N.Y. Abou El-Enein1 and M.A. Abolfotouh2
تدقيق على رعاية السكري في ثلاثة مراكز في الإسكندرية
نجوى يونس أبو العينين، مصطفى عبد الفتاح أبو الفتوح
الخلاصـة: للتدقيق على الخدمات المقدمة للسكريين في ثلاثة مراكز في الإسكندرية تم اختيار ثلاثة مؤشرات هي البنية والإجراءات والحصائل. وقد كانت البنية سيئة، ومن مشاكلها الرئيسية عدم وجود نظام للمواعيد والاتصال بالمرضى، وقصور في موارد المختبرات ]المعامل[ وعدم وجود المواد التثقيفية. أما الإجراءات فقد كانت سيئة أيضاً في رأي 6.29% من المرضى، ومن أوجه القصور فيها: غياب المعلومات الأساسية في السجلات، وضياع الفحوصات السريرية الأساسية، كما كانت درجة التحكم في المرض سيئة من وجهة نظر 49.2% من المرضى، ولم ينجح من الإصابة بأية مضاعفات سوى 30.6% من المرضى. وقد كان الامتثال للمواعيد جيداً في رأي 80% من المرضى. أما الحصائل التي هي أفضل (مضاعفات أقل وامتثال أكثر) فقد ترافقت ترافُقاً يُعْتَدُّ به إحصائياً. مع سوء إجراءات الرعاية. ولا يمكن أن نعتبر ذلك من المنبئات ذات المصداقية للحصائل لأن الرعاية الجيدة قد يُشرع بها مع وجود المضاعفات.
ABSTRACT: Selected indicators for structure, process and outcome of care were used to audit diabetes care in 3 centres in Alexandria. Structure was poor: main problems included absence of appointment and recall system, deficiencies in laboratory resources and lack of educational material. Process of care was poor for 69.2% of patients: deficiencies included absence of essential information in records and missing some essential clinical examinations. Degree of control was poor for 49.2% of patients and only 30.6% had no complications. Compliance to appointment was good for about 80% of patients. Better outcome (fewer complications and higher compliance) was significantly associated with poor process of care. This cannot, however, be considered a valid predictor of outcome as good care might be initiated by the presence of complications.
Audit des soins aux diabétiques dans trois centres d’Alexandrie
RÉSUMÉ: Un certain nombre d’indicateurs de structure, de processus et de résultats des soins ont été utilisés pour réaliser un audit des soins aux diabétiques dans trois centres d’Alexandrie. La structure s’est avérée médiocre : les principaux problèmes étaient l’absence de système de rendez-vous et de rappel, des insuffisances en termes de ressources de laboratoire et le manque de matériel pédagogique. Le processus de soins était déficient pour 69,2 % des patients : les points faibles étaient l’absence d’informations essentielles dans les dossiers et l’omission de certains examens cliniques essentiels. Le degré de contrôle était mauvais pour 49,2 % des patients, et seuls 30,6 % n’avaient pas de complications. Le respect des rendez-vous médicaux était bon pour environ 80 % des patients. On a observé une association significative entre de meilleurs résultats (moins de complications et meilleur respect des rendez-vous médicaux) et un mauvais processus de soins. Toutefois, cette association ne peut pas être considérée comme un facteur prédictif de résultats valable, dans la mesure où la mise en place de soins de qualité peut être motivée par la présence de complications.
1Department of Health Administration and Behavioural Sciences; 2Department of Family Health, High Institute of Public Health, University of Alexandria, Alexandria, Egypt ( Correspondence to M.A. Abolfotouh:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
)
Received: 26/12/04; accepted: 15/03/06
EMHJ, 2008, 14(3):636-646
Introduction
Diabetes is one of the major world health problems: prevalence for all age groups worldwide was estimated to be 2.8% in 2000 and projected to be 4.4% in 2030 [1]. The 10 countries estimated to have the highest numbers of people with diabetes in 2000 and 2030 are listed by The International Diabetes Federation Diabetes atlas 2000 [2]. The top 3 countries are the same as those identified for 1995 (China, India and the United States of America) [3]. Bangladesh, Brazil, Indonesia, Japan, and Pakistan also appear in the lists for both 2000 and 2030. Italy and the Russian Federation appear in the list for 2000 but are replaced by Egypt and the Philippines for 2030, reflecting anticipated changes in population and structure in these countries.
The total number of people with diabetes is projected to rise from 171 million in 2000 to 366 million in 2030. The urban population in developing countries is projected to double between 2000 and 2030. For Egypt, the total projected number of people with diabetes is 6.7 million [1].
Treatment and preventive care in persons with diabetes can slow the progression of end-stage complications and reduce the risk of cardiovascular and other diabetes-related disease [4–6]. On the basis of these findings, there has been substantial recent interest in diabetes disease management interventions, guidelines and care practice [7,8]. As the vast majority of diabetes care occurs in primary care settings, to promote proper management, standards for care and clinical practice guidelines targeting primary care providers (among others) have been published by professional organizations such as the Canadian Diabetes Association [9], the American Diabetes Association [10] and the World Health Organization (WHO) [11].
Quality of medical practice and record registration are related. A medical audit is “a detailed review and evaluation of selected clinical records by qualified professional personnel for evaluating quality of medical care” and it is one of the most important functions of the medical staff. The audit committee reviews medical records to determine whether the appropriate action was taken and examine the processes, and to determine whether if the process had been different, i.e. investigation, diagnosis, etc., the outcome would have been different [12]. Audit of diabetes care is now becoming common in general practice [13].
The aim of this study was to assess the care provided at 3 diabetes centres in Alexandria in terms of structure, process and outcome in accordance with documentation and adherence to WHO guidelines [14] for primary diabetes care.
Methods
The study was conducted from March 2003 to end of May 2003. Out of the total of 6 diabetes centres affiliated to Ministry of Health and Population in Alexandria city, 3 centres having higher attendance rate were selected: Abu-Qir Hospital (El Montaza region), Farouk Hospital (middle region) and Ras El-Ten Hospital (El Gomerk region). Returning patients who had been diabetic for ≥ 1 year and who visited the centre during the period of the study (3 months) were the target of the study. During the pilot study, it was noted that the usual number of patients at each centre was 40–50/month. Therefore, using an equal allocation method of sampling, the study included 360 patients registered at and regularly attending the 3 centres. The first 120 consecutive patients attending each centre during the study period were selected. There were no refusals to participate.
All patients were interviewed using structured questionnaires for collection of information about patient characteristics (age, sex, education, employment), disease characteristics (duration of diabetes, presence of complications) and treatment characteristics (type of treatment). Interviews were carried out by the first author in the clinic immediately after clinical examination.
Selected indicators for structure, process and outcome of care were based on the quality assurance protocol and the WHO manual on diabetes mellitus [14,15]
Assessment of structure
Structure of diabetes care was assessed using 2 checklists: one for the essential items of care (13 items) and the second for the less-essential items (10 items). The checklist on essential items was scored on a 3-point scale: item available all the time scored 2; item available sometimes scored 1; item not available scored 0. The checklist of less-essential items of care was scored on a 2-point scale: item available scored 1 and item not available scored 0.
The total score of all items for structure of diabetes care ranged from 0 to 36. If the total score was > 28, i.e. > 80% of the total score, structure of care was considered good; if score was 21–28, i.e. 60%–80%, it was considered fair; if total score was
Assessment of process
Process of care was assessed by a modified scoring system [16]. This depended on the fulfilment of 10 items for good diabetes care by physicians in the previous year by reviewing the medical records. Score ranged from 0 to 10 points. Process was categorized as good (8–10 points), moderate (5–7 points) or poor (
Assessment of outcome
Outcome indicators included degree of diabetes control, degree of compliance with appointment and presence of complications. Control of diabetes was defined as good if the previous 2 readings for fasting blood sugar were 70–120 mg/dL and poor if they were > 120 mg/dL.
Degree of compliance with appointment was based on the number of visits of diabetes patients during a 6-month period. Good compliance (2 points) was recorded for attending the centre on > 2 occasions, fair compliance (1 point) when they attended for 1 occasion and poor compliance (0 points) when they had never attended the centre during the previous 6 months. The total score for outcome of diabetes care ranged from 0 to 6 points, categorized as good (4–6 points), fair (2–3 points) or poor (
Analysis
Data analysis was done using SPSS statistical package, version 10. Statistical significance for difference between rates was tested by chi-squared test and independent sample means by the Student t-test. The F-test was also used to compare between the 3 groups for some variables, e.g. age, duration of illness and compliance. Significance was denoted at the ≤ 0.05 level.
Results
Males constituted 52.2% of the sample and females 41.8%; mean age was 53.36 [standard deviation (SD) 10.83] years. Type I diabetes patients constituted 22.9% and type II diabetes patients 77.1%. Mean duration of diabetes was 1.48 (SD 0.50) years. There was no significant difference between the 3 centres for patient characteristics except for age (F = 10.897; P < 0.01): mean age was highest among Ras El Ten Hospital patients, 55.35 (SD 11.45) years and lowest among those at Abu-Qir Hospital, 49.70 (SD 8.45) years (Table 1).
The average total score for structure of diabetes care in the 3 centres was 15, 16 and 16 points of a total possible 36 points (Table 2), i.e. < 60% of total score, reflecting poor care in all 3 centres. The essential items that were available all the time were: effective referral system, coordination with the district hospital diabetes clinic, direct access to an eye specialist, 1 doctor in the practice who had a special interest in diabetes and a diabetes register. Essential items that were never available included: internal quality assurance system in the practice, appointment system and system for recall of defaulters (Table 2).
Most of the less-essential items were never available apart from direct access to a hospital laboratory, cholesterol measurements, carrying out electrocardiography and funduscopy in the practice and direct access to a dietitian (Table 2).
Audit of process of care recorded in patients’ files for the previous year showed that over 60% of patients had not had their feet examined, nor had they been clinically examined for weight, peripheral sensation and pulse (Table 3). Also, they had not been referred for annual ophthalmic examination, urea and electrolytes. The glycosylated haemoglobin test had not been performed for anyone. This situation was similar in all 3 centres with no statistically significant differences. Regarding overall degree of care, 69.2% of patients received poor care, 26.4% fair care and 4.4% good care. Mean score was lowest at Ras El Ten Hospital and highest at Farouk Hospital (P = 0.004).
Outcome of diabetes care is shown in Table 4. Degree of control was poor for 49.2% of patients; only 30.6% had no complications. Compliance to appointment was good for about 80%. There was no statistically significant difference between the 3 centres as regards outcome items (P > 0.05).
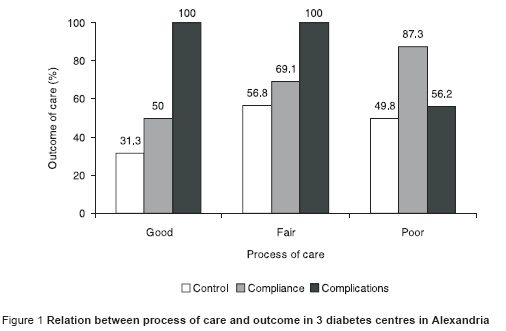
Regarding the relationship between process of care and outcome, with worse degree of care compliance was better than with good care (87.3% vs 50.0%) and there were fewer complications (Figure 1).
Discussion
Diabetes is a chronic illness that requires continuing medical care and patient self-management education to prevent acute complications and to reduce the risk of long-term complications [17,18]. Monitoring and careful recording of important clinical data are considered to be a vital part of diabetes care [19], making it possible to compare past and present status, to review the course of the disease and to justify continuing or changing treatment [20]. However, there is evidence that “usual care” for individuals with diabetes falls short of these ideals [21–24]. Despite the broadly distributed diabetes care guidelines, in the present study, the majority of patients did not have proper documentation of adequate management to optimize control or prevent target organ damage: degree of care was poor for 69.2% of patients. Our findings are comparable with those of other studies in Saudi Arabia [25], Lebanon [26], the United States of America [27,28] and England [29].
The structural criteria are considered antecedents of quality, and outcome criteria are considered consequences of quality [30]. There should be a direct relationship between processes and outcomes of care; less than optimal outcomes have their roots in inappropriate or poorly implemented processes [31]. In the present study, degree of control was poor for more than half the patients. It was interesting, however, to note that better outcome—in terms of fewer complications and higher compliance—was associated with poor process of care, contradictory to what would be expected. This finding could be explained by the fact that many of the elements of process of care were not being carried out except when there were signs of poor outcome in terms of complications, etc. The physician was possibly initiated to provide care only in case of complaint regarding complications, and this may be why there are fewer complications with poor care. Thus poor outcome in terms of more complications and lower rate of compliance acted in the present study as a cause rather than an effect, leading to upgrading the process of care.
Poor outcome in the present study may have been a result of factors such as lack of some essential structural items for care. The shortage of laboratory strips was compensated by cooperation between the clinic and the hospital central laboratory. Actually, the patient is referred for urine analysis for glucose every visit to the clinic (every 10–20 days) and referred for fasting and postprandial blood glucose only every 3rd visit.
Access to a coordinated, interdisciplinary, diabetes care team to offer appropriate care, whether the need is self-management, education, medical advice, or psychosocial support, has been identified as an important factor for improving treatment outcomes in diabetes [31]. The team should include, but not be limited to, physicians, nurses, dietitians and mental health professionals with a special interest in diabetes [32]. In the present study there was lack of some essential items in the structure of care such as a diabetes nurse, and this could influence the process and outcome of care. Nurses can play an important role in patient-oriented interventions, through patient education or facilitating adherence to treatment [33,34]. A dietitian was available in only 2 of the 3 centres in this study, even though it is known that a registered dietitian, knowledgeable and skilled in implementing nutrition therapy into diabetes management and education, is the team member who evaluates the patient’s food intake, metabolic status, lifestyle, readiness to make changes, goal-setting, dietary instruction and evaluation [35].
Compliance to appointment in the present study was rated good for most of the patients. Fair or poor compliance by the others may be a consequence of the absence of an appointment system for diabetes patients or a system for identifying and recalling defaulters. Our results are comparable to those of similar studies in Saudi Arabia [25] and Lebanon [26]. Some studies have shown that organizational interventions that improve regular prompted recall and review of patients (central computerized tracking systems or nurses who regularly contact the patient) can improve diabetes management [33,36].
Glycaemic control is fundamental to the management of diabetes. In some developed countries, at least half of those diagnosed with diabetes do not achieve satisfactory glycaemic control, despite the availability of effective treatments [37]. In the present study the degree of control was poor for about half the patients. Prospective randomized clinical trials have shown that achieving glycaemic control is associated with decreased rates of retinopathy [30,38], nephropathy and neuropathy, and epidemiological studies support the potential of intensive glycaemic control in the reduction of cardiovascular disease [30].
The most important issues in diabetes care, besides good metabolic control, are to reduce the high risk of macrovascular complications by adequate treatment of high blood pressure and to convince diabetes patients to stop smoking [39]. In the present study, 69.4% were suffering from complications. In spite of this, only 35.8% of patients were referred for ophthalmic examination and only 29.4% were referred for protein urea testing, even though direct access to an ophthalmologist and laboratory services were available. Moreover, blood pressure measurements, ECG and lipid profile were only requested in case of complaint. This applied for foot examination also, although all individuals with diabetes should receive an annual foot examination to identify high-risk conditions [32].
Conclusion and recommendations
It is recommended that a special clinic protocol for diabetes care should be developed, based on the standards guidelines and intensive training of physicians. There is a need for the introduction of a diabetes flow-sheet in the patient records to facilitate documentation, there is also a need for a diabetes nurse, educational materials and other essential structure care in each diabetes centre.
The level of process of care cannot be considered a valid predictor of outcome as good care might be initiated by the presence of complications, as seen in the present study. The diabetes care team must be trained not to wait till there is poor outcome to provide quality care.
References
- Wild S et al. Global prevalence of diabetes—estimates for the year 2000 and projections for 2030. Diabetes care, 2004, 27:1047–53.
- Diabetes atlas 2000. Brussels, International Diabetes Federation, 2000.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes care, 1998, 21:1414–31.
- Bertoni AG. Achieving control of diabetic risk factors in primary care settings. American journal of managed care, 2001, 7(4):411–21.
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long term complications of insulin dependent diabetes mellitus. New England journal of medicine, 1993, 329:977–86.
- UK Prospective Diabetes Study Group (UKPDS). Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. British medical journal, 1998, 317(7160):703–13.
- Glasgow RE et al. Diabetes care practices in primary care: results from two samples and three measurement sets. Diabetes educator, 1999, 25(5):755–63.
- American Diabetes Association. Clinical practice recommendations 2000. Diabetes care, 2000, 23 (6):S1–116.
- Canadian Diabetes Association. Clinical practice guidelines for diabetes mellitus in Canada. Canadian diabetes, 1992, 5:1–4.
- American Diabetes Association. Standards of medical care of patients with diabetes mellitus. Diabetes care, 1989, 12(5):365–8.
- Management of diabetes mellitus. Standards of care and clinical guidelines. Geneva, World Health Organization, 1994.
- Shaw CD, Costain DW. Guidelines for medical audit: seven principles. British medical journal, 1989, 299(6697):498–9.
- Dunn N, Pickering R. Does good practice organization improve the outcome of care for diabetic patients? British journal of general practice, 1998, 48(434):1237–40.
- Manual on diabetes mellitus in primary health care. Alexandria, World Health Organization, 1995.
- Quality assurance in primary health care manual. Riyadh, Ministry of Health/World Health Organization Regional Office for the Eastern Mediterranean, 1994 (WHO-EM/PHC/81-A/G/93).
- Chesover D, Tudor-Miles P, Hilton S. Survey and audit of diabetic care in general practice in South London. British journal of general practice, 1991, 41:282–5.
- Ferris FL. How effective are treatments for diabetic retinopathy? Journal of the American Medical Association, 1993, 269:1290–1.
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England journal of medicine, 1993, 329:977–86.
- O’Connor PJ. Organizing diabetes care: identify, monitor, prioritize, intensify. Diabetes care, 2001, 24:1515–6.
- Goudswaard AN et al. Quality of recording of data from patients with type 2 diabetes is not a valid indicator of quality of care. A cross-sectional study. Family practice, 2003, 20:173–7.
- Bell RA et al. Quality of diabetes care among low-income patients in North Carolina. American journal of preventive medicine, 2001, 21:124–31.
- Beckles GL et al. Population-based assessment of the level of care among adults with diabetes in the U.S. Diabetes care, 1998, 21:1432–8.
- Bloom SA et al. Tracking clinical preventive service use: a comparison of the health plan employer data and information set with the behavioral risk factor surveillance system. Medical care, 2000, 38(2):187–94.
- Engelgau MM et al. Use of services by diabetes patients in managed care organizations: development of a diabetes surveillance system: CDC Diabetes in Managed Care Work Group. Diabetes care, 1998, 21:2062–8.
- Khattab M et al. Audit of diabetic care in an academic family practice center in Asir region, Saudi Arabia. Diabetes research, 1996, 31:243–54.
- Akel M, Hamadeh G. Quality of diabetes care in a university health center in Lebanon. International journal for quality in health care, 1999, 11(6):517–21.
- Kell SH et al. Measures of disease control in Medicare beneficiaries with diabetes mellitus. Journal of the American Geriatric Society, 1999, 47(4):417–22.
- Weiner JP et al. Variation in office-based quality: a claims-based profile of care provided to Medicare patients with diabetes. Journal of the American Medical Association, 1995, 273(19):1503–8.
- Dunn NR, Bough P. Standards of care of diabetic patients in a typical English community. British journal of general practice, 1996, 46:401–5.
- Attree M. Towards a conceptual model of quality care. International journal of nursing studies, 1996, 33:13–28.
- Skovlund SE, Peyrot M. The diabetes attitudes, wishes, and needs (DAWN) program: a new approach to improving outcomes of diabetes care. Diabetes spectrum, 2005, 18:136–42,
- American Diabetes Association. Standards of medical care in diabetes. Diabetes care, 2004, 27:S15–35.
- Hansen LJ, Drivsholm TB. Interventioner til forbedring af diabetesbehandlingen i det primaere sundhedsvaesen og pa diabetesambulatorier [Interventions to improve the management of diabetes mellitus in primary health care and outpatient community settings]. Ugeskr laeger, 2002, 164(5):607–9.
- Lim TO. Diabetes care: is it adequate? An audit of diabetes care in a hospital. Medical journal of Malaysia, 1990, 45(1):18–22.
- Purnell B. The role of the dietitian in diabetes care. Diabetes primary care, 1999, 1:84–7.
- Scott RS, Brown LJ, Clifford P. Use of health services by diabetic persons. II. Hospital admissions. Diabetes care, 1985, 8(1):143–7.
- Kristensen JK et al. HbAlc in an unselected population of 4438 people with type 2 diabetes in a Danish county. Scandinavian journal of primary health care, 2001, 19:241–6.
- UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet, 1998, 352:837–53.
- Färnkvist LM, Lundman BM. Outcomes of diabetes care: a population-based study. International journal for quality in health care, 2003, 15:301–7.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)