M. Sadat-Ali,1 A.H. Gullenpet,2 F. Al-Mulhim,2 H. Al Turki,3 H. Al-Shammary,2 A. Al-Elq4 and A. Al-Othman1
كسور الفقرات ذات الصلة بتَخَلْخُل العظام لدى النساء بعد سن اليأس: معدل الانتشار لدى عينة من المملكة العربية السعودية
مير سادات علي، عابد حسين غلاييد، فاطمة الملحم، هيفاء التركي، هادية الشمري، عبد المحسن العلق، عبد الله العثمان
الخلاصـة: هدفت الدراسة للتعرف على معدل الانتشار المرتكز على المستشفيات لكسور الفقرات لدى السعوديات بعد سن اليأس. وقام الباحثون بتقييم صور الصدر الشعاعية للنساء السعوديات اللاتي تزيد أعمارهن على 50 عاماً عند زيارتهن لغرفة الطوارئ في مستشفى الملك فهد الجامعي. وشمل التقييم 785 صورة شعاعية، وأظهر التحليل أن لدى 159 (%18.2) من المريضات 198 كسراً في الفقرات، وبلغ المعدل الوسطي للعمر 65.7 عاماً (بانحراف معياري 8.5). وفي %37.8 فقط من الصور الشعاعية تمت الإشارة إلى الكسور في الفقرات في التقرير الشعاعي، وكان %13.2 من المصابات بكسور في الفقرات يطبقن المعالجة المضادة للارتشاف العظمي في تخلخل العظام.
ABSTRACT The study aimed to determine hospital-based prevalence of vertebral fractures in postmenopausal Saudi Arabian women. Chest radiographs from consecutive Saudi women over the age of 50 years visiting the emergency room at King Fahd Hospital of the University were evaluated. Of 785 radiographs analysed 159 (20.3%) patients had 198 vertebral fractures. The mean age of the women was 65.7 (SD 8.5) years. In only 37.8% of the radiographs with fractures was a vertebral fracture highlighted in the radiologist’s report, and only 13.2% of the women with vertebral fractures were on antiresorptive therapy for osteoporosis.
Fractures vertébrales liée à l’ostéoporose chez la femme postménopausée : prévalence dans un échantillon saoudien
RÉSUMÉ Cette étude visait à déterminer la prévalence en milieu hospitalier des fractures vertébrales chez les femmes saoudiennes postménopausées. On a procédé à une évaluation des radiographies thoraciques de femmes saoudiennes âgées de plus de 50 ans qui s’étaient présentées consécutivement au service des urgences de l’Hôpital universitaire du Roi Fahd. Sur 785 radiographies analysées, on a observé 198 fractures vertébrales chez 159 patientes (18,2 % du total). L’âge moyen des femmes était de 65,7 ans (écart type : 8,5). Pour 37,8 % seulement des radiographies montrant des fractures, le rapport du radiologue mettait en évidence une fracture vertébrale et 13,2 % seulement des femmes présentant des fractures vertébrales étaient sous traitement antirésorbeur contre l’ostéoporose.
1Department of Orthopaedic Surgery; 2Department of Radiology; 3Department of Obstetrics and Gynaecology; 4Department of Internal Medicine, College of Medicine, King Faisal University and King Fahd Hospital of the University, Al Khobar, Saudi Arabia (Correspondence to M. Sadat-Ali:
Received: 05/05/07; accepted: 25/06/07
EMHJ, 2009, 15(6):1420-1425
Introduction
Osteoporosis is a silent skeletal disease which decreases the bone quantity and quality causing fragility fractures. These fractures increase morbidity and mortality in females as well as in males. It is estimated that yearly over 250 000 hip fractures, an equal number of wrist fractures and more than twice that number of vertebral fractures occur in the United States of America (USA) alone [1,2]. Melton reported that 30% of postmenopausal white women in the USA have osteoporosis, of whom 25% have a vertebral fracture [3]. These fractures decrease quality of life, adding to age-related complications with increased morbidity and mortality [4,5]. The economic burden in 1995 in the USA was about US$ 14 billion, which was spent to treat complications of osteoporosis rather than osteoporosis itself [6].
Even though vertebral fractures are described as the hallmark of osteoporosis [7], their diagnosis and management is delayed until a visible limb fracture occurs. Reports in the literature indicate that these fractures are missed by clinicians [8–10] and more remain undetected by radiologists [11,12]. In Saudi Arabia in the past decade osteoporosis has been looked at more as a curiosity than a problem, even though many studies have reported a high prevalence of osteoporosis among Saudi women [13–16].
To our knowledge there are no reports on the prevalence of vertebral fractures in Saudi Arabia and this study was conducted to assess the hospital-based prevalence of vertebral fractures in postmenopausal Saudi Arabian women.
Methods
A review was made of chest radiographs done for female patients over the age of 50 years ordered from the emergency room of King Fahd Hospital of the University in Al-Khobar, between January 2003 and December 2005. Patients who underwent standard posterior–anterior and lateral chest radiography for any reason were included.
During the study period, 10 300 chest X-rays were performed using the Ipac Magic digital archiving system; 18% were in females above the age of 50 years. Radiographs from 880 consecutive patients were studied by 2 independent radiologists (A.H.G. and H.S.). The radiographs were then jointly reviewed with the principle author (M.S-A). The quality of 24 radiographs was not good enough for evaluation and they were discarded. The medical charts of the remaining patients, none of whom had prior history of trauma to the spine, were reviewed. A total of 71 patients were excluded from the study: 21 had malignant disease, 12 had connective tissue disease and 38 were receiving steroids.
The remaining 785 radiographs were reviewed for the presence of vertebral fracture as per the semi-quantitative technique described by Genant et al. [17]. Radiographs were scored as normal (0), mild (1), moderate (2) or severe (3). Mild fracture was one in which the overall height of the vertebra was reduced by 25%, moderate fracture when the overall height of the vertebra was reduced by more than 50% and severe facture was a total collapse of the vertebra. Patients’ demographic data collected from the medical charts included age, basic blood tests, diagnosis and medical treatment.
The data were entered in a database and analysed using SPSS, version 11, with 95% confidence intervals (95% CI) and P-values considered significant at < 0.05.
Results
A total of 785 chest radiographs were reviewed for osteoporosis-related vertebral fractures. A total of 159 (20.3%) patients had 198 vertebral fractures. Age data and blood tests results are shown in Table 1. The mean age of these patients was 65.7 (standard deviation 8.5) years (range 50–91 years). Table 2 shows the prevalence of vertebral fractures according to age groups; 70 (35.4%) of the fractures were in the age group 61–70 years.
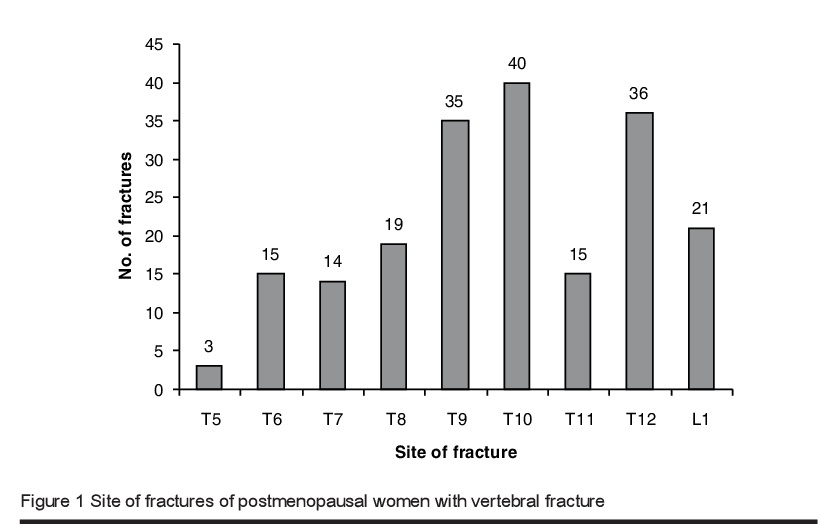
Out of the 159 patients with vertebral fractures, X-ray reports were found in the patients’ records for 82 patients, and only 31 of these (37.8%) had a fracture noted. Figure 1 gives the site and number of fractures: the 9th, 10th and 12th thoracic vertebrae were the most commonly affected. There were 89 (44.9%) mild, 65 (32.8%) moderate and 44 (22.2%) severe fractures. The majority of the patients who had > 1 fracture were over the age of 70 years. The number and severity of fractures were greater in the older group of patients (P < 0.001).
A review of the medical records showed that 51 (32.1%) patients were suffering from cardiovascular disease, 30 (18.9%) respiratory illness, 32 (20.1%) combined cardiovascular and respiratory disease and 7 (4.4%) renal failure. Only 21 patients (13.2%) were on antiresorptive therapy, which means that 138 (86.8%) patients had an osteoporosis-related fracture and were not on treatment for osteoporosis.
Discussion
This is the first hospital-based report on osteoporosis-related vertebral fractures diagnosed by chest radiographs from Saudi Arabia. The prevalence of vertebral fractures in women over the age of 50 years was 20.3%. Concern could be raised on 2 issues; first, that in only 37.8% of the radiographs was a vertebral fracture highlighted in the radiologist’s report and, second, only 13.2% of the women with vertebral fractures were on treatment for osteoporosis. Grazio et al. reported a low prevalence of 9.7% vertebral fractures in an urban population [18]; however other studies from Europe and America put this figure in the range of 16%–25% [3,19–21]. The prevalence of these fractures among Saudi females appears to be within the reported range.
Underdiagnosis of vertebral fractures on plain radiography has been an issue which has been debated for some time now. Delmas et al. reported that on average 45.2% of fractures are missed in North America, 46.5% in Latin America and 29.5% in Europe/South America/Australia [12]. In this study 62.2% of the reported radiographs failed to highlight the fracture but emphasized the findings on the soft tissues of the chest rather than including the skeletal structure as well in their evaluation. Possible reasons for the high percentage of false negative reports in our study compared to reports in the literature could be due to the fact that radiographs were reported by staff at different levels of experience; secondly, junior staff may not have had special training in the diagnosis of vertebral fractures from routine chest radiographs; and, finally, quantitative and semi-quantitative morphometry is a laborious, time-consuming exercise which may not be suitable for reviewing the films requested for emergency room patients.
Early diagnosis of osteoporosis-related vertebral fracture is important as there is a 5–10-fold increased risk of a second fracture within a year [22,23] and a 2-fold increase in hip fracture, with the resulting increase in morbidity and mortality [24]. Apart from other serious complications, patients with vertebral fractures suffer from nagging back pain, fracture-induced kyphotic deformity and progressive disability. The reduced physical activity due to chronic pain probably makes them more osteoporotic and, without proper diagnosis and adequate treatment, the situation becomes worse. Another issue we found in this study which needs to be addressed is that only 13.2% of the patients were on treatment for osteoporosis. This indicates that women who already have an osteoporotic-related vertebral fracture were neither diagnosed with the disease nor given any treatment.
This retrospective study had some limitations. Evaluation of the chest radiographs of patients attending the emergency room might be biased: it is possibile that some of the cases presenting with chest pain may in reality be due to osteoporosis-related vertebral fracture. Secondly, the radiologists who reviewed the radiographs for the study were specifically looking for vertebral fractures rather the soft tissues of the chest.
In conclusion, this study highlights some deficiencies in our system. While the prevalence of vertebral fractures found in this Saudi Arabian sample (18.2%) was similar to some Western countries, it still shows that we are complacent in dealing with the problem of osteoporosis. Secondly, there was delay in the diagnosis of the osteoporosis-related fractures and treatment. Thirdly, we had no definitive plan to train our staff to identify these fractures on a routine basis. The Saudi Arabian population is ageing, and the increasing number of elderly people is bound to have an impact on health care budgets in the future. It is time now to act prudently with the available resources to diagnose osteoporosis early and treat it appropriately in addition to encouraging the population to modify their lifestyles to reduce the incidence of fractures through exposure to sunlight, consumption of vitamin-D-fortified foods and weight-bearing exercise.
References
- Osteoporosis prevention, diagnosis, and therapy. Consensus statement/National Institutes of Health consensus development conference, 2000, 17:1–36.
- Riggs BL, Melton LJ III. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone, 1995, 17(Suppl. 5):505S–11.
- Melton LJ III. Epidemiology of spinal osteoporosis. Spine, 1997, 22(24 Suppl.):2S–11S.
- Cauley JA et al. Risk of mortality following clinical fractures. Osteoporosis international, 2000, 11:556–61.
- Kado DM et al. Vertebral fractures and the mortality in older women. Archives of internal medicine, 1999, 159:1215–20.
- Ray NF et al. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. Journal of bone and mineral research, 1997, 12:24–35.
- Nevitt MC et al. The association of radiologically detected vertebral fractures with back pain and function: a prospective study. Annals of internal medicine, 1998, 128:793–800.
- Gehlbach SH et al. Recognition of osteoporosis by primary care physicians. American journal of public health, 2002, 92:271–3.
- Probst JC et al. Osteoporosis recognition: correcting Gehlbach et al. American journal of public health, 2002, 92:1885.
- Morris CA et al. Incidental vertebral fractures on chest radiographs, recognition and documentation and treatment. Journal of general internal medicine, 2006, 21(4):352–6.
- Gehlbach SH et al. Recognition of vertebral fracture in a clinical setting. Osteoporosis international, 2000, 11:577–83.
- Delmas PD et al. Underdiagnosis of vertebral fractures is a worldwide problem: The IMPACT study. Journal of bone and mineral research, 2005, 20(4):557–63.
- Sadat-Ali M et al. Bone mineral density among postmenopausal Saudi women. Saudi medical journal, 2004, 25:1623–5.
- El-Desouki MI. Osteoporosis in postmenopasual women using dual X-ray bone densitometry. Saudi medical journal, 2003, 24:953–6.
- Sadat-Ali M, Al Elq AM. Male osteoporosis among Saudi Arabian population: a pilot study. Annals of Saudi medicine, 2006, 26:450–4.
- Sadat-Ali M, Al-Habdan I, Marwah S. Bone mineral density measurement of distal radius in Saudi Arabian females. Annals of Saudi medicine, 1996, 16:414–6.
- Genant HK et al. Vertebral fracture assessment using a semi-quantitative technique. Journal of bone and mineral research, 1993, 8(9):1137–48.
- Grazio S, Korsić M, Jajić I. Prevalence of vertebral fractures in an urban population in Croatia aged fifty and older. Wiener klinische Wochenschrift, 2005, 117(1–2):42–7.
- Majumdar SR et al. Incidental vertebral fractures discovered with chest radiography in emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Archives of internal medicine, 2005, 165(8):905–9.
- Grados F et al. Prevalence of vertebral fractures in French women older than 75 years from the EPIDOS study. Bone, 2004, 34(2):362–7.
- Díaz López JB et al. Prevalencia de fractura vertebral en población asturiana mayor de 50 años de acuerdo con diferentes criterios radiológicos [Prevalence of vertebral fracture in the population older than 50 years in Asturias (Spain) defined following different radiological criteria]. Medicina clínica, 2000, 115(9):326–31.
- Lindsay R et al. Risk of new vertebral fracture in the year following a fracture. Journal of the American Medical Association, 2001, 285:320–3.
- Delmas PD et al. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone, 2003, 33(4):522–32.
- Black DM et al. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. Journal of bone and mineral research, 1999, 14:821–8.








