective communication strategies [16–21]. The predictors of default and major barriers to treatment adherence were identified as poor patient–provider interaction and patients’ lack of knowledge regarding side-effects and stigma [22,23].
Planned interventions to sustain and further scale-up the progress are listed below along with challenges for the future:
An uninterrupted supply and funding for first-line ATT drugs and commodities has been assured until 2012 through funding from the Government, Japanese Counter Value Funds, Global Drug Facility (grant for paediatric drugs) and GFATM R-8. However, long-term strategies for financing an uninterrupted supply of quality-assured first- and second-line ATT drugs, including paediatric formulations, are needed.
Expansion of the TB surveillance system and preparation for the TB prevalence survey are ongoing. An electronic nominal reporting system is being introduced through WHO technical assistance. A nationwide prevalence survey is planned for 2010/2011 with technical assistance of the USAID-funded Tuberculosis Coalition Assistance Program partners: WHO, KNCV, The Union and JATA.
The engagement of private care providers and parastatal health care facilities, though limited, in establishing DOTS linkages with 27 of 67 teaching hospitals has substantially contributed to the increase in case notifications.
In view of the health-seeking behaviour in the urban and rural populations, scaling-up of DOTS in the private sector in the remaining 60 districts has been recognized as a prerequisite for increasing case detection, provision of standardized care, and inclusion of other health care providers and the remaining parastatal organizations. Funding for these activities has been secured through GFATM R-9 support.
Rolling out of the new WHO-recommended treatment regimen (2009) will need strengthening of case management, delegating supervision of treatment from the diagnostic centres to BHUs. Partnering with the Sindh Peoples’ Primary Health Initiative and the Punjab Rural Support Programme should enable the effective use of BHUs for TB suspect detection and treatment support.
Effecting tangible improvement in the drug management system is the prime objective of GFATM R-8, with Greenstar developing a drug management logistics system. The Tuberculosis Coalition Assistance Program supports the NTP in the revision of drug management and forecasting guidelines. As banning across-the-counter sales of ATT drugs is currently not a viable strategy in Pakistan, the NTP has opted to develop a “seal of quality” for locally produced ATT drugs that meets international quality standards, while WHO is engaged in providing technical assistance to local drug manufacturers aiming to attain a prequalification status.
Rapid improvements in the laboratory network for culture and DST for the diagnosis of drug-resistant TB are prerequisites for its management. Nine laboratories (1 national, 4 provincial, 2 intermediate and 2 in tertiary care hospitals) are currently being upgraded. Four TB culture district-level laboratories (1 in each province) will be made functional through GFATM R-6 support while through GFATM R-9 support the laboratory network for culture and DST will be further developed and rapid testing for MDR-TB introduced in 15 tertiary care teaching hospitals.
Scaling-up of MDR-TB care is an urgent task for Pakistan. WHO estimates an annual incidence of over 13 000 MDR, SS+ cases in Pakistan based on estimates of 3.5% MDR in new cases and 35% in re-treatment cases [24]. A study conducted by the Aga Khan University [25] reports 1.8% primary resistance in a specified annual cohort of notified SS+ new and re-treatment cases.
A representative survey in 2010 will determine baseline drug resistance. This is a follow-up on a MDR-TB preassessment conducted by a WHO mission in 2008. Based on the recommendations of this mission, public and private tertiary hospitals have been identified for piloting MDR-TB management through GFATM R-6 support. The NTP and partners have successfully applied to GFATM R-9 to expand MDR-TB diagnosis and care to 80% of the estimated SS+ cases by 2015. In 2009, the Green Light Committee approved ATT second-line drugs for 1500 cases.
Identified challenges for further scaling-up of TB care include: integration of TB control strategies in preservice curricula; upgrading TB control in the new province of Gilgit–Baltistan and intensifying TB control in underserved areas; innovative approaches for enhancing case detection in marginalized groups with limited access to health services, such as workers in the informal sector and periurban slum populations; introduction of an electronic nominal recording and reporting system for monitoring and evaluation of all programme elements; and adaptation of ACSM strategies and correlation of operational research studies with ACSM activities as relevant for all the 6 pillars of the Stop TB Strategy.
With TB DOTS in place at all public facilities in the country, the focus needs to shift to increased case detection by involving the majority of private providers and introducing standards of TB care in social security institutions and the substantial parastatal sector. Although sustaining progress for over a decade, the NTP nevertheless needs to pursue its activities with greater vigour and expanded framework in order to achieve regional and global targets, including Millennium Development Goals. The full adoption of the WHO Stop TB Strategy in the national plan of 2010–2015 will bridge the current gaps. Moreover, the adaptation of the current NTP managerial set-up to future challenges, with continuous and coordinated technical and donor support, will be instrumental for ensuring sustainability and further success.
References
- Dye C et al. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country (WHO Global Surveillance and Monitoring Project). Journal American Medical Association, 1999, 282:677–686.
- Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis and HIV/AIDS. American Journal of Tropical Medicine and Hygiene, 2004, 71(Suppl. 2):147–155.
- Global tuberculosis control– epidemiology, strategy, financing. WHO report 2009. Geneva, World Health Organization, 2009 (WHO/HTM/TB/2009.411).
- Global tuberculosis control: a short update to the 2009 report. Geneva, World Health Organization, 2009 (WHO/HTM/TB/2009.426).
- Pakistan social and living standards measurement (PSLM) survey, 2004–2005. Islamabad, Federal Bureau of Statistics, Statistics Division, Ministry of Finance, 2005.
- Shah SK et al. Do private doctors follow national guidelines for managing pulmonary tuberculosis in Pakistan? Eastern Mediterranean Health Journal, 2003, 9(4):776–788.
- Arif K et al. Physician compliance with national tuberculosis treatment guidelines: a university hospital study. International Journal of Tuberculosis and Lung Diseases, 1998, 2:225–230.
- Khan JA et al. Knowledge, attitude and misconceptions regarding tuberculosis in Pakistani patients. Journal of Pakistan Medical Association, 2006, 56(5):211–214.
- Khan IM et al. Urging health system research: identifying gaps and fortifying tuberculosis control in Pakistan. Croatian Medical Journal, 2002, 43:480–484.
- National health accounts Pakistan 2005–06. Islamabad, Federal Bureau of Statistics, Statistics Division, 2009.
- Engaging all health care providers in TB control: guidance on implementing public–private mix approaches. Geneva, World Health Organization, 2006 (WHO/HTM/TB/2006.360).
- Baloch AN, Mann G. ?ituation analysis. Public–private partnership models, operational and monitoring & evaluation guidelines for national TB control program Pakistan. Islamabad, Technical Assistance Management Agency to the National Health & Population Welfare Facility, 2006.
- Auer C. Public–private mix DOTS in Pakistan – an assessment (report of a public– private mix TB DOTS mission commissioned by WHO EMRO, 19 August–9 September, 2008). Cairo, Regional Office for the Eastern Mediterranean Region, World Health Organization, 2008 (?ttp://www.ntp.gov.pk/downloads/ppm/PPM%20Assessment.zip, accessed 21 June 2010).
- Mission report – joint review of TB care in Pakistan, 8–13 August 2009. Islamabad, World Health Organization, 2009.
- Annual report 2007. Islamabad, National TB Control Programme, Ministry of Health, 2007.
- Liefooghe R et al. Perception and social consequences of tuberculosis: a focus group study of tuberculosis patients in Sialkot, Pakistan. Social Science & Medicine, 1995, 41:1685–1692.
- Agboatwalla M et al. Gender perspectives on knowledge and practices regarding tuberculosis in urban and rural areas in Pakistan. Eastern Mediterranean Health Journal, 2003, 9:732–740.
- Ali SS et al. Tuberculosis: do we know enough? A study of patients and their families in an outpatient hospital setting in Karachi, Pakistan. International Journal of Tuberculosis and Lung Diseases, 2003, 7:1052–1058.
- Khan A et al. Tuberculosis in Pakistan: socio-cultural constraints and opportunities in treatment. Social Science & Medicine, 2000, 50: 247–254.
- Mushtaq MU et al. Knowledge, attitude and practices regarding tuberculosis in two districts of Punjab. International Journal of Tuberculosis and Lung Diseases, 2010:303–310.
- Khan J et al. Tuberculosis diagnosis and treatment practices of private physicians in Karachi, Pakistan. Eastern Mediterranean Health Journal, 2003, 9(4):769–775.
- Diagnostic and treatment delay in tuberculosis: an in-depth analysis of the health-seeking behaviour of patients and health system response in seven countries of the Eastern Mediterranean Region. Cairo, Regional Office for the Eastern Mediterranean Region, World Health Organization, 2009 (WHO-EM/TDR/009/E).
- Special issue of JPMA on tuberculosis research publications in Pakistan. Journal of Pakistan Medical Association, 2009, 59(Suppl.1):1–122.
- Anti-tuberculosis drug-resistance in the world. WHO/IUATLD global project on anti-tuberculosis drug resistance surveillance, fourth global report. Geneva, World Health Organization, 2008 (WHO/HTM/TB/2008.394).
- Javaid A et al. Prevalence of primary multidrug resistance to anti-tuberculosis drugs in Pakistan, International Journal of Tuberculosis and Lung Diseases, 2008, 12(3):326–331.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)