R. Busulwa,1 M.Y. Takiyaddin,2 A.A. Azzubeidi,3 H. El Zein El Mousaad,1 J. Tawillah4 and H. Ziady5
ABSTRACT An HIV/AIDS situation analysis in Yemen was conducted in 2002 to assess knowledge and attitudes towards the male condom as a means of HIV prevention. Data were collected from 3 groups: the general population, a marginalized minority group and Yemenis returning from extended work abroad. Only 51.3% had ever heard of the male condom; of these, just 45.5% were aware of its protective benefit against infection. The major constraint to condom promotion was concern that it would undermine the sexual norms of the country. Reduction in sensation and doubts about its preventive efficacy were further constraints. Nonetheless, over 21% approved of condom promotion among high-risk groups.
Perceptions du préservatif comme méthode de prévention du VIH au Yémen
RÉSUMÉ Une analyse de la situation relative au VIH/SIDA a été réalisée au Yémen en 2002 pour évaluer les connaissances et attitudes concernant le préservatif masculin en tant que moyen de prévention du VIH. Des données ont été recueillies auprès de 3 groupes : la population générale, un groupe minoritaire marginalisé et des Yéménites rentrant au pays après une longue période de travail à l’étranger. Seuls 51,3 % avaient déjà entendu parler du préservatif masculin ; et parmi ces derniers, seulement 45,5 % étaient conscients de l’intérêt du préservatif dans la protection contre l’infection. La contrainte majeure pour la promotion du préservatif était la crainte qu’il n’affaiblisse les normes sexuelles du pays. La diminution des sensations et les doutes sur son efficacité préventive constituaient d’autres contraintes. Néanmoins, plus de 21 % approuvaient la promotion du préservatif dans les groupes à haut risque.
1WHO Representative Office, Khartoum, Sudan (Correspondence to R. Busulwa:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
2National AIDS Programme, 3Health Policy and Technical Support Unit; Ministry of Public Health, Sana’a, Yemen.
4WHO Representative Office, Djibouti.
5HIV/AIDS and Sexually Transmitted Diseases Unit, Division of Communicable Diseases, WHO Regional Office for the Eastern Mediterranean, Cairo, Egypt.
EMHJ, 2006, 12(Supplement 2): 64-77
Introduction
Yemen is listed among the 20 least developed countries in the world. Some of the available development indicators for 2001 were as follows: a population of 18.9 million growing at 3.5% per annum, GDP per capita of US$ 492 and illiteracy rates of 50% and 65% for men and women respectively [1]. Infant and under-5 mortality rates have been reported at 75 and 102 per 1000 live births respectively, with maternal mortality at 365 per 100 000 [2]. Other data indicate only 50% of the population have access to essential drugs, just 22% are attended by skilled health personnel [3], and only 45% have adequate sanitation facilities [4]. A 1998 household budget survey found that 17.6% of the population were living below the food poverty line, and 41.8% were living below the upper poverty line, being unable to obtain both their food and non-food requirements: clothing, shelter, health education and transport [5].
Yemeni culture is strongly influenced by Islamic values, with extramarital sex being considered extremely shameful and stigmatizing for the individual and even the family. Sex between men is also taboo, although the anecdotal indications are that traditional sanctions against it may be less severe than those against extramarital heterosexual relations (for instance, reported instances of “honour killing” mostly in the past, were almost invariably for heterosexual relations). Despite this culture, many health care providers have admitted to seeing increasing numbers of patients with symptoms consistent with sexually transmitted infections (STIs), and the phenomenon of men having sex with men is known to exist in the country. There are no indications of the occurrence of injecting drug use in the country.
The prevalence of human immunodeficiency virus (HIV) infection in Yemen remains unknown because, to date, no seroprevalence studies have been undertaken. The cumulative number of cases reported to the National AIDS Programme (NAP) was 1379, as of December 2003 [6]. There are indications that because of stigma and harassment, including police arrests in the past, people who know or suspect themselves to be HIV-infected, avoid testing if they can. This fact, together with the still limited capacity to diagnose HIV in the health services, would suggest that the cases notified to the NAP are just the tip of the iceberg.
Globally, condoms are an important option in the fight against HIV/AIDS. Solid epidemiological studies have shown that condoms are effective for HIV prevention, and consistent use can reduce transmission probability by as much as 95% [7]. These include studies carried out among sero-discordant couples [8,9] and studies done in countries such as Uganda where a decline in HIV rates has been well documented and condoms have been an integral part of the success story [10].
A study conducted during 2002, with the joint support of the United Nations Development Programme (UNDP), the World Health Organization (WHO) and the Yemeni NAP provided an opportunity to explore perceptions of this important method of HIV prevention in the Yemeni context. Because of still limited availability and familiarity with the female condom in the country, the study’s focus on condoms was limited to the male condom. This paper presents some of the findings of the study.
Methods
The study was conducted in the 4 governorates of Hodeidah, Taiz, Aden and Hadramawt. The 4 were selected by the NAP because, along with Sana’a city which was covered by an earlier study, coordination mechanisms for execution of the study existed in these areas. In addition, the increasing numbers of diagnosed cases indicated vulnerability of the population in these governorates to HIV/AIDS. Data were collected during June–August 2002, using both qualitative and quantitative methods. Qualitative findings were factored into modifications of the quantitative survey questionnaire.
Study population
Respondents were selected from the general population from both rural and urban areas and included married and single individuals as well as students and out-of-school youth. In addition to the general population, other groups recognized as vulnerable or high-risk groups were included in the study. These were returnee families, truck drivers, fishermen, members of the marginalized group Al Akhdam, women engaged in commercial sex (CSWs) and men who have sex with men (MSM). For the purposes of the study and this paper, the term “marginalized group” is used to refer to the group name Al Akhdam, as this name is considered offensive by some in the group. Returnee family respondents were operationally defined as those who either themselves or at least one of their parents had returned to Yemen after a period of more than 4 years outside the country. This was intended to exclude those who had been out of the country on short visits or for academic courses. Additionally, for the qualitative data, national and governorate level policy-makers and health service providers were also recruited.
Respondents were aged 15 to 49 years and gave verbal consent to participate in the study. In addition, in consideration of local culture, the permission of the responsible male relative, if available, was sought for females and adolescent respondents.
Qualitative methods
These consisted of 49 key informant interviews and 45 focus group discussions (FGDs). The selection of these respondents was different from that for the quantitative survey, which followed 2 months later. Key informants were interviewed individually and were selected either because they were accessible and representative or because they were very knowledgeable of the groups under study. National and governorate level policy-makers and reproductive health service providers were also selected as key informants. Further categorization of target groups included: in-school and out-of-school young people, and married men and women. Selection was made in such a way as to ensure that, availability permitting, these categories were accessed in all the governorates, in both urban and rural areas. CSW and MSM individuals were selected as key informants through networking with knowledgeable resource persons in the communities, and using individuals identified to establish contact with others of a similar lifestyle.
Key informants were interviewed in a variety of convenient and feasible locations that guaranteed privacy of the discussions and where the informants were at ease. These locations ranged from offices, restaurants, hotels or public parks.
The FGDs consisted of 8–12 participants of similar sex, marital status, rural or urban residence or residence in identified target group communities. In addition, separate FGDs were conducted for in- and out-of-school youth, with different groups for either sex. Local mobilizers helped in identifying participants in each location who were willing to participate in the FGD sessions.
Both key informant interviews and FGDs were moderated using topic guides that covered perceptions of condoms, along with care and support to people living with HIV/AIDS, observed sexual risk behaviour in the communities, factors related to HIV/AIDS vulnerability, as well as attitudes to potential local HIV/AIDS interventions. The interviews and FGDs were conducted by social science/public health personnel who were selected and trained by the principal investigator. Interviews and discussions were conducted by personnel of the same sex as the key informants, except for the CSWs because the female personnel were reluctant to interview them.
FGD proceedings were recorded in writing by recorder personnel, as well as by audio cassette, with the permission of the participants. Only written notes were taken during key informant interviews. Following the interviews and discussions, the notes were rewritten comprehensively, and submitted to the principal investigator. Audio tape recordings were transcribed and also reviewed by the principal investigator in order to transform the initial FGD recorder notes into session reports that were entered into a word processing program (Microsoft Word) for analysis. Key informant interview reports were similarly entered into the program and all the data were coded, sorted and analysed in terms of the initially conceived themes as well as the ones that emerged as the study proceeded.
Quantitative methods
This was based on a household survey of 2579 respondents of whom 2534 were Yemeni nationals, categorized into 3 groups—the general population per governorate and 2 vulnerable groups (returnee family group and marginalized group). The remaining 45 respondents were foreign nationals whose number was too small to make any meaningful comparison with the Yemeni population sub-groups. A target minimum sample size for each category overall was derived from the formula: N = Z2pq/d2 with the level of significance set to 5%. A study questionnaire was developed by the principal investigator, also drawing from standard questions used in international studies by an international behavioural surveillance toolkit [11]. The questionnaire was revised to respond to emerging qualitative findings and pre-testing. The questionnaire covered background and demographic data, mass media access, awareness of HIV/AIDS and other STIs as well as known sexual risk behaviour by others in the communities, reported first hand to the respondent by those who had engaged in it. This “third party” determination risk behaviour was done because it did not appear likely that all individuals would correctly report their own risk behaviour in an interviewer-administered questionnaire.
Stratified, multistage random sampling was used for the general population sample, starting by the selection of 2 urban and 3 rural districts (mudiriyat) in each governorate, followed by selection of 2 parishes (oslah) in each district. Thereafter, in each selected parish 2 villages were taken; 1 at the centre of the parish and another randomly selected at least 1 km away. In the case of large cities, zones and quarters (ahia) represented parishes and villages respectively.
Because of their settlement patterns, and the need to execute the study within a narrow time frame, for the marginalized group and returnee family members, purposive sampling was used with known large settlements of the groups being identified and sampled. This resulted in a relative over-
representation of urban respondents for these groups, something that was borne in mind during rural/urban comparison analysis.
In each selected village or settlement, interviewers travelled in randomly determined but perpendicular directions, interviewing 1 respondent of their sex per household. Where there was more than 1 willing eligible respondent, just 1 was selected by casting lots. After interview, 3 subsequent household(s) were skipped in the general population and 1 was skipped in the returnee and marginalized groups sampling.
The completed questionnaires were reviewed for completeness and subsequently entered into SPSS, which was used in the quantitative analysis.
Results
Awareness of HIV/AIDS and other STIs
The vast majority of respondents in the 3 groups sampled in the quantitative survey (general population, returnee family group and marginalized group) had ever heard of HIV/AIDS (84%–92%), but specific knowledge of modes of transmission of HIV was lower (67%–89%). This was further indicated by concurrently high levels of false beliefs such as HIV being transmittable by touch, clothing, sharing a meal and mosquitoes, held by 24%–58% of those who had ever heard of HIV/AIDS. More males, urban residents and those who had ever attended school knew of these diseases than females, rural residents and school non-attenders and the difference was statistically significant (P < 0.001) (Table 1).
Prevailing sexual risk behaviour
There was almost complete consensus among key informants and FGD participants that sexual risk behaviour was on the increase. Reproductive health care service providers were also more or less unanimous that they were witnessing an increase in the frequency of patients with symptoms consistent with STIs.
“Life has changed. In the past we heard about all these behaviours but not as much as today…. [Now] everything is done openly. Nobody cares if it’s right or wrong.” Female secondary school student FGD.
From analysis of the qualitative data, growing poverty, a sociocultural transition, variations in the sexual subcultures between sections of the Yemeni population, and population movements including a migrant worker tradition, emerged as the factors underlying sexual risk behaviour.
The quantitative survey indicated that in the general population, 19.2% of males had been told personally by another male that such a male had had extramarital sex (heterosexual) over the preceding 12 months. In addition, 8.8% of males had first-hand knowledge of others who had had sex with other males over the same period. Rates of male-reported third-party risk behaviour were higher among respondents from returnee and marginalized families, although this was only statistically significant for reports of MSM (Figure 1). The quantitative survey also revealed that 6.4% of all males had had an abnormal genital discharge over the preceding 12 months, this rate rising to 24.0% for female respondents, although this would be less specific for STI than for males [12].

Awareness of male condoms
Apart from the general population, where 51.3% had heard of the male condom, less than half of the respondents in any of the population groups sampled had heard of it. At 36.3%, this awareness was significantly lower among respondents from the marginalized group (P < 0.001). Furthermore, in all respondent categories, no more than 45.5% of all those who had ever heard of the condom knew that it could also prevent STIs. Overall, therefore, the fact that a condom could prevent STIs was known by less than 23% of all respondents in any respondent category (Figure 2).
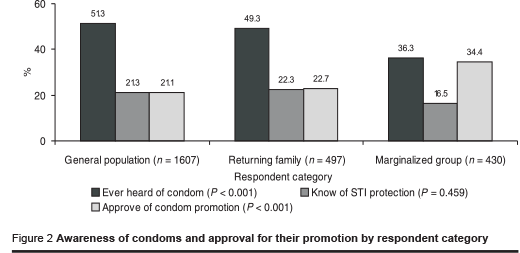
Condom awareness was further examined by sex, residence and schooling. Awareness of the male condom, both by having heard of it and by knowing it as a method of family planning was significantly higher among males and those who had ever been to school. The difference by residence was examined only among general population respondents (to avoid the potential urban over-representation resulting from the purposive sampling of the other 2 population groups sampled). This yielded a significantly higher awareness of condoms among the urban than rural general population respondents, 55.0% and 45.3% respectively (P < 0.001) (Table 1).
Knowledge of sources of and access to condoms
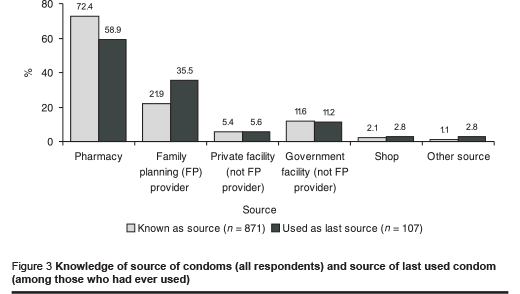
From the qualitative data, most key informants and FGD participants in the urban areas knew where condoms could be obtained. However, there were barriers of cost reported for the poor, as well as the requirement of marital status verification before issue of condoms at some government health facilities. This latter requirement effectively excluded many members of high-risk and vulnerable groups from access to the lowest cost condoms.
Quantitative survey findings indicated that pharmacies were the most widely known source, more often named than all other sources, including various categories of health facilities combined. Despite the higher cost, pharmacies were also the most frequent source of the last condom used, again more often used than all the other sources combined. There were no statistically significant differences in awareness of the various sources by respondent category (Figure 3).
Use of condoms
Qualitative findings indicated that condom use was rare even among the high-risk groups, with the possible exception of some female sex workers in 1 city.
“Many people don’t like to use the condom. I find myself forced to do it [sex] without a condom.” Female sex worker key informant.
“No one is using the condom with me because I know my clients very well we trust each other.” Female sex worker key informant.
“There are some girls who carry condoms in their handbags. I have practised sexual intercourse with one of those girls. She asked me to use it but I refused. I think most people don’t use condoms because they don’t like [them].” High risk heterosexual male key informant.
“I don’t use a condom at all. I don’t know what it is.” Man who has sex with men key informant.
“No one is using the condom with me, because people who engage in risk behaviour don’t feel enjoyment if they use condom. I never used it and no one has used it with me. …. I never thought about it.” Man who has sex with men key informant.
Despite the indicated low level of use, several health care providers reported a noticeable increase in uptake of condoms for family planning. There were reports that some among the rich and educated were using condoms more readily than the rest of the population.
“There are a lot of married and educated youth using the condom because they care about their health. It is a good idea to use condoms, and there will be no problem [with the policy] except it doesn’t give you enjoyment during sex.” Returnee family male FGD participant.
There was also open demand for a good quality condom supply and condom education from some members of the vulnerable groups such fishermen in 1 coastal city.
From the quantitative survey, it emerged that only 2% of the total survey sample had used a condom for any reason in the preceding 12 months. This rate rose to 6% of those who had ever been married, and among users of modern family planning methods 9% had used a condom in the previous 12 months. Condom use for family planning or otherwise was reported more frequently by males, those who had ever been to school, and for urban dwellers amongst the general population respondents. However this was only statistically significant for those living in urban areas and who had ever been to school (Table 1).
Overall constraints to condom use
The commonest reported constraint to condom use among high-risk individuals was the experience of reduced pleasure, reported by both male and female informants.
“Condoms are not being used at all by truck drivers because people are not aware of how to use them, and if they use them they don’t feel enjoyment.” Truck driver key informant.
“People who pay for sex don’t normally use the condom. They say ‘we pay money to enjoy ourselves, with the condom there is no enjoyment’.” Female sex worker key informant.
More generally, some respondents opposed the promotion of condoms for HIV control because they were not even 100% safe for birth control, let alone HIV prevention.
“There is no benefit from this condom, because it is not even [fully] safe for family planning. How could it be safe for prevention of AIDS?” Urban married man FGD participant.
“If the condom is not safe for family planning how can we use it to protect ourselves from AIDS?” Rural married woman FGD participant.
Some fishermen also complained of frequent breakage of condoms, raising questions about the quality of the condoms available to end-users in the hot coastal areas. Other respondents occasionally mentioned the belief that repeated use of condoms would lead to genital irritation, infection and even cancer in women.
Opposition to condom promotion
Most FGD participants and key informants opposed the idea of promoting the use of the condom for HIV/AIDS and other STI prevention in the country. Dissemination of information on any benefits of condom use was opposed because of the belief that such awareness would remove the fear of the negative consequences of extramarital sex, such as pregnancy and disease, leading to an increase in such behaviour. Dissemination of such information was seen to undermine the traditional deterrents to “illegal” sex, namely the threat of these negative consequences. For some people holding such views, any increase in condom use, even among high-risk groups such as MSM, would be a negative development.
Some respondents, including well educated youth, even believed that condom promotion would result in a net increase, instead of a decrease in STIs.
“No, we should not encourage the use of condom or the spread of condom because this can cause the spread of diseases and other dangerous behaviours. No, it is forbidden. It is not allowed” Female university student FGD participant.
“When someone uses a condom as prevention against AIDS, this indirectly helps in the spread of AIDS and other wrong behaviours” Urban woman FGD participant.
For a large section of the population that included health care providers, preserving the morals and the traditional sexual norms was of greater importance than preventing the spread of HIV. If HIV reduction interventions reduced the spread of infection but left the rate of “illegal” sex higher, this would be a negative development, in their view.
“In our country we don’t need the condom at all. We should not worry about AIDS more than we worry about its cause which is illegal sex. Instead of educating people on condom use, you should educate them to stop “illegal” sexual behaviour... We must not educate people that “illegal” sex is forbidden, then [after that] educate them that you can practise it with a condom.” Urban married man FGD participant.
“Socially, we are against this idea of condom use, because you are trying to solve the problem by using its very cause! If AIDS is a result of “illegal” sex behaviours, we [would be] increasing the level of this behaviour by providing condoms. There is no need to open doors that are going to create a lot of problems in the community. With this policy you are calling us to follow the West and forget about our faith, religion and traditions.” Policy-maker key informant.
“Those who are engaged in bad behaviour will accept it [the condom], even if there is a poison in it. But why do you make what is haram (sinful) in Islam, halal (acceptable)?” Health care provider key informant.
The sentiment of the need to “protect” people from condom promotion was such that, in one FGD, it was even recommended that any condom use among couples where 1 partner was already infected with HIV, be kept secret, so that knowledge of such use would not spread to the rest of the community. In several FGDs, stern enforcement of laws against sexual risk behaviour by the government, rather than disseminating information on the condom’s potential protection, was seen as the most important step to take to control the spread of HIV. In another FGD, it was even recommended that the government should punish people promoting condom use for “increasing illegal sex” in the community.
Health care providers and condom promotion
Support for condom promotion was more frequently voiced among health care providers than other respondents, and in all the governorates many of them expressed readiness to participate in educating people about condoms. They saw the obstacles faced as surmountable, just as those against other modern methods of family planning had been overcome in the past. Experienced health care providers, who often saw cases of STI on a regular basis, more readily recognized the necessity for condom promotion.
However, there was a perception that making extramarital sex safer was tantamount to legitimizing it, leading to a conscious decision by some health care providers to withhold information on the STI-protective benefits of condoms from their clients. In one FGD of health sector policy-makers, the group was so sharply divided on this issue that there was danger of the discussion turning violent, and some participants finally walked out in protest.
“If ‘illegal’ sex is forbidden in our religious guidelines, how can we encourage condom use? Do you want us to tell people who want to have ‘illegal’ sex to use the condom in order to prevent AIDS? This is unbelievable.” Health sector policy-maker FGD participant.
Another constraint was that most health care providers had inadequate skills and lacked the necessary tools (such as dildos) to demonstrate correct condom use. Shyness and fear of the stigma that could be attached to someone promoting or demonstrating details of condom use were also evident.
“If one goes into details [of steps of proper condom use], the clients will imagine that the provider is not a good person, that she is probably promiscuous, and that she is also encouraging the wives to engage in bad behaviour [‘illegal’ sex].” Midwife trainer key informant.
Furthermore, because most of the reproductive health service delivery is done by female providers, information provided on condom use in reproductive health settings would have to be mediated via the females in order to reach their male partners. This indirect route could jeopardize the accuracy of the information that would eventually reach the males.
Broader support for condom promotion
Despite widespread opposition to condom promotion, there was at least a minority of participants in almost all FGDs supporting it, at least for high-risk individuals. Even in FGD sessions where the opposition was very strong, recognition of the difficulty in getting all individuals engaged in risk behaviour to stop it, led to expressions of tolerance for condom promotion, if it was limited to high-risk groups.
“If the condom is going to be distributed in special places, such as those that deal with commercial sex work, it is no problem because it is not easy to stop them. But giving condoms to those people should be followed by health education on the dangers of these diseases” Urban married man FGD participant.
“For those perverts [who have extramarital sex] if we offer the condom, it is good. But more important than the condom is poverty reduction and health education, especially in secondary schools.” Female reproductive health service provider FGD participant.
In the quantitative survey, respondents were asked whether condom promotion ought to be carried out for individuals who persist with extramarital sex, as is done in some other countries, as part of routine interventions, especially those targeting high-risk and vulnerable groups. Over one-fifth of respondents in each of the 3 main categories supported such condom promotion. At 34.4%, this support was highest among the marginalized group, and overall, was significantly higher among males, those who had attended school and among the urban general population respondents (Table 1, Figure 1).
Discussion
Globally, constraints to condom use are similar across countries and continents and include factors such as reduced sensation, concerns on reliability, unavailability or inaccessibility, low-risk perception, as well as psychological and social factors including gender relations [13]. Various combinations of these factors have been reported by studies from Jamaica [14], Uganda [15,16], Australia [17], China [18] and the USA [19,20].
Our study reveals a low awareness of the condom in general and of its STI protective benefit in particular, co-existing with low levels of use in a context of consistent reports of increasing occurrence of sexual risk behaviour, even in the general population. The study finding that 19.3% (close to 1 in 5) of general population males had been told first hand of heterosexual extramarital sex by other participating males over the preceding 12 months indicates a significant occurrence of sexual risk behaviour. Even among those individuals who knew of the condom’s STI prevention benefit, knowledge of the correct steps of its proper use was very limited. Given the consistent reports from both key informants and FGDs, that sexual risk behaviour was on the increase, it is important to find a culturally acceptable role for the condom in the prevention of HIV/AIDS and other STIs.
Given the broader scope of the study, full exploration of the effect of socio-economic factors in condom awareness and use was not possible. However, the lower awareness found among women, the less educated and rural residents highlights the need to address this disparity in knowledge and the consequent vulnerability of these groups of the population. That the difference in reported condom use by sex was not statistically significant, suggests that most condom use may be between males and females, even though the method might still be male-driven or male-led.
Pharmacies were the most frequently known source of condoms, and they were the most frequent source of the last condom used. The popularity of pharmacies indicates readiness of the Yemeni population to access condoms through social marketing approaches, and these are already being exploited. The greater degree of anonymity for the buyer and the longer opening hours of pharmacies compared with health facilities are some of the advantages of this source.
The strong sentiments expressed against condom promotion indicate the need for any efforts at promotion to pay due attention to these sensitivities. Nonetheless, considering the conservative cultural context and low awareness, the fact that over one-fifth of the respondents supported condom promotion indicates potential for increased acceptance with more sensitization. The general increase in acceptance of modern family planning methods over time supports this impression.
The levels of sexual risk behaviour and syndromic symptoms of STIs found by our study indicate that the condom is likely to remain a much-needed weapon in the arsenal against HIV/AIDS in the country, at least in the short and medium term. Opponents of condom promotion include health sector policy-makers and service providers. However, because some members of these groups have already resolved the conflicts in their own minds and come out in favour of condom promotion, it is reasonable to assume that debate and discussion among health professionals could result in the identification of acceptable ways for their participation in condom promotion and distribution activities. This could be enhanced by highlighting that the use of condoms by individuals engaged in risk behaviour would protect the “innocent” spouses of these individuals and their unborn children who are not party to such behaviour. Because the condom has increasingly become accepted as a method of birth control, it is possible within this context to increase awareness of its proper use, and its STI-protective benefit, without unduly offending cultural sensitivities. Indeed the national HIV/AIDS strategy, approved by the Cabinet in December 2002, takes the approach of “complementing traditional cultural and religious values, such as abstinence and marital faithfulness, with information on the protective benefits of the condom in settings of risk behaviour” [21]. Nonetheless there are significant challenges to the use of the condom for HIV/AIDS prevention in Yemen as illustrated by our study which need to be addressed and any efforts to promote its contraceptive and STI prevention benefits must take account of cultural sensitivities.
Acknowledgements
The authors are grateful for the support of the following officials in Yemen: the Ministry of Public Health and Population, Mr James Rawley and Mr Abdo Seif of the UNDP Office, and the many national personnel who collected the data for this study.
References
- Yemen common country assessment. Sana’a, Yemen, United Nations Development Programme, 2001.
- The National Family Health survey. Sana’a, Yemen, Central Statistics Organization, Ministry of Planning, 2003.
- Yemen demographic and maternal and child health survey, 1997. Sana’a, Central Statistical Organization (Yemen) and Calverton, Maryland, Macro International, 1998.
- World Development Report 2000/2001: Attacking poverty. Washington DC, The World Bank, 2001.
- Household budget survey, Sana’a Central Statistical Organization, 1998.
- HIV/AIDS surveillance report, fourth quarter 2003. Sana’a, National AIDS Programme, Ministry of Public Health and Population, 2003.
- Workshop summary: scientific evidence on condom effectiveness for sexually transmitted disease (STD) prevention. Bethesda, National Institutes of Health (NIH), US Department of Health and Human Services (www.niaid.nih.gov/dmid/stds/condomreport.pdf, accessed 30 November 2005).
- Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Social science and medicine, 1997, 44:1303–12.
- DeVicenzi I. A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. New England journal of medicine, 1994, 331:341–6.
- Hogle JA, ed. What happened in Uganda? Declining HIV prevalence, behaviour change, and the national response. Washington DC, US Agency for International Development, 2002.
- Behavioral surveillance surveys: guidelines for repeated behavioral surveys in populations at risk of HIV. Durham, North Carolina, Family Health International, 2000 (http://www.fhi.org/en/HIVAIDS/pub/guide/bssguidelines.htm, accessed 6 June 2006).
- Guidelines for sexually transmitted infections surveillance. UNAIDS/WHO Working Group on Global HIV/AIDS/STI Surveillance. Geneva, World Health Organization, 1999 (WHO/CDS/CSR./EDC/99.3).
- Spryut AB, Finger WR. Acceptability of condoms—user behaviors and product attributes. In: McNeill ET et al., eds. The Latex condom, recent advances, future directions. Durham, North Carolina, Family Health International, 1998.
- Spryut A et al. Dual method use among family planning clients, Kingston, Jamaica. Paper presented at the 124th Annual Meeting of the American Public Health Association, New York, 17–21 November, 1996.
- Rwabukwali CB et al. Culture, sexual behaviour, and attitudes towards condom use among Baganda Women. In: Feldman DA, ed. Global AIDS policy. Westport, Bergin and Gorvey, 1994:70–89.
- Kamya RM et al. Predictors of condom use in Kampala Uganda. Paper presented at the 10th International AIDS Conference, Yokohama, Japan, 7–12 August, 1994.
- Richters J, Donovan B, Gerofi J. How often do condoms break or slip off in use? International journal of STD & AIDS, 1993, 4:90–4.
- Lin L et al. Improving condom use in Sichuan, China: findings from a qualitative study. Reproductive health matters, 1996, 7:101–6.
- Grady WR et al. Condom characteristics: the perceptions and preferences of men in the United States. Family planning perspectives, 1993, 25:67–73.
- Choi KH, Rickman R, Catania JA. What do US heterosexual adults believe about condoms? [Letter]. New England journal of medicine, 1994, 331:406–7.
- National strategic framework for the control and prevention of HIV/AIDS in the Republic of Yemen. Sana’a, Yemen, Ministry of Public Health and Population, December 2002.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)