P.K. Patel,1 S.T. Al-Awaidy,2 S. Bawikar, 2 S. Al-Busaidy3 and S. Al-Mahrooqi2
وبائيات الحصبة وتأثيراتها على برنامج التمنيع في سلطنة عُمان
براكاش ك. باتل، صلاح بن ثابت العويدي، شيام باوكر، سليمان البوسعيدي، سالم المحروقي
الخلاصـة: أجرى الباحثون دراسة استعادية مستندة على السجلات من الأول من كانون الثاني/يناير 2003 وحتى 31 كانون الأول/ديسمبر 2003 لوصف وبائيات الحصبة في عُمان وتأثيراتها على برنامج التمنيع، مستمدين المعطيات من نظام التـرصُّد الوبائي، فأدرجوا في الدراسة جميع الحالات التي أبلغ عن الاشتباه بإصابتها بالحصبة خلال فتـرة الدراسة؛ وقد بلغ عدد هذه الحالات 185 حالة، تم التثبُّت من 19.4% منها على أنها حصبة فعلاً. وقد جمع الباحثون عينات دم لتحري الغلوبولين المناعي M من 97.3% من الحالات. وكان العمر الوسطي لحالات الحصبة 8 سنوات (بانحراف معياري قدره 10.7 سنوات). وكان المعدل التقديري الإجمالي لوقوع الحصبة في فتـرة الدراسة 0.53 لكل مئة ألف شخص – سنة. ودلَّ التحليل التحوّفي على أن الحصبة أكثر شيوعاً لدرجة يُعْتَدُّ بها إحصائياً بين غير العُمانيين وبين الأطفال الذين لم يتلقوا التلقيح ضدها.
ABSTRACT: To describe the epidemiology of measles in Oman and the implications for a vaccination programme, we conducted a retrospective record-based study from 1 January 2000 to 31 December 2003 using data from the national epidemiological surveillance system. All cases notified as suspected measles during the study period were included. Of the 185 notified cases, 19.4% were confirmed measles positive. Blood samples for measles IgM were collected in 97.3% of cases. The mean age of measles cases was 8.0 (SD 10.7) years. The estimated overall incidence rate of measles for the study period was 0.53 per 100 000 person-years. Regression analysis indicated measles was significantly commoner among non-Omanis and children who had not been vaccinated.
Épidémiologie de la rougeole et ses implications pour un programme de vaccination à Oman
RÉSUMÉ: Afin de décrire l’épidémiologie de la rougeole à Oman et ses implications pour un programme de vaccination, nous avons mené une étude rétrospective à partir des registres, du 1er janvier 2000 au 31 décembre 2003, en utilisant les données du système national de surveillance épidémiologique. Tous les cas suspects de rougeole notifiés pendant la durée de l’étude ont été pris en compte. Sur les 185 cas notifiés, 19,4 % ont été confirmés positifs. Des échantillons de sang destinés à la détection d’IgM spécifiques de la rougeole ont été prélevés dans 97,3 % des cas. L’âge moyen des cas de rougeole était de 8,0 ans (écart type 10,7) . Le taux global d’incidence de la rougeole estimé pour la période sur laquelle portait l’étude était de 0,53 pour 100 000 personnes-années. L’analyse de régression a permis d’établir que la rougeole était significativement plus courante parmi les non-Omanais et les enfants qui n’avaient pas été vaccinés.
1Department of Health Affairs, Directorate-General of Health Services, Dhahira, Ministry of Health, Oman (Correspondence to P. K. Patel:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
)
2Department of Communicable Disease Surveillance and Control;
3Central Public Laboratory (CPHL), Ministry of Health, Muscat, Oman.
Received: 04/02/06; accepted: 27/03/06
EMHJ, 2008, 14(3):579-589
Introduction
Measles is an acute highly infectious disease of childhood. It has been assumed the disease may be eliminated because of the following reasons: humans are the sole reservoir of the virus; transmission can only be between humans; the virus is very stable; a human carrier state does not exist; and there is a vaccine of proven high efficacy [1]. Initially it was thought that measles elimination could be achieved quickly with a routine one-dose programme but experience has shown that at the very least high coverage of 2 doses is required to achieve elimination [2].
In spite of the availability of and effective vaccine, measles remains a public health problem worldwide especially in developing countries with 30–40 million cases occurring annually. In 2002, there were an estimated 610 000 deaths due to measles worldwide, 540 000 of them in children under the age of 5 years, representing 30%–40% of the burden of vaccine-preventable diseases in childhood. Target dates of 2000, 2007 and 2010 for the elimination of measles were established for the region of the Americas, the European Region and the Eastern Mediterranean Region (EMR) respectively [3]. Several strategies are now being adopted to increase coverage of immunization including a 2-dose schedule, mopping up, supplementary immunization with vitamin A, national and regional mass immunizations, and development of high-quality case-based measles surveillance supported by regional measles laboratory [4]. Oman is one of the EMR countries to adopt these elimination strategies.
Elimination does not equate to zero cases because when elimination has been achieved, imported cases may still occur, with limited spread to susceptible persons. Eventually there will be enough susceptibles from the small proportion of vaccine failures to allow an epidemic [5]. Thus there is a continued need for surveillance even when no cases are reported.
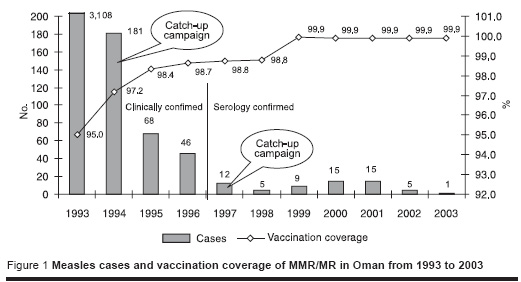
Occurrence of measles cases has decreased drastically in Oman from 40 679 cases in 1981 to a mere 15 cases in 2001, which is largely due to sustained high coverage of routine immunization, catch-up campaigns and intense case-based surveillance. Measles vaccination was formally launched in Oman in 1981 under the Expanded Programme on Immunization (EPI) programme with a single dose of the measles vaccine given at 9 months. In March 1994, a second dose of measles was introduced at 15 months as measles/rubella (MR) vaccine, and a catch-up campaign with this vaccine was done in March 1994 for all individuals aged 15 months to 18 years. The MR vaccination was replaced by measles/mumps/rubella (MMR) vaccine during 1997 and in October 2001 measles vaccination and MMR vaccination were rescheduled at 12 and 18 months respectively [6]. Figure 1 shows the number of measles cases reported between 1993 and 2003 with the 2-dose vaccination coverage and catch-up campaigns in Oman [7].
Oman has 2 340 815 inhabitants with a 23.9% expatriate population. Approximately 10.3% of the total population is below 5 years of age (2003 census) [8]. In Oman, measles has been a notifiable disease (individual case-based notification) since March 1991, when communicable disease surveillance was established. All the cases that satisfy the case definition of measles are recorded in a disease notification form along with the mandatory information form. Blood samples are also collected and sent for measles IgM testing routinely.
To assess progress in measles control, it is recommended that immunization programmes be evaluated by means of specific epidemiological surveillance involving investigation of all reported cases. Furthermore, the epidemiological characteristics of a disease may vary according to geographical area, age group and transmission setting, thereby calling for the implementation of different purpose-designed preventive strategies [2]. Hence, this study aimed to describe the series of measles cases notified in Oman over a 4-year period through the epidemiological surveillance system.
Methods
For the purpose of this study, the database of case-based notification and mandatory information forms for measles was used; this is available within the national epidemiological surveillance system. This retrospective review of records was carried out from 1 January 2000 to 31 December 2003 (4 years); data became available in electronic format in 2000. All the cases notified by the attending physicians during this period were included in the study. Information was collected on: patient’s identification data (name, sex, age, address, region and nationality), presenting symptoms, laboratory data, record of vaccination, source of infection and link with any outbreak. Physicians (paediatricians, general practitioners and general medicine doctors) had been trained in collecting this information during regional seminars conducted periodically.
The Ministry of Health (MOH) in Oman has written guidelines (communicable disease surveillance and control manual) for the surveillance of communicable diseases including measles and there is mandatory case notification from all health institutions, including primary care, and wide health care access and utilization (97%) [9]. It is unlikely therefore that measles cases remain undetected by the surveillance system for an extended period. In addition, measles surveillance in Oman is sensitive enough to consistently detect imported cases, isolated cases, and small outbreaks. However, cases that are mild and do not approach a health facility may go unnoticed.
The regional epidemiologist/communicable disease focal point in the regional headquarters oversees the activities of the surveillance and validates the data. A formal epidemiological investigation is carried out by the focal point upon receipt of notification and all the positive cases are actively followed up to search for the source of infection and other measles cases among the contacts and the community. Epidemiological links to any case and to an imported case are also evaluated. A weekly negative report of measles is also made in sentinel sites, including the private clinics, as a part of the elimination strategy.
The clinical case definition used was: disease displaying the following characteristics: (a) maculo-papular rash, (b) fever ≥ 38.3 °C, and (c) cough, coryza or conjunctivitis. Cases are classified: as “probable” if they fulfil the clinical definition, or as “confirmed”, if, in addition, there is an epidemiological link to another case of measles or laboratory evidence (demonstration of specific serum IgM antibodies). A measles outbreak is defined as presentation of 2 or more epidemiologically linked cases within a maximum period of 14 days (incubation period). Imported cases are those in persons infected outside Oman and the illness cannot be linked to local transmission.
The 0.5–1 mL serum samples collected for each suspected case all over Oman are transported to Central Public Health Laboratory (CPHL), Darsiet, Muscat at 4–8 °C within 24–48 hours. The CPHL is also a reference laboratory for measles surveillance in the Eastern Mediterranean Region of the World Health Organization (WHO) Demonstration of specific IgM antibodies is done using the Behring Enzygnost enzyme-linked immunosorbent assay (ELISA) kit (Marburg, Germany). Laboratory validation is routinely done by sending samples to the WHO reference laboratory in Cairo, Egypt.
The data extracted in our study were analysed using SPSS, version 9. Univariate analysis was done to calculate frequencies and proportions. Age-specific incidence rates were calculated per 100 000 population, using the 2003 population-census as denominator. Association between the different age groups and risk of measles among cases was studied with reference to the relative risk (RR) (incidence rate ratio) and 95% confidence interval (CI). To determine the independent contribution of each variable among the notified cases, adjusted odds ratios (OR) and 95% CI were calculated by means of a logistic regression model.
Results
Over the 4-year study period, 190 cases of measles were notified from all the regions in Oman. Of these, 185 cases met the clinical case definition (97.4%). Of these 185 cases, 19.5% were found to be positive for measles, 11.9% (22/185) were laboratory confirmed by testing IgM positive and 7.6% (14/185) were epidemiologically confirmed on being associated with another case of measles that was later laboratory confirmed. There were 145 (78.4%) laboratory-confirmed negative cases. Although the remaining 4 cases fulfilled the clinical definition, no additional laboratory evidence was forthcoming, and they were duly classified as “probable” cases (Table 1).
Overall, blood samples for measles IgM were collected in 97.3% (180/185) of cases. All the 185 cases had presented with fever and rash as a symptom. Cough, coryza and conjunctivitis were associated with 65%, 68% and 32% of notified cases respectively. The positive predictive value for measles of cough, coryza and conjunctivitis was 25.9%, 28.3% and 40.0% respectively. Information on the gender of the cases was obtained for 60 notified cases. Of these 60, 35.8% were male and 49.2% female. There was no significant difference in the measles cases between males (6 positive) and females (5 positive) (χ2 = 0.64, P = 0.7).
For the purpose of analysis, confirmed and probable positive cases were considered as measles cases (40 cases, 21.6%). The mean age and standard deviation (SD) was 8.0 (SD 10.7) years as shown in Figure 2. The largest proportion (37.5%) of the measles cases was in the < 1 year age group followed by 1–4 years age group (20.0%); altogether the under 5 years age group represented 57.5% of the cases. The estimated overall incidence rate of measles for the study period was 0.53 per 100 000 person years. The incidence was higher in those aged < 1 year (RR = 14.8; 95% CI: 9.7–24.4); 1–5 years (RR = 2.0; 95% CI: 1.0–3.7); and 5–9 years (RR = 1.3; 95% CI: 0.6–2.6) as shown in Table 2.
![Figure 2 Age distribution of the 40 measles cases, 2000–2003 [Mean 8 (SD 10.7) years] Figure 2 Age distribution of the 40 measles cases, 2000–2003 [Mean 8 (SD 10.7) years]](/images/stories/emhj/vol14/03/14-3-08-f2.jpg)
The probable source of infection was established in 35.0% (14/40) of cases. Eleven of the 14 cases were linked to an epidemiological outbreak and later laboratory-confirmed and the other 3 cases were classified as imported. During the outbreak the place of transmission was the school and the secondary transmission occurred at home. Of the remaining cases where the source of infection was not established, 4 were probably vaccine-related and 22 were sporadic cases. There were 2 outbreaks during the study period, one each in North Sharqiya and Dhahira regions of Oman. In North Sharqiya, 10 cases were reported from 8 April 2000 to 23 June 2000. Epidemiological investigation suggested that the reason for the outbreak was inconclusive with no established chains of transmission. In Dhahira there were 12 cases reported from 10 September 2001 to 9 January 2002. The outbreak was linked to an imported case and the source was evident in 11 cases, with 3 chains of transmission, mostly involving expatriate children.
Table 3 illustrates the measles cases with respect to vaccination status. Half of the cases had either not received the measles vaccine or did not know their vaccination status. The majority (75%) of these cases were expatriates and vaccination records were not available for them. The remaining 25% had received some vaccine (7 cases, a single dose; 3 cases, 2 doses). It is noteworthy that 25% (10 cases) of the measles cases were younger than the eligible age for vaccination under the current EPI schedule for measles vaccination; 70% of these 10 were Omani and 30% were expatriate children.
The measles risk among the notified cases was compared with various factors such as age, nationality and vaccination status at the time of notification as shown in Table 4. Among the notified cases from all the regions in Oman, measles cases were higher among children < 5 years and non-Omanis. Similarly, cases who were not due for measles vaccines and who were not vaccinated also had a higher risk of measles. However, regression analysis indicted that measles was significantly commoner only among notified individuals who were non-Omani (OR = 2.8; 95% CI: 1.0–8.0), who had not received measles vaccination (OR = 23.6; 95% CI: 4.4–125.0) and who had received 1 dose of the measles vaccine (OR = 7.3; 95% CI: 1.5–34.6).
North Sharqiya and Dhahira regions had a higher risk of measles compared to other regions possibly because of the outbreaks that occurred during the study period in these 2 regions. However, there was no statistically significant difference in the occurrence of measles cases between the various regions in Oman (P > 0.05).
Discussion
The routine epidemiological measles surveillance system implemented in Oman provides the major characteristics of measles cases registered in all the regions. The proportion of measles IgM-positive cases among the blood samples collected was 20.0% (36/180), which is low compared to a study conducted in Catalonia, Spain (70.1%) [2]. This is possibly due to a decline in incidence of measles over the years in Oman which tends to produce a reciprocal effect of an increase in the number of false notifications (over-diagnosis) [10]. Also in the Catalonia study, cases were confirmed using blood and nasopharyngeal secretions which could account for the higher positivity. The proportion of confirmed (IgM-positive and linked to an outbreak) cases in the present study was 19.4% (36/185), which again is low compared to the study conducted in Catalonia, Spain (30%) [2], but higher compared to southern African countries [11].
In situations marked by low number of cases, such as in our study, serum-based diagnostic confirmation is the choice, as was the case in Oman [12]. On the other hand, if large numbers of cases are reported, rapid, non-aggressive salivary determination of type-specific IgM antibody can enhance the reporting reliability and accelerate control measures [13]. The proportion of associated symptoms like cough, coryza and conjunctivitis was low in our study compared to the Spanish study [2]. The positive predictive value for conjunctivitis was 40%, suggesting conjunctivitis is an important clinical feature in measles diagnosis in Oman.
The proportion of cases under the age of 5 years was higher (57.5%) in our study compared to the 24% and 38% in other studies [2,14]. The greatest proportion of the cases (37.5%) was in the age group < 1 year. The age-specific incidence rates indicted that the age groups <1 year and 1–4 years were at the highest risk of presenting with measles; among 87% (20/23) of these cases no transmission pathway could be established. Correspondingly, outbreak-related cases did not exceed 50% and in the majority of cases there was insufficient evidence for reconstruction of the transmission pathway. This might be due to the existence of measles virus circulation via mild cases among vaccinated individuals [15,16]. However, estimation of susceptibles according to the mathematical model of WHO in Oman gives a figure below the critical < 5% for the birth cohort since 1994 [17]. Hence, the reason for outbreaks due to unlinked imported cases and sporadic cases was not apparent.
The majority (71.4%) of the measles cases with a chain of transmission were in the > 4 years age group (10/14) and 90% of them were unvaccinated expatriate children. Three cases were imported cases. Likewise, a significant number of measles cases occurred among unvaccinated non-Omanis compared to Omanis who had received some vaccination. Hence, vaccination requirement at school entry [2,15] and mass campaigns, especially among expatriate children, may help to prevent measles outbreaks in Oman due to imported cases. Mandatory measles vaccination requirements for expatriate children entering the country could also be considered.
With respect to place of infection, an appreciable proportion of cases, 47.5% (19/40), were associated with school and the home. Similarly, as described in other studies, home and schools must be viewed as settings that pose a risk of transmission [18,19]. The mingling of cohorts of infants and young children with a high proportion of susceptibles (due for vaccination and unvaccinated) constitutes an ideal situation for the occurrence of outbreaks in such places [20,21]. Despite control measures, secondary cases occurred during the outbreak thus signifying continued transmission [22].
In our study, 25% of the cases were yet to be vaccinated. However, a change in the current routine immunization (2 doses of MMR at 12 and 18 months) is not indicated in Oman during its elimination phase, because it is suggested that if MMR coverage at 12 months of age can reach > 90%, it would be worth changing the policy to 2 doses at 12 months and 6 years of age to induce higher antibody titres and prevent primary vaccine failure [23–25].
During the elimination phase, multiple imported sources of measles virus will result in an increase in susceptibility to measles among those 6 months during outbreaks and who are travelling to endemic countries could be considered [26,27]. Further genotypic studies of the measles virus in Oman could provide clues as to whether measles is endemic in Oman or not; if a diversity of measles virus genotypes is observed this will reflect multiple imported sources of the virus and indicate that no genotype of measles is endemic. However, lack of endemic transmission is evident by the limited secondary transmission from imported cases [28].
The 3 measles cases in our study who had received 2 doses of vaccine represent the small proportion of primary vaccine failures that fail to seroconvert despite revaccination with a second dose [29,30]. Similarly, in Britain, over a tenth of cases occurred in children who had been vaccinated [31] because vaccine failure is known to sustain transmission in populations with high vaccine coverage [29].
Complementary measures, such as administration of a further dose of vaccine over a short period of time to the whole population of a given age group, regardless of prior vaccination status, by catch-up campaigns can also be considered [32]. However, it is a costly strategy and one that is difficult to sustain over an extended period of time. All such measures will have to be assessed within a regional context of measles eradication in the short term [33]. In the Americas, sustained interruption of indigenous measles virus transmission has been achieved through a 3-tiered vaccination strategy that includes a) “catch-up” vaccination of all persons aged 1–14 years, regardless of disease history or vaccination status; b) “keep-up” vaccination of greater than or equal to 90% of children in each successive birth cohort at age 12 months; and c) “follow-up” campaigns designed to vaccinate all persons within a specific age range whenever the number of susceptible persons in the preschool-aged population approximates the size of a typical birth cohort (every 3–5 years) [34].
Conclusion
The incidence of measles is low in Oman. Children under 5 years, especially unvaccinated expatriate children, could present as imported cases of measles leading to limited spread to the susceptible population in Oman. Continued effort to bring down the susceptibles by high vaccination coverage, sensitive investigation of all reported positive cases, identification of clusters linking them geographically or by time, and supplementary vaccination measures will assist in the further reduction of measles incidence in Oman.
Acknowledgements
We would like to thank Dr Ali Jaffer Mohammed, DGHA, for his valuable guidance and support. We also thank all the disease surveillance staff and study subjects involved in the study.
References
- Duclos P et al. Measles in adults in Canada and the United States: implications for measles elimination and eradication. International journal of epidemiology, 1999, 28:141–6.
- Godoy P et al. Measles epidemiology in Catalonia (Spain): implications for a regional vaccination programme. International journal of epidemiology, 1999, 28:558–62.
- Progress toward global measles control and regional elimination, 1990–1997. Morbidity and mortality weekly report, 1998, 47(48):1049–54.
- World Health Organization. Initiative for vaccine research (IVR) website. Acute respiratory infections. Measles. ( http://www.who.int/vaccine_research/diseases/ari/en/index1.html, accessed 4 October 2007).
- World Health Organization, Department of Vaccines and Biologicals. Measles technical working group: strategies for measles control and elimination. Report of a meeting, Geneva, 11–12 May 2000. ( www.who.int/vaccine_research/diseases/measles/en/Measles_TechWorkGroup_110502.pdf, accessed 4 October 2007).
- The milestones of EPI in Oman. Manual on Expanded Programme on Immunization, 3rd ed. Muscat, Ministry of Health, 2003:3.
- Communicable disease surveillance and control. A standard operating procedures manual, 2nd ed. Muscat, Ministry of Health, 2005:42.
- Ministry of National Economy. General Census for population, housing and establishments ( http://www.omancensus.net/english/index.asp, accessed 16 October 2007).
- 9. World Health Organization, Regional Office for the Eastern Mediterranean. Country profiles. Oman (http://www.emro.who.int/emrinfo/index.asp?Ctry=oma, accessed 4 October 2007).
- Brown DWG et al. Salivary diagnosis of measles: a study of notified cases in the United Kingdom, 1991–93. British medical journal, 1994, 308:1015–17.
- Southern African countries eliminate measles death in 2000. Vaccine preventable diseases bulletin, 2001, 8:1–2 (http://www.afro.who.int/ddc/vpd/bulletins/2001/feb2001.pdf, accessed 22 October 2007).
- Ramsay M, Cohen B, Brown D. Serum IgM testing is needed in all cases of suspected measles British medical journal, 1996, 313:23l.
- Miller E. The new measles campaign. Immunization should prevent an epidemic predicted by modelling. British medical journal, 1994, 309:1102–3.
- Centers for Disease Control and Prevention. Measles – United States, 1995. Morbidity and mortality weekly report, 1996, 45:305–7.
- Peltola H et al. The elimination of indigenous measles, mumps, and rubella from Finland by a 12-year, two-dose vaccination program. New England journal of medicine, 1994, 331:1397–402.
- Pederson IR et al. Subclinical measles infection in vaccinated sero-positive individuals in arctic Greenland. Vaccine, 1989, 7:345–8.
- Ministry of Health. Oman’s progress towards measles elimination. Community health and disease surveillance newsletter, 2000, 9(1):1–4.
- Gindler JS et al. Epidemiology of measles in the United States in 1989 and 1990. Pediatric infectious diseases journal, 1992, 11:841–6.
- Hutchins S et al. Measles outbreaks in the United States, 1987 through 1990. Pediatric infectious diseases journal, 1996, 1:31–8.
- Centers for Disease Control and Prevention. Progress toward elimination of measles from the Americas. Morbidity and mortality weekly report, 1998, 47:189–93.
- 21. Marwick C. National effort to immunize adolescents begins. Journal of the American Medical Association, 1996, 276:766–8.
- Davis RM et al. A persistent outbreak of measles despite appropriate prevention and control measures. American journal of epidemiology, 1987, 126:438–49.
- Min-Shi Lee, D James Nokes. Predicting and comparing long-term measles antibody profiles of different immunization policies. Bulletin of the World Health Organization, 2001, 79(7):615–24.
- Lee MS et al. Post mass-immunization measles outbreak in Taoyuan County, Taiwan: dynamics of transmission, vaccine effectiveness and herd immunity. International journal of infectious disease, 1999, 3(2):64–9.
- Ceyhan M et al. Immunogenicity and efficacy of one dose measles-mumps-rubella (MMR) vaccine at twelve months of age as compared to monovalent measles vaccination at nine months followed by MMR revaccination at fifteen months of age. Vaccine, 2001, 19(31):4473–8.
- Papania M et al. Increased susceptibility to measles in infants in the United States. Pediatrics, 1999, 104:59.
- Watson JC, Hadler SC, Dykewicz CA, Reef S, Phillips L. Vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). Morbidity and mortality weekly report, 1998, 47(8):1–57
- Centers for disease control and prevention (CDC). Measles outbreak associated with an imported case in an infant – Alabama, 2002. Morbidity and mortality weekly report, 2004, 53(2):30–3.
- Cutts F, Markowitz L. Successes and failures in measles control. Journal of infectious diseases, 1994, 170(Suppl. 1):32–42.
- Poland GA et al. Measles re-immunization in children sero-negative after initial immunization. Journal of the American Medical Association, 1997, 277:1156–8.
- Ramsay M et al. The epidemiology of measles in England and Wales: rationale for the national vaccination campaign. Communicable disease report. CDR review, 1994, 4(12):141–6.
- Quadros de CA et al. Measles elimination in the Americas. Evolving strategies. Journal of the American Medical Association, 1996, 275:224–9.
- Bellini WJ, Rota PA. Genetic diversity of wild-type measles viruses: implications for global measles elimination programs. Emerging infectious diseases, 1998, 4:29–35.
- Centers for disease control and prevention (CDC). Measles Eradication: Recommendations from a Meeting Cosponsored by the World Health Organization, the Pan American Health Organization, and CDC.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)