T. Dogru,1 A. Sonmez,1 I. Tasci,1 G. Yagci2 and M.R. Mas1
1Department of Internal Medicine; 2Department of Surgery, Gulhane Medical School, Ankara, Turkey (Correspondence to I. Tasci:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
Received: 18/01/06; accepted: 27/03/06
EMHJ, 2008, 14(3):742-744
Introduction
Appendicitis caused by Mycobacterium tuberculosis is extremely rare and its presentation is atypical [1]. We describe a patient with peritoneal tuberculosis (TB) and perforated tuberculous appendicitis, who was investigated for vague abdominal distention and weight loss. The presentation of types of TB of the appendix and the role of cancer antigen-125 (CA-125) in the diagnosis and follow up of gastrointestinal TB are discussed.
Case report
A 48-year-old man was admitted to the Department of Internal Medicine, Gulhane School of Medicine in September 2003. He had a 2-month history of fatigue, anorexia, marked weight loss and progressive abdominal swelling. His medical history was unremarkable. The physical examination showed paleness of the conjunctiva and skin, and diffuse non-tender abdominal distention.
Abnormal laboratory results were: haemoglobin 10 g/dL, erythrocyte sedimentation rate 80 mm/h, eosinophil count 16%, and serum CA-125 196 U/L (normal < 35 U/L). Urine and sputum TB cultures and tuberculin skin test were negative. Chest roentgenogram was normal. Abdominal ultrasonography showed extensive ascites and septations but no masses. Computed tomography did not reveal any additional findings.
Ascites was haemorrhagic in appearance and the following results were found: white blood cell count 0.4 × 109/L (80% lymphocytes), glucose 41 mg/dL, total protein 5.4 g/dL, albumin 2.5 g/dL and amylase 10 U/L. The serum/ascites albumin gradient was 1. The following tests in the ascites fluid were also negative: microbiological analysis including acid-fast bacilli, polymerase chain reaction test for M. tuberculosis, and cytological examination.
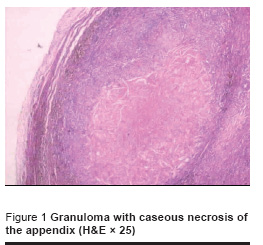
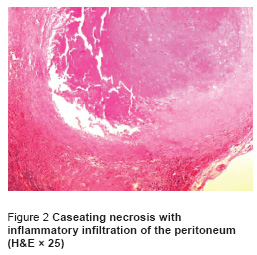
Upper gastrointestinal endoscopy and colonoscopy were normal. Exploratory laparotomy disclosed massive haemorrhagic ascites, and a thickened, inflamed and adhesive peritoneum. The appendix was perforated and a plastron was observed. Multiple biopsies were obtained, and omentectomy, debridement and appendectomy were performed. Histological examination of the specimens from the appendix and peritoneum revealed numerous caseating granulomas with acid-fast bacilli (Figure 1 and Figure 2).
The patient was diagnosed with gastrointestinal TB and underwent 2 months intensive treatment with 4 antituberculous drugs (isoniazid 300 mg, rifampin 600 mg, ethambutol 1000 mg and pyrazinamide 2000 mg daily) followed by a 4-month course of isoniazid 300 mg and rifampin 600 mg daily. Serum CA-125 levels returned to normal at the end of the third month of therapy (18 U/L). He adhered fully to the treatment. The drugs were well tolerated and no side-effects were observed during the entire course of therapy. During the 12-month follow-up all complaints of the patient resolved, he gained weight and no ascites was detected.
Discussion
Tuberculous appendicitis is an extraordinary clinical condition, which is more prevalent in regions with endemic TB [1]. When a site of infection is detected elsewhere in the body, the case is named as “secondary” tuberculous appendicitis; otherwise the condition is called “primary” tuberculous appendicitis.
Our patient had tuberculous peritonitis accompanied by perforated appendix proven by biopsy to be TB. Because of this coincidence it is not easy to determine whether this was a complicated case of primary tuberculous appendicitis or the appendicitis occurred secondary to tuberculous peritonitis. Tuberculous appendicitis usually presents a nonspecific clinical picture such as mild intermittent right iliac pain or is diagnosed incidentally after a latent asymptomatic period [2]. Therefore, tuberculous appendicitis secondary to peritoneal TB seems to be more likely in our case.
Culture of the ascitic fluid, sputum and urine for TB as well as the tuberculin skin test were all negative, and the chest X-ray was normal. Thus, diagnosis of TB could only be established by detection of caseating granulomas and acid-fast bacilli in the appendix and peritoneum. Difficulties in demonstrating the bacilli have been reported and histopathological examination may offer a more definite diagnosis in gastrointestinal TB [3].
The presence of high CA-125 levels also strengthened the diagnosis of TB in our patient. CA-125 is a high molecular weight glycoprotein, which is mostly used as a marker for the diagnosis of gynaecological and non-gynaecological malignant disorders and relapses [4]. Moreover, we and others have demonstrated that serum CA-125 can also increase in tuberculous peritonitis and will decrease and even normalize with anti-TB therapy [5]. Indeed, serum CA-125 levels in our patient returned to normal after 12 weeks of treatment. Thus, current data indicate that determination of serum CA-125 concentration can be used in tuberculous peritonitis, not only to make an accurate diagnosis and ascertain the activity of the disease but also to follow the response to treatment.
In conclusion, we report an atypical presentation of a perforated tuberculous appendicitis accompanying peritonitis. TB, a highly prevalent disease in low-income countries, can mimic many other chronic diseases, and should always be considered in patients with abdominal pain of undetermined origin.
References
- Singh MK, Arunabh V, Kapoor VK. Tuberculosis of the appendix. A report of 17 cases and a suggested etiopathological classification. Postgraduate medicine journal, 1987, 63:855–7.
- Askari A, Coventry P, Perks WH. Primary tuberculous appendicitis. Postgraduate medicine journal, 1993, 69:411–2.
- Uygur-Bayramicli O, Dabak G, Dabak R. A clinical dilemma: abdominal tuberculosis. World journal of gastroenterology, 2003, 9:1098–101.
- Bergmann JF et al. Elevation of CA-125 in patients with benign and malignant ascites. Cancer, 1987, 59:213–7.
- Mas MR et al. CA-125: a new marker for diagnosis and follow-up of patients with tuberculous peritonitis. Digestive and liver disease, 2000, 32:595–7.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)