A. Humayun1
ABSTRACT In October 2005, northern Pakistan was devastated by an earthquake killing 73 000 people. Some of the seriously injured were airlifted to a tertiary hospital in Rawalpindi, near Islamabad. This field report describes the psychiatric services delivered at that hospital. It explains how the needs were assessed and psychosocial interventions designed at different levels. The training needs of the medical staff were also identified and efforts were made to enhance their skills for psychosocial care. Finally, the report formulates some recommendations for improving such services.
Tremblement de terre en Asie du Sud : le cas de la psychiatrie dans un hôpital de soins tertiaires
RÉSUMÉ En octobre 2005, le nord du Pakistan a été dévasté par un tremblement de terre qui a fait 73 000 morts. Certains des blessés les plus graves ont été évacués par voie aérienne vers un hôpital de soins tertiaires à Rawalpindi, près d’Islamabad. Ce rapport de terrain décrit les services psychiatriques fournis dans cet hôpital. Il expose la méthode d’évaluation des besoins et de conception des interventions psychosociales à différents niveaux. Les besoins en formation du personnel médical ont également été définis et des mesures ont été prises pour renforcer les compétences de ce personnel en matière de prise en charge psychosociale. Enfin, le rapport présente un certain nombre de recommandations visant à améliorer ces services.
1Institute of Psychiatry, Rawalpindi General Hospital, Rawalpindi, Pakistan (Correspondence to A. Humayun:
Received: 05/03/06; accepted: 17/08/06
EMHJ, 2008, 14(5): 1205-1216
Introduction
The need for psychosocial care for populations exposed to disasters is well established [1]. Studies of the impact of disasters in developing countries focus on assessing needs and developing mental health interventions in primary care [2]. Although there is some evidence in the literature about developing emergency services in hospital settings following disasters [3], such experiences are rarely reported from the developing countries. The following is an account of assessment of psychosocial needs of earthquake victims in a tertiary hospital and a description of interventions designed to deal with such needs.
On 8 October 2005, a fierce earthquake (7.6 on the Richter scale) reduced the northern area of Pakistan to rubble. At least 73 000 people died and another 70 000 were severely injured [4]. The collapse of health care facilities added to the complexity of the relief operation. Emergency medical camps were set up in affected areas. More seriously wounded victims were airlifted to the nearest city hospitals, one of which was Holy Family Hospital (650-bed teaching hospital) in Rawalpindi where a state of emergency was declared. Our team, consisting of a psychiatrist and 3 trainees, started working in the hospital a week after the earthquake and provided on-site cover for 3 weeks. Our objectives were to:
- Assess needs
- Support the surgical teams
- Enhance their capacity to intervene/ communicate effectively
- Impart basic counselling skills to doctors
- Provide psychological care for the victims
- Identify high-risk groups for psychiatric intervention.
The following field rep describes our experience of clinical service and training of medical staff during this disaster.
Providing clinical services
In the first 4 weeks, nearly 1800 victims attended the Accident and Emergency Department of Holy Family Hospital, 994 of whom were admitted to the hospital. The rate of admission (maximum 151 in 1 day) and therefore the turnover was extremely rapid. Accordingly, a large number of patients had to be discharged to other health care facilities soon after surgery to accommodate the rapid influx. Thus 187 patients had already been discharged in the first week, so 807 patients were assessed. The surgical wards accommodated 120 patients and the rest were admitted to other wards supervised by the surgical teams.
In addition to basic support for all victims (807), we identified vulnerable patients who required more focused psychological interventions and those with pre-existing mental illnesses who needed treatment. The following indicators were developed to identify a vulnerable group.
- Those who were unattended by family or friends
- Those with severe losses, e.g. amputations/multiple loss in the family
- Those appearing unwell (not sleeping, not eating, not speaking or extremely distressed) (3 or more symptoms)
- Those complaining of excessive pain or having poor compliance.
Those identified as vulnerable were assessed in detail. They were reviewed 4–6 times each. The average duration of a visit was about 10 minutes. All interventions were recorded. Using the key indicators, 141 (17.5%) victims were identified in the vulnerable group, 17 of whom were actually attendants of injured victims. Of these, 97 (68.8%) were female. The youngest victim was 2 years of age and the oldest was 84 years, mean age 27.52 (SD 15.88) years. Table 1 shows the number of victims identified for each indicator.
The losses noted in the vulnerable group are shown in Table 2. Table 3 shows the 6 most common symptoms identified in the vulnerable group. Over half suffered from disturbed sleep and sadness. Just over 60% of the vulnerable group received an ICD10 diagnosis [5] (Table 4), the commonest being grief reactions (35.5%).
Table 5 gives a summary of the interventions carried out. These included:
- Basic psychological support [2]. This included listening with empathy, ventilation and reassurance.
- Grief counselling [2]. This addressed the loss and the pre-disaster relationship with the deceased, exploring personal meaning of the loss and encouraging mourning rituals.
- Problem solving [2]. This addressed social issues such as establishing contact with the families or reuniting them.
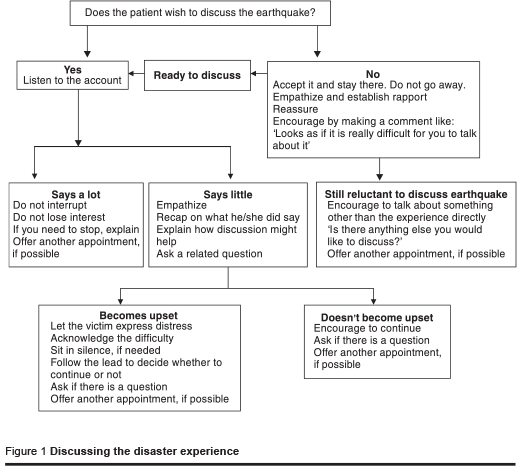
- Discussing the disaster experience. A cultural view discourages active discussion about traumatic experiences in order to protect the sufferer from further distress. The difficulty was more marked for children and young adults where they appeared to seek (nonverbal) permission from the parents even when they were keen to discuss their experience. At the same time, patients were not in any way forced to recollect events if they did not wish to [6]. Figure 1 summarizes this intervention.
- Working with the families. This included basic support for them, improving communication, encouraging discussion of concerns and assisting them in dealing with the patient’s distress.
- Breaking bad news [7]. The cultural way of dealing with such tragedy is that families withheld information from the seriously injured about their losses. Some injured were rescued from the rubble after days and were airlifted directly to the hospital. Therefore, they were unaware of the safety of other family members. An injured mother was not informed of the death of her 19-year-old daughter even after 3 weeks.
- Dealing with disability. This included pre-operative and post-operative counselling for amputation or severe injuries where the patient was disabled/dependant for a protracted period.
As regards psychotropic prescription, benzodiazepines were advised for 15.7% of the vulnerable group, all seen by the consultant psychiatrist. Clinical guidelines were developed for doctors regarding prescription of benzodiazepines (Table 6).
In the third category of liaison interventions, the most difficult aspect was pain management. By the third week, many patients were receiving parenteral opioid analgesic (18 out of 58 on one ward). Once prescribed, the injections were purchased by the families without being aware of the risk of dependence. Following this observation, a protocol was developed for pain management in collaboration with the surgeons.
The protocol for pain management was as follows.
- Review analgesia: check compliance, increase dose, change the drug.
- Explore psychosocial difficulties.
- Help the patient link pain with distress.
- Discuss further intervention with the consultant surgeon.
If synthetic opioids were considered:
- Consultants only should advise.
- Risk of dependence should be explained.
- Name of the drug should not be written down for the family to purchase (it should be available in the hospital).
- Opioid should be prescribed for a limited period only and then reviewed.
- Patient should never be discharged on synthetic opioid analgesia without arranging follow-up.
Based on our experience at Holy Family Hospital, the psychosocial interventions were delivered at 3 levels (Box 1).
Training of medical staff
It was quite difficult to coordinate training of doctors partly because surgical teams were overwhelmed with work and partly because they felt that the job was best left to mental health professionals.
The following training strategies were used: group discussions; “hands-on” bedside training; clinical supervision; joint rounds with surgeons.
The objective was to provide support; assess needs for training; impart basic knowledge about psychosocial issues; and enhance skills of communication and basic psychological support.
These discussions lasted for 1–2 hours. They were not structured and informal interaction was encouraged. The junior doctors participated better when the respective consultants were present. Although surgical teams were much more overworked and physically exhausted than those who were providing cover on other wards, the level of stress and dissatisfaction was much higher in the latter group who felt that the clinical supervision and coordination was inadequate and not organized.
“Hands-on” training, although timeconsuming, was rated as the most useful strategy by the medical students and doctors. As they identified a difficult situation, they sought advice/supervision at the bedside. These interventions were brief and focused, lasting on average 10 minutes, and were either supervised or demonstrated on the spot. In most cases, the situation was jointly reviewed at least once more.
As regards clinical supervision, initially even trainees in psychiatry faced many difficulties as the situation was so different from routine clinical work. So, joint assessments were done. Daily meeting was held to review difficulties. If there were doubts after discussion, then intervention was supervised (“hands-on” training).
In view of the enormity of clinical work, joint rounds with surgeons were brisk (each patient was reviewed in a few minutes) but major decisions were made. This opportunity was valuable as most members of the clinical team were present during the discussions. Although surgeons seemed aware of psychological aspects of patient care, they generally remained reluctant to demonstrate it. Their explanations included comments like: “My primary concern is the wound”; “I do not have the time to discuss these minor issues”; “My house surgeon will later speak to the patient”; “I understand it should be done but I am not sure how to do it”; and “We do teach all this to our trainees when they present cases in conference rooms”.
Difficulties faced
General difficulties
Most doctors highlighted “unpreparedness” for disaster management in terms of their training and organization of the services. Surgical teams were trained to deal with trauma to some degree but others felt that the challenge was way beyond their capacity. In addition, most doctors felt affected by the disaster itself. The range of emotional experiences included:
- Fear: that they could have been affected adversely themselves or that the roof might still collapse during the after shocks
- Sadness: about the extent of the damage and degree of loss
- Guilt: about being safe/for not being able to do enough/for not being able to spend time with their own families
- Anger: about the scarcity of resources/ poor organization/lack of supervision/ administrative decisions.
Medical students appeared particularly vulnerable as they tended to become overinvolved with victims, did not want to leave them and felt guilty for not being able to resolve their needs; some even wanted to follow up the victims after discharge.
Clinical difficulties
Limited communication skills
Communication with patients could be a difficulty even for simple procedures like exploring details of the injury experience, explaining procedures, satisfying family, etc.
Dealing with psychological issues
Junior doctors and medical students expressed their reluctance or inability to deal with adverse emotional reactions. Most preferred to avoid severely grieved or angry people and focused on physical aspects of wound care.
Pain relief
A major management issue were patients who “demanded” excessive pain relief, which appeared out of proportion to the clinical condition. In such cases, doctors increased the dose or added more analgesics. If this did not help, they resorted to synthetic opioid analgesics which “worked”.
Use of psychotropic medication
Even the senior doctors were unsure about the rational prescribing of benzodiazepines for symptomatic use. The most commonly asked question was “when to decide that someone should be given a tablet?”
Administrative difficulties
Multidisciplinary approach
The need for organized team work and better clinical coordination was repeatedly highlighted. There were at least 3 surgical specialists involved in the care of each patient (orthopaedic, general surgeon and plastic surgeon) and a fourth one (a physician or psychiatrist) in some cases. Most experts seemed to work in isolation, quite oblivious to other plans. Poor documentation did not help. The junior doctors were mostly occupied carrying out round orders and organizing operation lists. A difficult situation arose when a surgeon planned for amputation on a child. The junior doctor was uncomfortable, feeling that the mother was not prepared at all. She was optimistic about wound healing, a view also held by the doctor involved in daily dressings. In view of the confusion, counselling was postponed until the plan was clarified. Shortly thereafter, a consultant reviewed the case and confirmed that amputation was not needed.
Limited resources
In addition to a dearth of trained personnel, there were many resource-limiting and social difficulties, such as tracing and reuniting families, unattended and inappropriately attended patients, overwhelming social needs. The hospital was well stocked with medicines and other necessary items (syringes, dressings) but still a paediatrician was desperate for tetanus toxoid for a 5-year-old child. The ward doctor spent the night calling different chemists to locate it. Staff was inadequate to meet nursing and toileting needs of patients who were attended by family members of the opposite sex. It was noted that some patients avoided solid food to control bowel movements.
Discharge policy
In view of the need for rapid turnover, abrupt discharge decisions were made by the administration. As a result, newly operated patients were shifted to a makeshift facility or a peripheral hospital with lesser expertise. Doctors found it difficult to explain such decisions to patients and their families. A consultant faced some angry patients and decided not to undertake this job himself. So, either junior doctors ended up coping with a highly distressing situation or nurses just wheeled patients to the reception, where they discovered that they were being shifted to another city/medical camp/hospital. In more than one incident, junior doctors refused to discharge a critical patient and faced threats from the administration of losing their jobs.
Discussion
Perhaps we could be more prepared in dealing with the psychosocial difficulties than we currently are [8].
Like many other natural disasters, the earthquake in Pakistan was a unique experience of dealing with immense distress where the complexity of the situation far outweighed the resources. Since the needs were very different from routine clinical presentations, strategies had to be developed promptly and then implemented in a resource-limited setting. In our experience, the environment was challenging: psychosocial services were being offered and not sought, there was a general lack of awareness and sensitivity by the medical staff towards psychosocial services, wards lacked the basic provisions for psychological interventions (privacy, silence, etc.). In addition, the existing guidelines [9,10] for providing such services or training doctors were quite inadequate.
Some involved with health care of the earthquake victims at Holy Family Hospital might justify the ethical lapses because of pressure of work or urgency of the situation. Whether it is a valid excuse for ignoring basic principles of medical ethics [11] is yet to be decided. The foremost concern is about respecting the autonomy of the patients, which means giving as much information as they want, making decisions for them with deliberation, maintaining confidentiality, never deceiving them, etc. Let us consider an example of informed consent. In most cases, families received hurried and inadequate explanation about treatment plans and it was left to them to discuss it with the patient. Many patients were uncertain whether it would be appropriate to ask questions. Of the 9 patients who underwent amputation, only 5 knew about it when they woke up. Privacy of patients was seriously compromised. Although efforts were made to admit patients of the same sex in one ward, most places had both men and women together. There were no screens in the wards and patients were indecently exposed for examination, dressings, wounds, etc., thus causing deep embarrassment.
The responsibility for the discharge policy lay more at the level of the institution and less on individuals. Many seriously injured received medical attention which was already delayed. Then they were prematurely and forcibly discharged. Some were struggling to locate their families or vice versa and further movement caused serious difficulties. There were no satisfactory selection criteria for deciding which patients were to be discharged (sometimes clinicians were not even consulted, the administration made the decision). The destinations were away in other cities and not always to adequate health facilities. These were not discussed with the patients and when they objected, information was withheld until they were forced into an ambulance.
There are limitations to this report. It is mostly based on observations and there is no evidence to determine whether the conditions and difficulties mentioned here reflect the normal situation or occurred solely as a result of the emergency. It was written up in hindsight, so victims and medical staff were not aware that the information would be used and their permission has not been sought. Also, our sample excludes specific groups such as unattended children or those with spinal injuries/paraplegia, who were shifted to other hospitals with appropriate facilities. In view of our limited team, the sample of the vulnerable group might also be an underestimate.
Adhering to the key principles outlined for services for mental health in emergencies [1], the following are recommendations for preparing tertiary hospitals.
Multi-disciplinary approach for health care. WHO strongly recommends access to mental health services for affected populations. In a resource-poor country where specialized services are scarce, a system-wide public health approach rather than trauma focused interventions is required [12]. The need to strengthen mental health services in primary care in the affected areas is well established [13]. Following a similar holistic approach, mental health professionals should be integrated as part of the trauma teams in tertiary hospitals as well.
Re-organization of services. The services in tertiary hospitals are specialitycentred and not patient-centred. Following a disaster, there is an immediate need for reorganizing services. All available health professionals should be integrated into trauma teams. Other specialists like physicians form a huge resource of trained medical staff that might remain under-used in emergencies primarily requiring surgical skills or vice versa. Such staff could easily be trained to: assist primary (trauma teams, in our case) teams; manage the general health of the victims; provide psychosocial interventions; and liaise with the administration/other agencies (e.g. voluntary workers, social services). The roles should be clearly defined for improved patient care and an effective referral system needs to be developed for complex cases and for organizing aftercare.
General awareness and education. There is widespread ignorance about the psychosocial needs of affected populations and the basic principles of mental health care, not just in the community but also amongst the health professionals. Within the hospital setting, there is need to educate the staff (administrative, medical, nursing and paramedical) and the general public. For this reason appropriate manuals for training hospital staff and leaflets for the general public [14] must be prepared.
Application of principles of medical ethics and psychosocial approach in policy decisions. Mental health professionals should work in close collaboration with the administration and the clinical teams to develop clear policy outlines for psychosocial health care. Specific cultural concepts need to be addressed. Some examples include:
- During evacuation of casualties from the affected areas, the vulnerable population (children, women, elderly and disabled, etc.) must be accompanied.
- A discharge policy must be in place, including the need for reliable documentation for tracking patients and clear information for families.
- Support groups for health care workers should be established to maintain staff morale.
- Tasks like distribution of the relief goods or food in the hospital should be planned carefully in order to maintain dignity of the victims.
Ongoing training. In view of limited specialized personnel (even in a teaching hospital in a major city), training of doctors in psychosocial aspects of health care needs to be emphasized, both in the short term and in the longer term. The objectives should be: to increase awareness of and educate about psychosocial issues; to develop appropriate skills for effective communication and psychological interventions; and to bring about a positive change in attitude of doctors.
In short term, the training should be brief, focused and supervised. In the longer term, the disaster experience has revealed the need for enhancing specialised services, developing human resources skilled in non-biological interventions and integrating psychosocial aspects into the existing biological approach of health care both at undergraduate and postgraduate levels of training.
Research and evaluation. Traditionally, standards of care are not developed or followed in resource-poor countries like Pakistan. Charismatic leaders tend to set up successful services/practices which are difficult to duplicate or monitor. Generally there is a great enthusiasm to deliver immediate services following a disaster, both at the national and international level. Whether the interest and services sustain and deliver ongoing care remains to be proved. Some suggestions are:
- To develop effective information systems so that the emergency data are preserved.
- To formally assess needs of the disaster victims so that resources are appropriately allocated and used.
- Once the needs are identified, to develop clear protocols at the earliest (e.g. for pain management and psychotropic prescriptions).
- To determine key indicators (focusing on care and rehabilitation) to be used for monitoring and evaluation.
Acknowledgements
This report is dedicated to the 4 million people whose lives have been shattered by the earthquake.
I would like to thank Professor Michael Herbert for his valuable support during my work with victims and for reviewing the draft. I am also grateful to Dr Mark Van Ommeren for his encouraging comments and Dr Bushra Razzaque for her commitment in collecting data.
References
- Mental health in emergencies: psychological and social aspects of health of populations exposed to extreme stressors. Geneva, World Health Organization, 2003.
- Manual for community level workers to provide psychosocial care to communities affected by the tsunami disaster. New Dehli, World Health Organization Regional Office for South-East Asia, 2005.
- SARS outbreak in the Greater Toronto Area: the emergency department experience. Canadian Medical Association Journal, 2004, 171 (11):1342–44.
- 2005 Earthquake Preliminary Damage and Needs Assessment. Asian Development Bank and World Bank in coordination with Government of Pakistan, November 12, 2005 (http://www.pakistan. gov.pk/divisions/economicaffairs-division/media/Pakistan-Damage-and-Needs-Assessment.pdf, accessed 25 March 2008).
- The ICD-10 Classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. Geneva, World Health Organization, 1992.
- Single-session psychological debriefing: not recommended. Geneva, World Health Organization (http://www.who.int/hac/ techguidance/pht/13643.pdf, accessed 25 March 2008).
- Fallowfield L, Jenkins V. Communicating sad, bad and difficult news in medicine. Lancet, 2004, 363:312–9.
- Sphere Handbook. Humanitarian charter and minimum standards in disaster response. Geneva, Sphere Project. 2004.
- Weine S et al. for the Task Force on International Trauma Training of the International Society for Traumatic Stress Studies. Guidelines for international training in mental health and psychosocial interventions for trauma exposed populations in clinical and community settings. Psychiatry, 2002, 65(2):156–64.
- Psychosocial and mental health interventions in areas of mass violence. Geneva, Médecins Sans Frontières, 2005.
- Gillon R. Medical ethics: four principles plus attention to scope. British medical journal, 1994, 309:184–8.
- Ommeren MV, Saxena S, Saraceno B. Mental and social health during and after acute emergencies: emerging consensus? Round Table. Bulletin of the World Health Organization, 2005, 83(1):75–6.
- The effectiveness of mental health services in primary care: The view from the developing world. Geneva, World Health Organization, 2001.
- Mental health and psychosocial support: Information for aid workers in Kashmir in October 2005. (http://www.reliefweb. int/rw/rwb.nsf/db900sid/EVOD-6H9GAS? OpenDocument&query=Information%20f or%20aid%20workers%20in%20kashmir accessed 29 June 2008).








