R.M. Smadi,1 B.Y. Smadi2 and A. Ka’abneh3
Introduction
Eritrea is situated on the east coast of Africa, bordering Sudan, Djibouti and Ethiopia. It is hot and dry in the desert strip along the Red Sea coast, cooler and wetter in the central highlands, and semi-arid in the western hills and lowlands, with the heaviest rainfall during June to September, except in the coastal desert.
Since settlement of the conflict between Eritrea and Ethiopia in 2000, a United Nations peacekeeping mission has been present in the area and the troops have faced a number of medical problems specific to the area.
We present an outbreak of 74 cases of an acute blistering skin reaction in a military unit serving in Eritrea. This reaction followed exposure to the secretions of a flying insect that is prevalent in hot tropical areas.
Case series
During the period July 2002 to January 2003, 74 patients visited military clinics in 3 different locations in the western sector of Eritrea (Barintu, OmHajar and Shambiko) with acute blistering skin lesions. All the patients were otherwise healthy, male soldiers (age range 23–48 years) with no significant past medical history. All were seen in the first 72 hours after the injury and followed up for 2–4 weeks until complete healing of the lesions. A detailed clinical history was obtained, which included the time of injury, the onset of symptoms, the characteristics of the lesion (site, size, number, associated symptoms, natural history) and the primary actions taken by the patient.
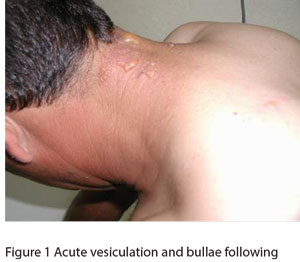
Most of the patients had 1 or 2 lesions and more than three-quarters of these were in exposed parts of the body (neck, upper limb and upper chest) (Table 1). The clinical severity of the lesions varied from patient to patient (Figures 1 and 2). In most cases the reaction started as redness with acute vesiculation that proceeded to bullae formation in the following hours, with a burning sensation and sometimes pain. Most lesions (85%) had completely healed within 1 week. One patient had residual postinflammatory hyperpigmentation (Figure 2), and another had secondary bacterial infection, which was successfully treated by topical and systemic oral antibiotics.

Patients observed that the reaction followed contact with an unidentified flying insect although there was no sensation of a sting at the time of injury. The most effective treatment was to wash the site of contact with tap water if the patient noticed the insect on the skin; this resulted in only mild or no erythema. Other treatments included cold wet compresses, drying soothing agents (calamine lotion), steroid creams, antibiotics (topical and systemic), antihistamines, emollients and barrier creams.
Insect description
The insect was described as fluorescent green metallic in colour, about 10 mm in length and 3 mm wide (Figure 3). Its main time of activity was observed to be the daytime, mainly between 10:00 and 18:00 hours. It was noticed that the insect curls around itself when attempts are made to kill it. Observations suggested that it did not sting or bite but secreted a white material from its rear, which caused irritation and blistering within hours of exposure. The pH of the secreted material, measured by Combur-Test urine test strips (Roche), was around 5, which corresponds with the popular name of this insect among the soldiers: acidic fly.
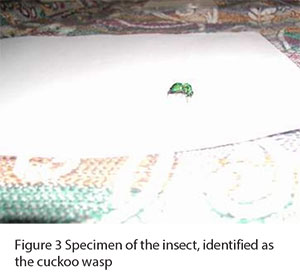
The insect was identified as most probably the cuckoo wasp (Hymenoptera. Suborder: Apocryta. Superfamily: Chrysidoidea. Family: Chrysididae). It lives mainly in the area bordering Ethiopia and Sudan and is not found in Asmara due to its inability to live in high altitude areas. Most of our cases occurred between July and October, which is the active season of the wasp. When these wasps are disturbed, they curl their body into a ball with the wings protruding from the sides, which may be a way of feigning death as a protection mechanism [1]. The adult wasps do not sting [2], which corresponds with our patients’ symptoms of burning and erythema, and rarely cause actual pain.
Discussion
All our patients were soldiers, and most cases occurred during the day time when the wasp is active and most of the soldiers are moving around. When the wasp comes into contact with skin it secretes a white, acidic vesicant substance that initiates an acute contact irritant dermatitis similar to that caused by the secretions of insects of the genus Paederus [3]. The extent of the skin reaction seems to depend on the time and duration of exposure, which accounts for the variation in the clinical severity of the lesions from one patient to another. The acidic pH of the insect secretion is likely to be the trigger for the irritant reaction [4].
The insect responsible for the lesions was believed to be the cuckoo wasp. A previous study in the same area by Al-Basheer, Hijazi and Dama recorded a similar outbreak of skin reactions [5], but this was thought to be caused by beetles and not wasps.
Despite initial concerns about the lesions, they were found to be easily treated if noticed early. Complications were rare, except for 1 case of residual postinflammatory hyperpigmentation, which is common after acute skin reactions [6], and 1 case of secondary bacterial infection. Fast healing of the lesions was greatly dependent on primary action being taken immediately after contact (washing with water).
It is important to be aware of unusual environmental hazards in areas where soldiers will serve in order to educate them about the potential hazards specific to the area.
Acknowledgement
We would like to thank Dr Ahmad Katebeh, Associate Professor, Entomology Department, Agriculture College, Jordan University, for his help in identification of the insect.
References
- Lyon WF. Nuisance parasitic wasps. Ohio State University extension fact sheet. HYG-2113-95 [online fact sheet] (http://ohioline.osu.edu/hyg-fact/2000/2113.html, accessed 18 January 2009).
- Insects and their allies. Hymenoptera: ants, bees and wasps. Victoria, Australia, Commonwealth Scientific and Industrial Research Organization [online fact sheet] (http://www.ento.csiro.au/education/insects/hymenoptera.html, accessed 18 January 2009).
- Sendur N, Savk E, Karaman G. Paederus dermatitis: a report of 46 cases in Aydin, Turkey. Dermatology, 1999, 199(4):353–5.
- Arthropod bites and stings. In: Fitzpatrick TB et al., eds. Dermatology in general medicine, 4th ed. New York, McGraw–Hill, 1993:2823–5.
- Al-Basheer M, Hijazi M, Dama T. Blister beetles dermatosis: a report of 43 cases in a military unit in Eritrea. Journal of the Royal Medical Services, 2002, 9(2):40–3.
- Irritant contact dermatitis. In: Burton JL, Burns DA, Breathnach SM, eds. Rook textbook of dermatology, 6th ed. Volume 1. Oxford, Blackwell Science, 1998:730–1.








