A.J. Choudhry,1 K.S. Al-Mudaimegh,2 A.M. Turkistani1 and N.A. Al-Hamdan1,3
ABSTRACT A prospective cohort study was conducted to estimate the incidence of acute respiratory infections (ARI) among hajjis registered at primary health care centres of Riyadh. Out of 1027 hajjis, 39.8% developed symptoms of ARI. The incidence of ARI was not statistically significantly associated with age, sex, educational status or smoking. The risk of illness was significantly higher among diabetics, hajjis who stayed longer in the hajj area and who prayed at Namera mosque. Use of a facemask by men, but not use of a facecover by women, was a significant protective factor against ARI.
Infection respiratoire aiguë associée au Hadj chez des pèlerins de Riyad
RÉSUMÉ Une étude de cohorte prospective a été réalisée pour estimer l’incidence des infections respiratoires aiguës (IRA) chez des pèlerins enregistrés dans des centres de soins de santé primaires de Riyad. Sur les 1027 pèlerins, 39,8 % ont développé des symptômes d’IRA. Il n’y avait pas d’association statistiquement significative entre l’incidence des IRA et l’âge, le sexe, le niveau d’instruction ou le tabagisme. Le risque de maladie était significativement plus élevé chez les diabétiques, chez les pèlerins qui étaient restés plus longtemps dans la zone du Hadj et ceux qui avaient prié à la mosquée de Namera. L’utilisation d’un masque facial chez les hommes était un facteur de protection important contre les IRA, mais pas l’utilisation d’un voile facial par les femmes.
1Field Epidemiology Training Programme, Riyadh, Saudi Arabia (Correspondence to A.J. Choudhry:
2Infection Control and Environmental Health Department, Children’s Hospital, King Fahd Medical City, Riyadh, Saudi Arabia.
3Department of Community and Family Medicine, Riyadh, Saudi Arabia.
Received: 28/08/04; accepted: 29/12/04
EMHJ, 2006, 12(3-4): 300-309
Introduction
Acute respiratory infections (ARIs) are the most common infections among humans, accounting for 35% of communicable disease consultations in primary care [1,2]. Yet even with such a high prevalence, respiratory infections receive only 0.15% of the research and development budget for health [3].
The hajj represents a major challenge to the Saudi Ministry of Health in addressing infection control at this gathering of over 2 million people. Infection hazards at the hajj include meningococcal meningitis, respiratory tract infections, blood-borne diseases and zoonotic diseases, all of which have domestic and international ramifications as Muslim pilgrims return home [4]. However, leaving aside the threat of meningococcal meningitis, the importance of other infectious diseases is generally not appreciated. ARIs are considered a low priority health problem due to the low risk of mortality and complications, except in physically debilitated and immunocompromised people [3]. However this attitude undermines their importance due to high infectiousness, capacity to lower the general immunity and high short-term disability.
In an attempt to identify the etiology of ARI in hajj, a study during the 1991–92 CE pilgrimage season found bacterial pathogens in 29.9% of sputum specimens and throat swabs and viruses in 19.5% [5]. Another study conducted in hajj 2001 CE of selected clinical influenza cases among pilgrims visiting outpatient clinics in Mecca and Medina hospitals found 14.8% were seropositive. Among seropositive cases, 60% were influenza type B, 27% were type A, and the rest were positive for both types A and B [6].
A large number of domestic hajjis complain of ARI immediately after returning from hajj. Except for a few cross-sectional studies giving some idea of the causative organisms, no systematically collected information is available about the magnitude and distribution of the problem. In the absence of such information, it is not possible to assess the burden of illness on the health care system or the need for preventive measures. This study in Riyadh was conducted to assess the incidence of hajj-related ARIs among domestic hajjis in the hajj of 1423 AH (2002 CE), and to identify the risk factors associated with these illnesses.
Methods
The study was designed as a prospective cohort study to estimate the incidence of hajj-related ARIs among hajjis travelling from the capital of Saudi Arabia, Riyadh city (population approximately 4 million). It is mandatory for all hajjis to have a valid certificate of vaccination against meningococcal meningitis, which is available free of charge in Saudi primary health care (PHC) centres for both Saudi Arabian nationals and non-Saudis prior to the hajj season. This provided a good opportunity to recruit the study cohort.
Sample
After developing the study protocol, permission was obtained from the Saudi Ministry of Health to conduct the study. In the absence of any previous study estimating the incidence of post-hajj ARI, incidence was assumed at 50% (to obtain the maximum sample size for a given level of precision). With a precision of 3% around the assumed incidence at a confidence level of 95%, a sample size of 1066 was calculated. To recruit the cohort, a single-stage stratified random cluster sampling technique was used. A list of all the 72 PHC centres was obtained from the Directorate of Health in Riyadh and was stratified into 5 administrative sub-regions. Two PHC centres were selected from each of these areas using a random number table. All people visiting the centres for vaccination against meningococcal meningitis were considered as the potential cohort.
Data collection
A data collection instrument was designed with several parts. Part 1 collected basic demographic information about the study subjects before the hajj: any current illness, smoking habit, history of chronic illness and vaccination against influenza. Part 2 included information about the events in hajj and later, including history of symptoms of ARI, health care sought and ARI-related practices during and after the hajj. It was filled by the investigator during the first week after the hajj through telephone contact. Part 3 included the same information but was filled 2 weeks after the hajj by telephone contacts with the hajjis who did not report any history of ARI in the first post-hajj contact.
All the directors of the selected PHC centres were visited to obtain their consent for participation in the study and information about the number of hajjis vaccinated. All the personnel responsible for vaccinating the potential hajjis were trained in filling the questionnaire.
All the potential hajjis visiting the participating primary health care centres were asked to participate in the study and those who agreed to participate were given part 1 of the data collection instrument by the nurse in the vaccination room. In the process, all people who had any ARI-like symptoms at the time of the visit were excluded from the cohort. Patients were told that they would be contacted by telephone after the hajj regarding their illness history. The recruitment continued from 10 Dhu al-Qi’da to 1 Dhu al-Hijja 1423 AH, with a total recruitment of 1560 potential hajjis.
During the first week after the hajj, the whole of the cohort was contacted by telephone by the investigating team to respond to questions in part 2 of the data collection instrument. Female doctors interviewed the female hajjis. The hajjis who did not have any ARI symptoms by the time of the first post-hajj contact were contacted again in the 3rd week after hajj, and part 3 of the questionnaire was filled.
For the purpose of this study, ARI was defined as one of the constitutional symptoms (fever, headache, myalgia) along with one of the local symptoms (running nose, sneezing, throat pain, cough with/without sputum, difficulty breathing) that developed after reaching Mecca for the hajj.
The study asked about use of a facemask among male hajjis and a facemask or a facecover (hijab/niqab) by female hajjis. At the time of this study, facemasks were not officially recommended by the Saudi Ministry of Health but they are becoming used more frequently during the hajj, especially among domestic hajjis and those from south-east Asia. Although the wearing of niqab by women is not customary for the ritual clothing (ihram) of the hajj, Saudi women prefer to cover their face even in ihram.
Data analysis
The data were entered, cleaned and analysed using Epi-Info, version 6.04. After describing the characteristics of the study cohort and ARI patients, the risk ratios with their 95% confidence interval (CI) were calculated to estimate the effect of different exposure factors on the outcome.
Results
Background characteristics
Out of 1439 persons recruited to the study, 1130 were traceable after the hajj. Among these, only 1027 actually performed the hajj for the year 1423 AH. Of these, 73.0% of hajjis were male and 79.1% were Saudi nationals. The mean age of hajjis was 33.5 years [standard deviation (SD) 11.7 years]. Regarding level of education, 114 (11.1%) hajjis were illiterate, 52 (5.1%) had received only primary school education, 114 (11.1%) intermediate school education, 336 (32.7%) high school education, and 411 (40.0%) university education.
The mode of travel showed 513 (50.0%) hajjis travelled by air, 468 (45.6%) by bus and 46 (4.5%) by car. The total duration of travel was 4 days for 46 hajjis (4.5%), 5 days for 437 (42.6%), 6 days for 411
(40.0%), 7 days for 115 (11.2%) and 8+ days for 18 (1.8%). The mean travel duration was 5.6 days (SD 0.8 days).
Among the total, 139 (13.5%) hajjis were current smokers. Eighty-three (8.1%) hajjis suffered from one or more chronic diseases: 47 (4.6%) diabetes, 19 (1.9%) a history of chronic sinusitis, 16 (1.6%) chronic tonsillitis and 16 (1.6%) bronchial asthma.
During their stay in the hajj area 281 hajjis (27.4%) visited health care centres for some medical problem. During the hajj, 477 hajjis (46.4%) never used a facemask while 550 (53.6%) used a facemask, i.e. 340 (33.1%) used it most of time and 210 (20.4%) used it some of the time. Among the males, 478 (63.7%) used a facemask at least sometimes, while among females this figure was 72 (26.0%). Among the females, 197 (71.1%) used a facecover most of time during hajj, 37 (13.4%) used it sometimes and 43 (15.5%) never used it. When combined with the facemask used by females it turned out that 248 (89.5%) women used either a facemask or a facecover for at least some of the time during the hajj. Only 31 hajjis (3.0%) prayed in Namera mosque during the hajj.
Incidence of ARI
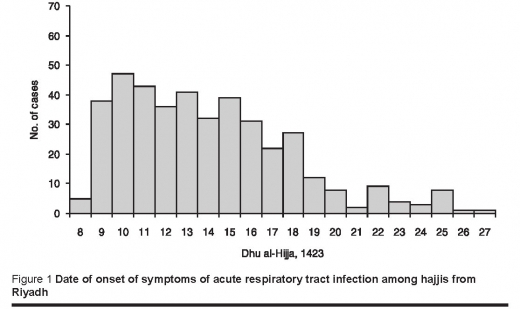
Out of the 1027 hajjis, 409 suffered from an ARI, in accordance with the case definition given earlier, during the hajj and within 2 weeks of the end of the hajj. So the cumulative incidence of ARI among the hajjis was 39.8% (95% CI: 36.8%–42.9%). The date of onset of illness ranged from 8 Dhu al-Hijja to 27 Dhu al-Hijja, while by 12 Dhu al-Hijja (the last day of hajj) 169 (41.3%) had developed symptoms of ARI (Figure 1).
Among the cases, 219 (53.5%) had a positive history of contact with ill patients. During the hajj, 281 cases (68.7%) had visited PHC centres and 298 cases (72.9%) had used an antibiotic. Only 15 cases (3.6%) were admitted to hospital due to ARI.
The small group of hajjis aged 70+ years had an ARI incidence of 83.3% compared with 37.7% among the hajjis aged < 25 years [risk ratio (RR) = 2.2; 95% CI: 1.47–3.21]. However, compared with hajjis < 25 years, the increase in other age groups was not statistically significant. Males showed a slightly higher incidence of ARI (40.4%) than females (38.3%) (RR = 1.06; 95% CI: 0.89–1.26). Non-Saudi hajjis had a cumulative incidence of ARI of 46.9%, which was 1.25 times higher than Saudi hajjis (95% CI: 1.06–1.48). There was some variation of risk of ARI among hajjis with different educational status, with the lowest risk for high-school graduates (34.8%) and highest for primary education (50.0%), but the difference was not statistically significant (Table 1).
The risk of ARI was higher for hajjis who travelled by bus (44.0%) or car (47.8%) compared with hajjis who used the aeroplane (35.3%). But the increased risk was statistically significant for travel by bus, while it was not significant for those who travelled by car compared with travel by air (Table 2). The duration spent in the hajj area showed a positive linear association with the incidence of ARI (Table 2).
Among the hajjis who used a facemask most of time during the hajj, fewer (15.0%) had ARI compared with hajjis who used it sometimes (31.4%) or never (61.2%). The risk was 2-fold among sometime users and 4-fold among never users compared with hajjis who used a facemask most of time. When the data was stratified by sex, the protective effect of a facemask was found only in men, in whom the strength of association increased on stratification, whereas using a facemask had no association with ARI among women (Table 3). For women who only used a facecover (hijjab/niqqab) there was a higher risk of ARI for occasional (43.2%) or never use (44.2%) compared with use most of time (36.0%) during the hajj, but the difference was not statistically significant. The pattern remained the same when the effect for the effect of using either a facemask or facecover (Table 3).
When the relationship of certain lifestyle factors on the incidence of ARI was studied, it was found that hajjis who opted to pray in Namera mosque in Arafat had 3.17 times higher risk of ARI compared with hajjis who did not pray in Namera mosque. Smoking, however, did not show an increase in the risk of ARI (Table 4). Suffering from a chronic disease gave a 1.46 increased risk of ARI and the difference was statistically significant (95% CI: 1.13–1.89). Among the individual diseases studied, only diabetes mellitus showed a statistically significant increased risk of ARI, while chronic sinusitis, chronic tonsillitis and bronchial asthma showed an increase in risk that was not statistically significant (Table 4).
Discussion
ARIs are a group of diseases occurring worldwide throughout the year and are not limited to any specific age, sex or nationality. Several factors contribute to the wide spread of ARIs, including direct contact with affected people, change in climate and crowded places [3]; all of these contributing factors are present in the hajj environment. As observed in other studies, the risk of viral origin ARI, especially respiratory syncitial and influenza viruses, increases during the colder months, with a peak in January and February [7]. The winter season coincides with the current dates of the hajj, so a high ARI incidence was expected. Under the circumstances, it was not surprising to find that almost 40% of the hajjis from Riyadh had an attack of ARI during and immediately after the hajj. But this high incidence of illness, even with low severity, as indicated by the low hospital admission rate, reveals a high burden of disease. As presented earlier, a large proportion of the cases developed the sickness even before they left Mecca for their homes, highlighting the inconvenience hajjis might have had in completing the rituals of the hajj and the heavy workload in the health care system in the hajj area. The problem has another dimension; ARIs are a communicable disease with high secondary attack rates [8] and thus there is great potential for ARIs to spread among the susceptible home population when the hajjis return, a problem which is further compounded by large family sizes in Saudi Arabia. However, specific post-hajj data is not available to establish the increase in the ARI cases presented in Riyadh or the rest of the country, indicating the need to study the issue of burden on the community due to a secondary wave of ARI among the non-hajjis exposed to infected hajjis.
The disease was uniformly distributed among both sexes and different nationalities, with a higher risk for older hajjis or diabetics. Both old age and diabetes mellitus are known to reduce immunity and increase the risk for ARIs and other viral infections, indicating the importance of special attention to these high-risk groups [3].
Crowdedness is also a known major risk factor for transmission of respiratory illnesses, but due to the universal exposure to crowdedness in the hajj environment, it is difficult to quantify this exposure. Visiting very crowded places such as during tawaaf (circumambulating the Ka’ba) and sa’ee (walking between Safaa and Marwa mountains) were not studied as indicators of crowdedness as they are compulsory rituals of the hajj. However, the higher risk of ARI for those praying at Namera mosque in Arafat (an optional activity) indicated that crowdedness is playing its role in the spread of ARI in the hajj environment. Further evidence of a causal relationship between the hajj and the occurrence of ARI is the positive dose–response relationship between the number of days stayed in the hajj area and the risk of ARI among hajjis.
The main question is how to reduce this heavy burden of ARI. Given the circumstances of the hajj it is almost impossible, under the current circumstances, to control the issue of crowding and exposure to contacts during tawaaf and sa’ee; and even in residential areas in Mina. The remaining alternatives to explore are personal protective measures such as vaccination, chemoprophylaxis and use of a facemask.
Keeping in view the diverse etiology of ARI, including both viruses and bacteria, the use of vaccines against one or multiple organisms does not appear to be rational [5]. However, use of influenza vaccine can be advocated for older hajjis, who were found to be at higher risk of ARI in this study and are known to have severe illness if infected by the influenza virus [3]. Similarly, chemoprophylactic use of antibiotics is not a sensible option [5]. Use of antibiotics for ARIs that are not confirmed as bacterial infections can increase the risk of developing drug resistance, with the dubious advantage of preventing a mild illness [9]. Nevertheless this study found that 63% of ARI cases had already been prescribed antibiotics to treat the symptoms of upper respiratory tract infections (URTIs). The rationale, however, for using antibiotics was not justified since according the current Centers for Disease Control (CDC) recommendations for treating ARIs, antibiotics should not be used to treat URTIs unless there is a documented bacterial infection [10].
In our study, regular use of a facemask was the most important practical protective factor, leading to a substantial decrease in the incidence of ARI. Although there is no clear research-based evidence on the effectiveness of facemasks in preventing transmission of ARIs, surgical facemasks are an established part of clinical practice. The use of facemasks has been advocated to protect people from inhalation of aerosols containing organic and inorganic particles [11]. Therefore, the CDC recommendations for the prevention of influenza include wearing a facemask [12]. Although wearing a mask may not provide complete protection from infection, it will reduce the incidence of infection by preventing droplet inhalation, which is considered one of the main modes of transmission of most URTIs.
Use of a facecover (hijab/niqab) by the women can also be considered as similar to use of a facemask. Most of the female hajjis were Saudis, who are more likely than other nationalities to cover their face during the hajj, and therefore the use of a facecover was quite frequent. But there was no evidence of a significant decrease in the incidence of ARI among women related to using a facemask or facecover. This difference from males can be explained by other customs, for example, women do not cover their face when alone in their tents with other females, and therefore have the same high risk of disease transmission in a closed environment with exposure to droplet infection. So using the facecover as a proxy for a facemask in women may be leading to misclassification of exposure status. Men, however, were using the facemask as a personal hygiene measure, independent of the place where they were.
This high proportion of ARI, along with the secondary wave of ARI in the city from which hajjis originated, is a heavy burden on the health care system. One objective of the investigation—to quantify this burden—has been achieved, but the other objective—to identify the cause—was not. In the absence of any laboratory-based evidence, it is difficult to comment about the etiology of ARI, especially when almost two-thirds of patients suffering ARIs had taken antibiotics before being contacted in the post-hajj period. Discouraging antibiotic use may be a difficult task, but more public information about the viral etiology of ARIs may be necessary.
So it is concluded that almost 40% of hajjis developed ARI during and immediately after the hajj, with a higher duration of stay in the hajj area, praying at Namera mosque and suffering from diabetes mellitus identified as the main risk factors. Using a facemask during hajj was found to be a major protective measure to decrease the risk of ARI among male hajjis.
On the basis of this study the investigators recommend that use of a facemask should be encouraged during the hajj to reduce the incidence of ARI; hajjis and health care providers should be advised not to use antibiotics for management of ARI without evidence of bacterial causation; and older people and diabetic patients should be informed about their high risk of ARI in order to adopt protective measures. Further studies should be conducted to establish the etiology of ARI among hajjis during the hajj winter season and to study the efficacy and effectiveness of the facemask in preventing ARI in the hajj as a health education based intervention trial.
Acknowledgements
We would like to acknowledge here the support of Dr Sahar Makki, Riyadh health directorate, and all the doctors and paramedical staff in the participating health care centres for their cooperation in recruiting the patients and their follow-up. We would also like to thank Dr Mona Bassurah, Dr Mona Anezi, Dr Aliya Al-Naji for their help in interviewing female hajjis. Last but not least, we would like to thank all the hajjis who participated in the study, without whose cooperation this study could not have been completed.
References
- Khoja TA, Al-Mohammad KK, Aziz KMS. Setting the scene for an ARI control programme: is it worthwhile in Saudi Arabia? Bulletin of the World Health Organization, 1999, 5(1):111–7.
- Povey G, Mercer MA. East Timor in transition: health and health care. International journal of health services, 2002, 32(3):607–23.
- Chin J, ed. Control of communicable diseases manual, 17th ed. Washington DC, American Public Health Association, 2000:425.
- Memish ZA. Infection control in Saudi Arabia: meeting the challenge. American journal of infection control, 2002, 30(1):57–65.
- El-Sheikh SM et al. Bacteria and viruses that cause respiratory tract infections during the pilgrimage (Haj) season in Makkah, Saudi Arabia. Tropical medicine and international health, 1998, 3(3):205–9.
- Kholedi AN et al. Seropositivity in clinical influenza cases among pilgrims during Hajj 1421 H. Saudi epidemiology bulletin, 2001, 8(4):27–8.
- Al-Hajjar S et al. Respiratory viruses in children attending a major referral centre in Saudi Arabia. Annals of tropical paediatrics, 1998, 18 (2):87–92.
- Graham NMH. The epidemiology of acute respiratory infection. In: Nelson KE, Willimas CM, Graham NMH, eds. Infectious disease epidemiology: theory and practice. Maryland, Aspen Publishers, 2001:439–76.
- Baron S, ed. Infections of the respiratory system. In: Medical microbiology, 4th ed. Texas, University of Texas Medical Branch of Galveston, 1996:211–6.
- Gonzales R et al. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Annals of internal medicine, 2001, 134:490–4.
- Pippin DJ, Verderame RA, Weber KK. Efficacy of face masks in preventing inhalation of airborne contaminants. Journal of oral and maxillofacial surgery, 1987, 45(4):319–23.
- Recommendations for the prevention of influenza. Morbidity and mortality weekly report, 2000, 49(RR03):1–38.








