M. Toumba,1 C. Kanaris,1 K. Simamonian2 and N. Skordis1
حصائل تدبير الحمل لدى المصابات بالثالاسيمية
ميروبي تومبا، كونستانينوس كاناريس، كريكور سيمامونيان، نيكوس سكورديس
الخلاصـة: تقدم هذه الدراسة وصفاً لتدبير الحمل وحصائله السريرية لدى مئة من القبرصيات اليونانيات المصابات بالثالاسيمية؛ منهن 88 مصابة بالثالاسيمية الكبرى و12 مصابة بالثالاسيمية المتوسطة؛ وقد شملت الدراسة 152 حملاً تكلَّل بالنجاح و161 ولادة. وقد أجري لجميع الحالات تقييم للغدد الصماء وقياسات متكررة للفرِّيتين. وضمَّت الحمول المتعددة التي تكللت بالنجاح سبع توائم وحملاً بثلاث أجنة تلو تحريض الإباضة. وقد تطلبت المصابات بالثالاسيمية نقل كمية أكبر من الدم أثناء الحمل، وكان هناك ازدياد يعتد به إحصائياً لمستويات فرِّيتين المصل أثناء الحمل، كما بقيت تلك المستويات مرتفعة ارتفاعاً يعتد به إحصائياً بعد الحمل. وقد انتهت الغالبية العظمى من الأحمال بولادة في تمام الحمل لأطفال أصحاء، وكانت المضاعفات التوليدية نادرة، باستثناء بعض المشكلات القليلة العدد.
ABSTRACT: We describe the management and clinical outcome of pregnancies among 100 Greek Cypriot women with thalassaemia: 88 with thalassaemia major and 12 with thalassaemia intermedia. A total of 152 successful pregnancies and 161 deliveries were included. All patients had endocrine assessment and frequent ferritin measurements. Multiple successful pregnancies included 7 twins and 1 triple pregnancy. Pregnant thalassaemics required significantly larger amount of total blood transfusion during pregnancy. There was a statistically significant increase in the ferritin levels during pregnancy, and levels remained significantly higher after pregnancy. Most pregnancies resulted in delivery of full-term healthy babies, and obstetric complications were rare, although some problems were encountered.
Issue et prise en charge de la grossesse chez les femmes atteintes de thalassémie à Chypre
RÉSUMÉ: Nous décrivons la prise en charge et l’évolution clinique de la grossesse chez 100 Chypriotes grecques atteintes de thalassémie : 88 de thalassémie majeure et 12 de thalassémie intermédiaire. Au total, 152 grossesses menées à terme et 161 accouchements ont été pris en compte. Toutes les patientes étaient surveillées sur le plan endocrinien et faisaient fréquemment l’objet d’un dosage de la ferritine. Parmi les grossesses multiples menées à terme, on a compté 7 grossesses gémellaires et 1 grossesse triple. Pendant la grossesse, les femmes atteintes de thalassémie ont nécessité des quantités de transfusions de sang total significativement plus élevées. On a observé une augmentation statistiquement significative des taux de ferritine pendant la grossesse, et ces taux sont restés significativement plus élevés après la grossesse. La majorité des grossesses se sont achevées par la mise au monde de bébés nés à terme et en bonne santé, et les complications obstétricales ont été rares, en dépit de certains problèmes.
1Paediatric Endocrine Unit, Department of Paediatrics, Makarios Hospital, Nicosia, Cyprus (Correspondence to N. Skordis:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
)
2Thalassaemia Centre, Nicosia, Cyprus.
Received: 04/12/05; accepted: 13/02/06
EMHJ, 2008, 14(3):628-635
Introduction
Normal sexual activity and reproductive capacity has become a demanding task for women suffering from thalassaemia major (TM). Modern advances in medical care have enabled patients with TM to survive successfully into adulthood. The prolonged life expectancy and improvement in quality of life of thalassaemia patients has redefined the challenges that couples face as they now have a realistic chance of creating a family.
Patients with TM are characterized by severe haemolytic anaemia and are dependent on multiple blood transfusions, which consequently result in tissue haemosiderosis. Patients with thalassaemia intermedia (TI), a clinically milder disorder, present with variable clinical features, from absence of symptoms to moderate and severe anaemia. TI patients can also have splenomegaly, skeletal deformities due to bone marrow expansion and haemosiderosis due to increased iron absorption from the gastrointestinal tract. In both cases iron deposition affects the cardiac, hepatic and endocrine systems [1].
Endocrine complications have been shown to be the result of iron deposition on the endocrine glands. Hypogonadotrophic hypogonadism, which is the commonest endocrinopathy, is the result of iron deposition on the pituitary gonadotroph cells and the hypothalamus, which both seem to be extremely sensitive to haemosiderosis [2–4]. TM patients often suffer from complete failure of pubertal development or develop hypogonadism later in their life. Female thalassaemia patients may have primary or secondary amenorrhoea, which leads to failure of the reproductive axis with chronic anovulation. Despite severe haemosiderosis, ovarian function is preserved in most of the patients, as they are still able to increase the oestradiol level following gonadotrophin stimulation resulting in ova production [5,6].
Early recognition and treatment of hypogonadotrophic hypogonadism is mandatory in order to preserve fertility and to increase the chances of parenthood in thalassaemic patients. Spontaneous pregnancies in women with preserved hypothalamic–pituitary–gonadal axis, who have normal menstrual cycles is a reality. Furthermore, women with primary or secondary amenorrhoea are able to conceive after proper treatment [7].
The purpose of this study was to describe the management and clinical outcomes of 100 pregnant women with thalassaemia attending thalassaemia centres in Cyprus in order to document the effectiveness of modern therapeutic advances.
Methods
This retrospective study over the period 1990–2004 included 100 pregnant women who were attending the 4 thalassaemia centres (Nicosia, Limassol, Larnaca and Paphos) in Cyprus. All thalassaemic women who were followed up in our clinics since their birth and who conceived, with treatment or spontaneously, and had successful deliveries were included in the study. At the time of pregnancy all were between ages 20 and 35 years. Of the 100 women, 88 suffered from TM and had been regularly transfused since infancy to maintain haemo-globin at the level of 10 g/dL. Treatment with chelating agents was initiated around the age of 2 years in the majority of these patients. Another 12 women had TI and required no transfusions.
For the purpose of the study the patients were divided into 4 groups.
Group 1 (n = 60): TM and normal sexual development, attained menarche and normal menstrual function.
Group 2 (n = 12): TI and normal menstrual cycles.
Group 3 (n = 11): TM and primary amenorrhoea.
Group 4 (n = 17): TM and secondary amenorrhoea before pregnancy.
All patients had endocrine assessment, which included measurement of free thyroxine (T4), thyroid stimulating hormone (TSH), prolactin, follicle stimulating hormone (FSH), luteinizing hormone (LH), oestradiol and a.m. cortisol. They also underwent gonadotropin-releasing hormone (GnRH) test by using the standard method before pregnancy and an oral glucose tolerance test was performed annually. Information about the method of conception, the mode of delivery and the outcome of pregnancy was collected from the patients’ medical records and from personal interviews.
Nine (9) of the patients had their cardiac function evaluated by serial echocardio-graphy (M-mode, 2-dimensional, Doppler) during pregnancy and after delivery. The following indices were measured: end systolic dimension, end diastolic dimension and ejection fraction.
Statistical analysis
To evaluate transfusion requirements and ferritin levels before, during and after pregnancy the Student t-test for paired data was used for group 1 and the Wilcoxon signed rank test for paired data was used for groups 3 and 4.
Results
Conception
The majority of our patients who had normal menstrual cycles conceived spontaneously. Induction of ovulation was performed in those who failed to conceive after 1 year of sexual intercourse with their partner and in those who wished a planned pregnancy. Women with amenorrhoea achieved conception after ovulation was induced. Surprisingly 1 patient with primary amenorrhoea conceived spontaneously, while she was on replacement combined treatment with oestrogen and progesterone.
In 8 of the couples included in the study, both members were thalassaemia patients. Following genetic counselling, 6 couples decided to proceed to sperm donation. One couple where the female partner suffered primary amenorrhoea and type 1 diabetes mellitus proceeded to ovum donation after failure of conception with sperm donation. In the remaining couple where the female had intact gonadal function, pregnancy was spontaneously achieved.
Number of successful pregnancies
A total of 100 Greek Cypriot women with TM and TI were able to achieve pregnancy and successfully deliver babies. These 100 women had 152 successful pregnancies between them, which resulted in the delivery of 161 babies. The mean birth weight of the full-term babies was 2700 g, which is considered appropriate for gestational age. Overall, there were only 4 babies who were classified as small-for-gestational-age and in these cases there was a correlation between the level of maternal haemoglobin during pregnancy and the birth weight of the baby. There were 5 twin pregnancies in women with primary amenorrhoea and secondary amenorrhoea (induced) and 2 twin pregnancies in patients with normal menstrual cycles (1 induced and 1 spontaneous) and also 1 triple pregnancy in a patient with primary amenorrhoea (induced).
The majority of pregnancies (79.9%) resulted in successful deliveries of full-term babies, whereas 13.3% resulted in premature deliveries, half of which were not singleton births. From all the pregnancies, 7 (4.7%) resulted in spontaneous abortions and 3 (2.1%) in very premature delivery of stillborn babies.
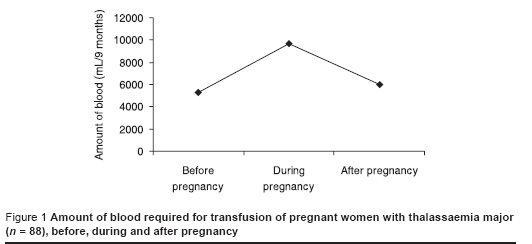
Transfusion requirements
As expected, pregnant TM patients required significantly larger amounts of total blood transfusion during pregnancy (P < 0.005 for group 1 and P < 0.05 for groups 3 and 4) as shown on Figure 1. In all 3 groups there was no difference between the amounts of blood required before pregnancy compared with that required after delivery. There was also no difference between the haemoglobin level before, during and after pregnancy in all 3 groups.
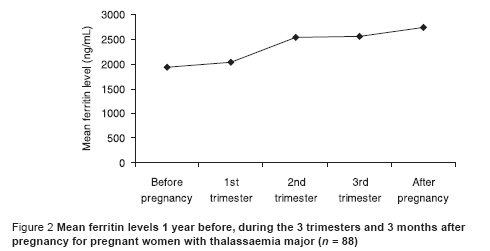
Ferritin levels
The mean ferritin levels 1 year before, during each of 3 trimesters and 1 year after pregnancy are shown on Figure 2. There was a statistically significant increase of the ferritin levels during pregnancy when they were compared to those before pregnancy for group 1 (P < 0.01) and for groups 3 and 4 taken together (P < 0.01). The ferritin levels remained significantly increased after pregnancy in all 3 groups (P < 0.01).
Complications
Two of our patients developed ovarian hyperstimulation syndrome, and were successfully recovered. The 28-year-old patient who carried a triple pregnancy developed congestive cardiac failure, as the consequence of cardiac tamponade following pericarditis. She was successfully treated and an elective premature caesarean section was performed. One patient who developed an uneventful episode of pericarditis also recovered. There were no other endocrine complications noted, nor any case of gestational diabetes. None of the patients showed impairment of renal function. Two of the patients with primary amenorrhoea, including the one with the triple pregnancy, developed pre-eclampsia, for which they had a premature caesarean delivery.
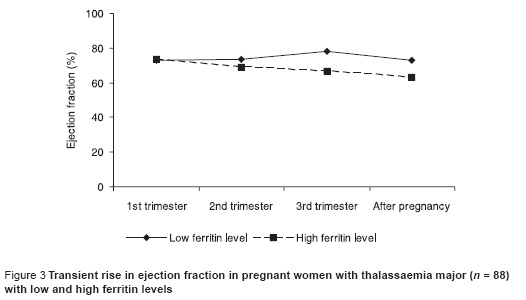
Cardiological evaluation
A transient increase in left ventricular (LV) end diastolic dimension, minimal change in LV end systolic dimension, and increase in systolic function, as measured with ejection fraction was observed in all the patients. All cardiac indices returned to the pre-pregnancy values following delivery (Figure 3). Interestingly, women who started pregnancy with a higher ferritin level had a more attenuated increase in LV end systolic dimension, accompanied by a decrease instead of an increase in systolic function. An expected elevation of their cardiac output was documented but no other significant changes in end systolic dimension and deviation in the indices for LV diastolic function were identified.
Discussion
Women with thalassaemia who are regularly transfused and are well chelated can now become pregnant either spontaneously or by inducing ovulation. The presence of gonadal dysfunction can be overcome with proper combination treatment. It is necessary that all pregnant thalassaemia patients be followed up very closely. Apart from the routine pregnancy follow-up, the thalassaemic pregnant woman needs additional medical care. Haemoglobin levels should be maintained at 10 g/dL and careful monitoring of vital signs during transfusion is required. Ferritin levels should also be measured and observed to avoid iron overload. Careful monitoring of the transfusion regime and regular evaluation of cardiac function should be done in all pregnant thalassaemic women to prevent fluid overload. Cardiac function should be evaluated periodically by a cardiologist.
The increase in ferritin levels during pregnancy is attributed to the discontinuation of iron chelation therapy and the increased amount of blood required for their transfusions. Increased ferritin levels during the last trimester of pregnancy and after delivery have not been reported before. Previous studies show that serum ferritin levels rise by 10% or less after delivery when compared to the prepregnancy level [6].
Iron chelation therapy, due to its possible teratogenic effects, is withheld as soon as the pregnancy is planned or identified. It has been assumed that pregnancy is an efficient chelator of iron due to its haemodilution effect and the fetal consumption of free iron. Although desferrioxamine therapy has not been implicated for any deleterious effect on the fetus, the current recommendation is its discontinuation, both once pregnancy is identified and during the induction period [8–10].
Chronic maternal anaemia in the thalassaemic pregnant woman may result in fetal hypoxia, which predisposes to premature labour, intrauterine growth retardation (IUGR) and death. In our study the incidence of such complications was smaller compared to a similar study which reported 2 abortions, 2 stillbirths and 3 pre-term deliveries (1 of which was in a twin pregnancy) in 17 pregnancies [11]. The percentage of IUGR babies in our series (4.5%) is also smaller compared to other reports [11,12].
During the induction of ovulation there is always the risk of ovarian hyperstimulation syndrome, a rare but life-threatening complication. It presents with ascites, hydrothorax, embolism and coagulation disturbances. Furthermore, both the renal and liver functions are affected due to increased vascular permeability; this results in fluid shifting from the intravascular to the extravascular compartment. Since this is a potentially life-threatening condition, all pro-ovulatory medication should be discontinued, and the patient must be carefully monitored and treated in the intensive care unit [13].
The pregnant woman with thalassaemia faces possible deleterious consequences in cardiac function as a result of myocardial haemosiderosis and changes in the haemodynamic state. Accelerated erythropoiesis and expansion of the total red cell volume occur, which consequently increase the cardiac output. This may well lead to cardiac failure. There were no severe cardiac complications reported previously, except for 1 case with early infiltrative cardiomyopathy [5]. In a previous report, with a larger number of pregnant women, there were no clinical or electrocardiographic changes during cardiac examination [14]. It is important for women to start pregnancy with low ferritin levels in order not to have a decrease in their systolic function indices.
A small number of women (8.8%) developed secondary amenorrhoea after delivery, although they attained menarche, had had normal menstrual cycles and became pregnant spontaneously. Pregnancy cannot be implicated as the causative factor as most women with TM develop secondary amenorrhoea at some stage in their life [15].
The desire of the thalassaemia woman to procreate should to be viewed with special caution and sensitivity by all physicians who are involved in her medical care. Medical reasons often impose a barrier to this wish. Based on experience in our clinic we have devised a protocol for follow-up of pregnant thalassaemic women:
Eligibility
Cardiac function: electrocardiogram, echocardiogram
Liver function: liver function test, ultrasound
Vessels: clotting factors, Doppler
Pancreas: oral glucose tolerance test
Viral infections: hepatitis B and C virus, HIV
Iron status
Feasibility
Hypothalamic–pituitary–gonadal axis
Ultrasound of uterus and ovaries
Postcoital test
Hysterosalpingography
Complete endocrine assessment
Genetic counselling: partner’s carrier status and fertility
During pregnancy there are a number of issues that need to be taken into consideration. Accumulated knowledge over the years from our clinic has helped us to formulate guidelines regarding the management of the pregnant thalassaemia patient, as follows:
Maintenance of haemoglobin level at 10 g/dL
Frequent low volume blood transfusions
Discontinue iron chelation therapy
Regular cardiac monitoring every 3 months
Assessment of endocrine function, including oral glucose tolerance test
Multidisciplinary approach by all specialists involved in the medical care of thalassaemia.
The strong desire of the thalassaemic woman to become pregnant must not be viewed as an emotional defiance of the stigma of her chronic disease, but recognized, respected and approached with sensitivity by all specialties involved in her medical care.
Acknowledgements
The authors wish to thanks Drs Soteroulla Christou, George Skordos, Evi Pangalou, Michael Hadjigavriel, Maria Sitarou and Annita Kolnakou for their contribution to this paper.
References
- Olivieri NF. Medical progress: the (beta)-thalassaemias. New England journal of medicine, 1999, 341:99–109.
- Berkovitch M et al. Iron deposition in the anterior pituitary in homozygous beta-thalassaemia: MRI evaluation and correlation with gonadal function. Journal of pediatric endocrinology and metabolism, 2000, 13:179–84.
- Charttejee R, Katz M, Cox TF. Prospective study of the hypothalamic–pituitary axis in thalassaemic patients who developed secondary amenorrhea. Clinical endocrinology, 1993, 39:278–96.
- De Sanctis V et al. Gonadal function in patients with β thalassemia major. Journal of clinical pathology, 1988, 41:113–37.
- Skordis N et al. Fertility in female thalassaemics. Journal of pediatric endocrinology and metabolism, 1998, 11(Suppl. 3):935–43.
- Jensen CE, Tuck SM, Wonke B. Fertility in β thalassemia major: a report of 16 pregnancies, pre-conceptual evaluation and review of the literature. British journal of obstetrics and gynaecology, 1995, 102:625–9.
- Skordis N et al. Update on fertility in thalassaemia major Pediatric endocrinology reviews, 2004, 2(Suppl. 2):296–302.
- Meadows K. A successful pregnancy outcome in transfusion dependent Thalassaemia major. Australian New Zealand journal of obstetrics and gynecology, 1984, 24:43–4.
- Martin K. Successful pregnancy in beta-thalassaemia major. Australian paediatric journal, 1983, 19(3):182–3.
- Voskaridou E et al. Desferrioxamine treatment during early pregnancy: absence of teratogenicity in two cases. Haematologica, 1993, 78:183–4.
- Savona-Ventura C, Grech ES. Pregnancy complications in homozygous thalassaemia patients. Journal of obstetrics and gynecology, 1991, 11:175–6.
- Tampakoudis P et al. Transfusion-dependent homozygous beta-thalassaemia major: successful pregnancy in five cases. European journal of obstetrics, gynecology and reproductive biology, 1997, 74:127–31.
- Negri P et al. Preliminary observations about assisted reproduction in thalassaemia. Journal of pediatric endocrinology and metabolism, 1998, 11(Suppl. 3): 929–33.
- Aesopos A et al. Pregnancy in patients with well-treated beta-thalassaemia: outcome for mothers and newborn infants. American journal of obstetrics and gynecology, 1999, 180:360–5.
- Skordis N et al. The impact of iron overload and genotype on gonadal function in women with thalassaemia major. Pediatric endocrinology reviews, 2004, 2(Suppl. 2):292–5.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)