HIV estimates
- HIV prevalence in the Region is 0.1% (low epidemic).
- The estimated number of people living with HIV (PLHIV) in the Region in 2016 is 360 000, including 12 000 children aged 0–14 years.
- 70% (252 000) PLHIV live in 3 countries Pakistan, Islamic Republic of Iran and Sudan.
- New infections have reached 37 000 in 2016 with Pakistan, Islamic Republic of Iran, Sudan and Somalia contributing to 83% of the total new infections in the Region.
- HIV mortality: 17 000 people have died of AIDS in 2016 compared to 15 000 in 2014.
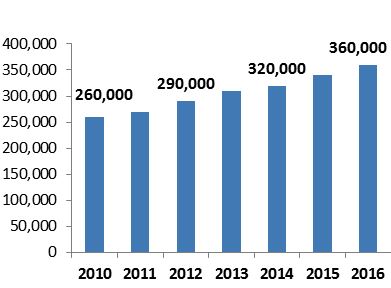
Fig. 1 Estimated number of PLHIV in the Region 2010–2016
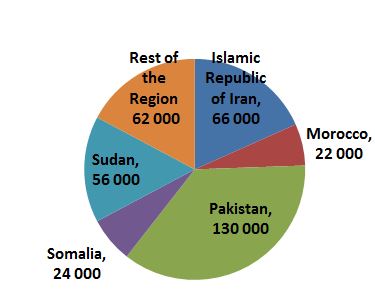
Fig 2. Distribution of PLHIV in the Region
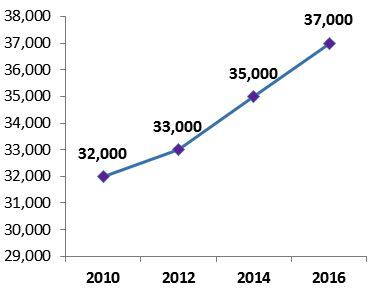
Fig. 3 New infections 2010–2016
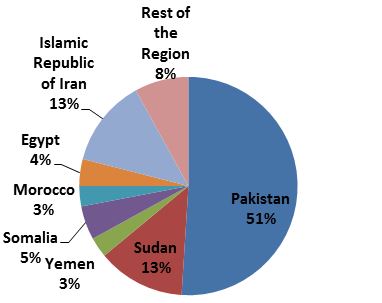
Fig 4. Distribution of new infections 2016
HIV in key populations at higher risk
- While the percentage of the general adult population living with HIV in the Region remained among the lowest globally (0.1%), key populations continue to be disproportionately affected.
- High rates of infection are found among people who inject drugs (PWID) in Afghanistan (4.4%), Islamic Republic of Iran (9.3%), Egypt (2.4%), Morocco (7.9%), Tunisia (3.9%) and Pakistan (21%).
- HIV prevalence among men having sex with man (MSM) was estimated at 12.6% in Lebanon, followed by Morocco (5.7%) and Sudan (1.4%) and Tunis (1.4%).
- HIV prevalence among sex workers: Djibouti (12.9%), Somalia (5.2%), Egypt (2.8%), and Pakistan (3.8%).
ART coverage
The number of PLHIV receiving antiretroviral therapy doubled from 2013 reaching 54 300 in 2016. Nonetheless, the Region continues to demonstrate the lowest coverage.
- 15% coverage for ART
- 18% coverage for pediatric HIV treatment
- 13% coverage for effective antiretroviral regimens to prevent mother-to-child transmission.
ART coverage varies across countries in the Region; where high ART coverage is reported in countries such as Qatar (86%), Kuwait (80%), Jordan (55%) Morocco (48%), other countries such as Afghanistan (7%), Pakistan (7%) and Sudan (10%) still have a very low coverage.
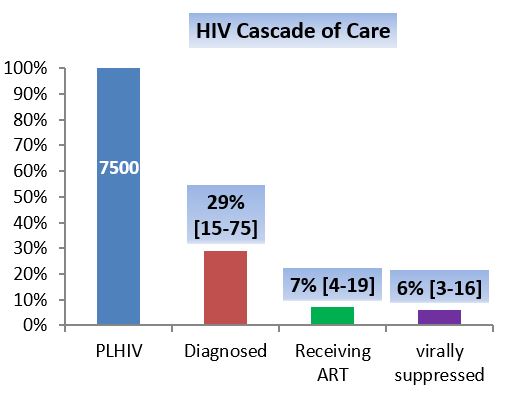
Fig. 5 HIV cascade of care in the Region
<
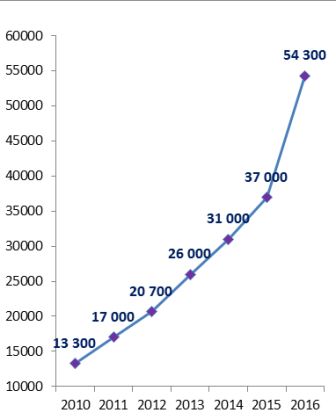
Fig. 6 ART coverage in the Region 2010–2016
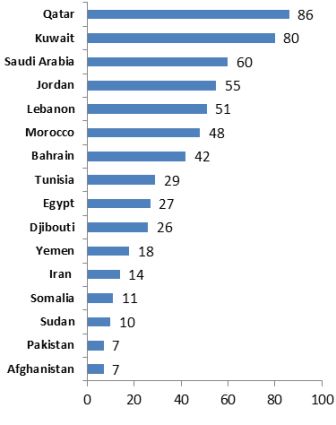
Fig. 7 ART coverage in selected countries 2016
HIV testing
- Only 30% of estimated PLHIV in the Region knew their status by 2016.
- The test-treat and retain cascade analysis conducted in Egypt, Islamic Republic of Iran, Morocco and Pakistan (Punjab) showed that 50–93% of PLHIV do not know their HIV status.
- Large numbers of people are tested in the Region but testing targets largely low-risk populations, such as migrant workers.
Testing and treatment
- Five focus countries (Egypt, Islamic Republic of Iran, Morocco, Pakistan/Punjab and Sudan) and Lebanon carried out the test-treat and retain cascade analysis and identified missed opportunities for engaging people living with HIV in the continuum of HIV testing care and treatment.
- Testing and treatment acceleration action plans to close these gaps were developed and are now being implemented in these countries.
- The Regional Office has supported countries to revise and update their HIV treatment guidelines in line with 2015 WHO recommendations which call for treatment for all.
- The Regional Office is supporting selected countries in revising their HIV testing policies and strategies and adapting the WHO HIV testing services guidelines at national level.
Strategic information
- The knowledge of HIV epidemics, though still limited in most countries, is improving, particularly among key populations at increased risk of HIV exposure.
Strategic and operational planning
- The Regional Office supports Member States to develop country-specific national responses based on the needs and priorities of PLHIV and populations at risk of HIV with the aim to contribute in reaching the WHO global targets.
Issues and challenges
National responses have been challenged by the nature of the epidemic which is concentrated in key populations at increased risk of HIV exposure. Those populations are highly stigmatized and discriminated against. Political developments in the past decade in the Region have not been conducive to de-criminalization and de-stigmatization.
Among rivalling communicable disease priorities, HIV is considered a low priority by many countries.
There is concern that HIV estimates are not very accurate in most countries of the Region because:
- the UNAIDS estimation methodology is not well adapted to low-prevalence countries
- Data on sizes of and HIV prevalence among key populations in many countries are scarce and not always of good quality. However, those data are essential for a meaningful modelling of the HIV epidemics.
The majority of PLHIV in the Region do not access HIV testing and therefore do not know their HIV status. The majority of HIV testing services use service delivery approaches that do not attract key populations (testing centralized in hospital/clinic laboratories).
While some successful service delivery approaches implemented through NGOs do exist, their reach is insufficient. Overall, there is still limited experience in countries, including among civil society organizations in implementing the most efficient approaches to increasing demand and providing HIV testing services for HIV testing among those most likely to be HIV positive. This is largely due to government restrictions on NGOs and the related lack of funding support for NGO service delivery. In the current political climate in most countries it is not anticipated that NGOs will receive more support soon.
ART coverage remains low:
- HIV test-treat-retain cascade analysis in countries of the Region shows consistently that the treatment gap is mainly the result of a “testing gap”, i.e. a gap between the estimated number of PLHIV and the number of PLHIV who know that they are infected. (However, as stated above, HIV estimates might also not be reliable).
- Access to treatment services is made difficult for key populations, in particular PWID.
- Current service delivery models are not conducive to rapid scale up of treatment (lack of integration/decentralization).
In most low-income countries of the Region, the HIV response is largely dependent on external donor funding. This is a reflection of the limited political commitment and low HIV priority given to HIV in countries.
Conclusions
- Epidemic remains concentrated in populations at higher risk.
- Still, three quarters of PLHIV carry the virus without knowing it (no prevention, no care); reaching enough and the right people with HIV testing services remains a huge challenge.
- Treatment acceleration in 2016.
- Treat all policy not yet implemented in countries with highest burden.
- Success factors: sound planning and monitoring; destigmatization; testing through community-based services; good quality of care.





 Consolidated guidelines on HIV testing services
Consolidated guidelines on HIV testing services Epidemiology of hepatitis C virus in the WHO Eastern Mediterranean Region: implications for strategic action
Epidemiology of hepatitis C virus in the WHO Eastern Mediterranean Region: implications for strategic action HIV test–treat–retain cascade analysis: Guide and tools 2017 Second edition
HIV test–treat–retain cascade analysis: Guide and tools 2017 Second edition
 Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021
Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021