Research article
A.A. Rushood,1 S. Azmat,2 M. Shariq,3 A. Khamis,4 K.A. Lakho,2 M.Z. Jadoon,5 N. Sial,2 A.A. Rushood 6 and E.A. Kamil 2
الاضطرابات العينية لدى أطفال المدارس في ولاية الخرطوم، السودان
عادل الرشود، شاه عظمت، مسعود شارق، عمار خميس، خليل لاكو، زاهد جادون، نعمت الله سيال، عبد العزيز الرشود، العاص أحمد كامل
الخلاصـة: أجرى الباحثون تحرياً شمل 1418 من المدارس الابتدائية في الخرطوم، السودان، في الفترة من 2005 – 2007، من أجل تقدير المشكلات العينية بين الأطفال ممن هم في عمر 6-15 عاماً. وتحروا 119 671 طفلاً (%56.7 منهم ذكور) بحثاً عن اختلالات واضحة في الانكسار أو اعتلال في العين الأخرى. ووجد الباحثون مشكلات عينية لدى 321 20 طفلاً (%3.03)، أما المواقع التي كان فيها أعلى معدلات الأمراض العينة فكانت كاراري %26.2، عمبادا (%21.0)، وجبل أوليه %15.7. وكان المعدل الإجمالي لأخطاء الانكسار %2.19، أما الحَسَر فكان لدى 64 100 طفلاً (%1.50) في حين شوهد مد البصر لدى 4661 (%0.70). ومن المشكلات العينية الأخرى التهاب الملتحمة والقرنية المنقول جنسياً، وعوز الفيتامين "أ"، والتهاب الملتحمة الجرثومي، والحَوَل والكثافة القرنية. ولم يتم تشخيص أكثر من 288 (%0.04) طفلاً بالتراخوما النشطة؛ وكان %86.5 منهم من موقع عمبادا في المناطق النائية من الولاية، حيث مرافق النقل سيئة والفقر منتشر على نطاق واسع. وعلى وجه الإجمال فإن %99 من أمراض العين التي تعرف الباحثون عليها كانت إما قابلة للمعالجة أو يمكن الوقاية منها. وللإقلال من هذه الأمراض ولبلوغ مرمى "الرؤية 2020" تمس الحاجة إلى برامج الصحة المدرسية العالية الفعَّالية والكفاءة.
ABSTRACT From December 2005 to June 2007, a total screening of all 1418 government primary schools in Khartoum State, Sudan, was performed to estimate ocular problems among children aged 6–15 years. We screened 671 119 children (56.7% males) for significant refractive error and other eye ailments. Ocular problems were found in 20 321 (3.03%) children. The 3 localities with highest ocular pathology were Karary (26.2%), Ummbada (21.0%) and Jabal Awlia (15.7%). The overall prevalence of refractive error was 2.19%. Myopia was found in 10 064 (1.50%) children while 4661 (0.70%) were hyperopic. Other ocular problems included vernal keratoconjunctivitis, vitamin A deficiency, microbial conjunctivitis, strabismus and corneal opacity. Only 288 (0.04%) children were diagnosed with active trachoma: 86.5% of these were from Ummbada locality, on the periphery of the State, where transportation facilities are poor and poverty is widespread. Overall, 99% of the eye ailments identified are either treatable or preventable. To reduce these and to achieve the goals of Vision 2020, an effective and efficient school health programme is needed.
Troubles oculaires chez des écoliers dans l'État de Khartoum (Soudan)
RÉSUMÉ De décembre 2005 à juin 2007, un dépistage exhaustif dans l'ensemble des 1418 écoles primaires publiques de l'État de Khartoum (Soudan) a été mené afin d'évaluer les troubles oculaires des enfants âgés de 6 à 15 ans. Nous avons soumis 671 119 enfants (56,7 % de sexe masculin) à un dépistage des vices de réfraction et autres pathologies apparentées. Des troubles oculaires ont été dépistés chez 20 321 enfants (3,03 %). Les trois localités où ce type de pathologies étaient les plus fréquentes étaient Karary (26,2 %), Ummbada (21,0 %) et Jabal Awlia (15,7 %). La prévalence globale des vices de réfraction s’élevait à 2,19 %. Une myopie a été diagnostiquée chez 10 064 enfants (1,50 %) et une hypermétropie chez 4661 élèves (0,70 %). La kératoconjonctivite vernale, la carence en vitamine A, la conjonctivite microbienne, le strabisme et l'opacité cornéenne comptaient parmi les autres troubles oculaires. Seuls 288 enfants (0,04 %) ont reçu le diagnostic de trachome actif : 86,5 % d'entre eux étaient originaires de la localité d'Umbada, à la périphérie de l'État, où les transports sont médiocres et la pauvreté généralisée. Globalement, 99 % des maladies oculaires identifiées étaient soit traitables, soit évitables. Afin de réduire leur prévalence et de réaliser les objectifs de Vision 2020, il est nécessaire d'avoir un programme de santé scolaire qui soit efficace et bien organisé.
1Department of Ophthalmology; 4Department of Family and Community Medicine, College of Medicine, Dammam University, Al-Khobar, Saudi Arabia
2Makkah Eye Complex & Makkah Ophthalmic Technical College, Al-Basar International Foundation, Khartoum, Sudan. 3Al-Basar International Foundation, Al-Khobar, Saudi Arabia. 5Pakistan Institute of Community Ophthalmology, Khyber Medical University, Peshawar, Pakistan. 6Department of Ophthalmology, King Fahad Hospital of the University, Al-Khobar, Saudi Arabia (Correspondence to A.A. Rushood:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
Received: 26/06/11; accepted: 01/11/11
EMHJ, 2013, 19(3):282-288
Introduction
Blindness and visual impairment remain a major problem in the world today. There are an estimated 37 million people worldwide who suffer from blindness and 161 million who suffer from visual disability; around 80% of these are avoidable [1]. Cataract, which can be easily operated upon and cured, is responsible for more than half of the blindness in the world. Glaucoma, diabetic retinopathy, trachoma, uncorrected refractive error and childhood blindness make up the rest [1]. According to the World Health Organization (WHO), the number of blind children in the world is approximately 1.4 million, and three-quarters of these live in the poorest regions of Africa and Asia [2].
The available data suggest that there is wide regional variation in the major causes of blindness in children. In wealthy parts of the world lesions of the central nervous system predominate, while in poorer countries corneal scarring as a result of acquired diseases are the most important causes [3].
Children are given priority in the Vision 2020 initiative and WHO plans for fighting blindness [4]. In developed countries, screening for eye diseases in preschool and school-aged children is done routinely [5,6]. Vision screening to detect eye problems in school-aged children dates back at least a century [7], but as yet no such services are available in Sudan.
Sudan is one of the largest countries in Africa, but has poor socioeconomic status. Blindness remains a major public health problem, with around half a million people blind, mostly due to cataract, glaucoma, onchocerciasis and childhood blindness. The prevalence of blindness in Sudan is estimated to be 1.5% [8,9].
Currently there are no data available on pattern of eye problems in children in Sudan and owing to the absence of effective school health services the situation has become more serious. Causes of avoidable blindness among children need early detection and intervention.
This study focuses on assessing the burden of ocular disorders in schoolchildren in order to plan effectively for prevention and/or managing avoidable blindness among Sudanese children. We estimated the prevalence of ocular problems in schoolchildren aged 6–15 years, in Khartoum State, Sudan.
Methods
This study was conducted in all 1418 governmental basic schools in Khartoum State, Sudan. It started in December 2005 and was completed by the end of June 2007. This was a total coverage survey for these types of schools. In 2008, the population was estimated at 7.15 million, around 24% of the total population of Sudan [10]. Basic schools are present in all areas of the State.
A total of 671 119 schoolchildren aged 6–15 years were included in the survey.
Study procedure
The teams visited all governmental basic schools in Khartoum State according to a planned schedule. All children were screened. Multiple visits were paid to each site to ensure coverage of any absentees.
Visual acuity (V/A) of each eye was assessed using Snellen’s E chart at a distance of 6 m. The targeted age group (aged 6–15 years) allowed using the E-chart with ease. External ocular examination was done with torch and hand-held magnifier, while the fundus was examined with direct ophthalmoscope. Refraction was done to obtain maximum vision amongst children with visual acuity ≤ 6/12 and showing improvement with pin-hole.
Treatment was provided for common ocular conditions such as conjunctivitis, vernal catarrh etc. Children with V/A ≤ 6/12 were refracted and provided with corrective spectacles when needed. Children with xerophthalmia were provided with vitamin A capsules and health education regarding vitamin A deficiency disorders. Children needing surgical intervention were referred to tertiary eye care facilities in Makkah Eye Complex, Khartoum.
The check-list for the survey covering the data collected for each pupil was piloted on patients attending the paediatric ophthalmology clinics in the out-patient department of Makkah Eye Complex in Khartoum. This was carried out to ensure the feasibility and practicality of collecting such information, as well as to train the team members in form-filling, coding and data entry.
Field methodology
Although the initial plan was to recruit and train school teachers to perform the initial screening and visual acuity testing, this plan could not be continued due to lack of interest among the teachers. Seven field teams were formed for the purpose of screening. Each team consisted of 2 optometrists and 2 ophthalmic assistants provided from well-established, busy paediatric ophthalmology outpatient clinics at Makkah Eye Complex. A community ophthalmologist supervised the overall activities of the screening. Multiple visits were paid to each site to ensure coverage of any absentees. The survey was done in 2 rounds. First, the ophthalmic assistants screened the children by checking V/A and looking for any ocular disorders. In the second round the optometrists and the ophthalmic assistants refracted all with V/A ≤ 6/12. In both rounds, the V/A of each eye was assessed separately. External ocular examination was done with the help of a magnifying loupe (× 1.25) and a pin-light to distinguish red eye, discharging eyes, and white spot in the eye (corneal scar) as well as crossed-eyes. The fundus was examined with a direct ophthalmoscope. Refraction was done to obtain maximum vision. Spherical equivalents were calculated for each refractive finding. Myopia was defined as –0.50 based on the spherical equivalent readings, and hyperopia was defined as +1.50 based on the same.
Detailed ocular examination including fundoscopy with direct ophthalmoscope was performed on all children with best corrected V/A
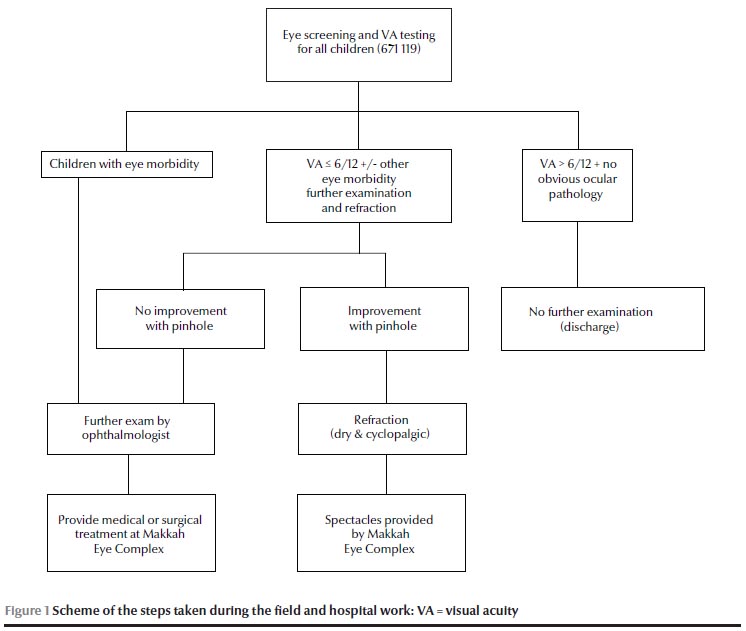
Forms (check-lists) were completed only for those with either an eye ailment or binocular vision ≤ 6/12. Figure 1 demonstrates the steps taken during the field and hospital work. Each examination took 5–10 minutes.
Data management and analysis
Completed data forms were reviewed in the field for accuracy and missing values. Data were double entered in the computer using SPSS for Windows, version 13.0. Verification and data cleaning were conducted at Makkah Eye Complex. Frequency and distribution tables were constructed as descriptive statistics. Results were cross-tabulated to examine the relationships between variables.
Statistical analysis was performed using the chi-squared test for association and Fisher’s exact test, as appropriate. P-values
Ethical approval
The study was approved by the ethical committees of Makkah Eye Complex, Khartoum State Ministry of Health and Khartoum State Ministry of Education. Informed consent for examination and cycloplegic refraction was obtained from parents via the teachers. Ophthalmic medicine, including vitamin A capsules and free glasses were provided to all children detected as having any eye problem or refractive error.
Results
A total of 671 119 schoolchildren (56.7% males) aged 6–15 years from 1418 governmental schools were screened. Initial screening indicated 30 693 pupils suspected of having some ocular ailment. Further evaluation of this group by senior staff excluded 10 372 children from the initial suspects. This left 20 321 (3.03%) children who had some ocular problem: 10 125(49.8%) of those were aged ≤ 10 years; 11 543 (56.8%) were boys.
The overall prevalence of refractive error (RE) was 2.19% (Table 1 ). This makes RE the most common cause for ocular morbidity among the schoolchildren (72.5%; 14 725 of 20 321): 8233 (55.9%) of these were boys (Table 2). We found 10 064 children had myopia and 4661 were hyperopic, giving a prevalence of 1.50% and 0.70% for myopia and hyperopia respectively. Of the 14 725 children with RE, 7028 (47.7%) were aged ≤ 10 years (Table 2). Hyperopia, but not myopia, was more associated with female sex (Table 2). Among females, there was no association between age and type of RE. Myopia was associated with older age amongst male children in our study.
Karary locality had the highest number of children with RE (5096; 34.6%) while Sharq el Nil has the lowest number (527; 3.6%) (Table 3 ).
Some ocular disorders showed a significant association with sex (Table 2): hyperopia, strabismus, trachoma and chalazia were more prevalent among girls (P = 0.001), and myopia, vernal keratoconjunctivitis and corneal opacities were more common among boys (P = 0.001). With the exception of cataract and nystagmus, all other ocular morbidities were statistically significantly associated with sex.
Cataract was found coexisting with other eye ailments and was dealt with separately in the data analysis. Visually disturbing cataract of any grading and any type (congenital, developmental or traumatic) was diagnosed in 261 (0.04%) children, 145 (55.6%) boys and 116 (44.4%) girls (Table 2). Of these, 137 (52.5%) were aged > 10 years. Almost 29% (75 out of 261) of these cases came from Karary locality (Table 3).
Of the other ocular problems diagnosed, with or without RE, the most commonly occurring were vernal keratoconjunctivitis (spring catarrh) 3429 (0.51%) followed by vitamin A deficiency 2397 (0.36%) (Table 2). The prevalence of trachoma, chalazion, ptosis and nystagmus were all below 0.05% (Table 2). Of the 288 pupils who were diagnosed as having active trachoma, 249 (86.5%) were from Ummbada locality (Table 3).
Cataract, strabismus, ptosis and vitamin A deficiency were more prevalent in Karary than in other localities (P = 0.001 for each) (Table 3). Trachoma, other corneal opacities (post-traumatic or post-infective), chalazia and microbial conjunctivitis significantly predominated in Ummbada locality. One third of the children with vernal keratoconjunctivitis (1145 out of 3429) were from Jabal Awlia locality.
Discussion
The prevalence of ocular morbidity detected amongst the schoolchildren in our study was 3.03%. This is lower than the prevalence in studies from Tibet (18.36%) [11], Nepal (11%) [12] and Ethiopia (62.6%) [13]. Males outnumbered females in having eye diseases: 56.3% of boys and 43.7% of girls had some ocular pathology. This is contradictory to the findings from some studies in Nigeria [14] and Pakistan [15].
Distribution of eye diseases varied from region to region. Most of the eye problems were reported amongst children from Karary and Ummbada. Most probably, the reason for this is that these 2 localities are situated in the periphery of Khartoum State and are far from the centre of Khartoum, away from contacts and eye care services. Transportation facilities are poor and poverty is widespread. It is important to note here that these locations are preferred places for many "temporary settlers" who are migrating from different areas of Sudan to Khartoum State. These regions are heavily populated and schools are very crowded (perhaps 100 or more in a class). These conditions facilitate contamination and infection between children. On the other hand, on the whole, Khartoum and Sharq el Nil localities had the lowest proportion of ocular morbidity among schoolchildren (with the exception of strabismus, nystagmus and cataract). These 2 localities are considered to be the richest areas in Khartoum State. Inhabitants are mostly high-ranking government employees and people of high socioeconomic status.
The prevalence of RE amongst the children was 2.19%. It is worth mentioning that the initial screening in a few cases was performed by trained teachers and ophthalmic technicians. It is likely this resulted in missing some children with RE, leading to an underestimation of the prevalence of this problem. More important, as cycloplegic refraction was only done on those children with obvious ocular morbidity, there is a high possibility that some pupils with RE, especially low hyperopes, were missed. The prevalence is lower than what was found in studies in Nepal (2.9%) [16], Malaysia (17.1%) [17], China (22.3%) [18] but more than in studies from South Africa (1.4%) [19] and Tanzania (1%) [20], though in Tanzania, the age group studied was slightly different from that in the current study, focusing on pupils aged 7–19 years.
Hyperopia in our study was quite low, even with a definition of +1.50 D or more. This is most probably because cycloplegic refraction was not done on everyone. Both myopia and hyperopia were more prevalent in pupils aged > 10 years. This is very important because amblyopia is considered by most authorities to be untreatable above this age [21], while it is manageable in those
Vernal keratoconjunctivitis was the second most common cause of ocular pathology (0.51%). This was close to what was found in schoolchildren in a study in southern Ethiopia (0.7%) [13] but much lower than in a study in South-Western Nigeria (7.4%) [23]. Most of the vernal keratoconjunctivitis cases are of the limbal form, well known in African people. This form is more severe, hence more associated with complications such as corneal vascularization and ectatic corneal changes like keratoconus [24].
Just under 0.4% or our sample had some ocular manifestation of vitamin A deficiency. It is clear that with the criteria followed in the diagnosis of this problem, a number of cases were missed and under-diagnosis of this morbidity was likely.
Microbial conjunctivitis and other corneal opacities were diagnosed in 0.22% and 0.20% of our sample respectively. Almost two-thirds of the corneal scars were found in boys. Similar findings have been reported in studies from Ethiopia and Nigeria [13,14,23].
Strabismus was the fifth most common cause of ocular morbidity in our sample of Sudanese schoolchildren. Overall prevalence was 0.22%. This is much lower than Oman (0.9%) [25] and the Islamic Republic of Iran (1.2%) [26].
Surprisingly, trachoma was not a major cause of ocular morbidity in our sample of schoolchildren from Khartoum State. Only 288 (0.04%) pupils were diagnosed with active trachoma. This is in contrast to reports from some regions of southern Sudan, where trachoma was found to be endemic and there was an unusually high prevalence of active trachoma and trachomatous trichiasis in children [27]. Early stages of the disease (F1 and F2) can be asymptomatic and may be overlooked in quick ocular examination. This leads to the suspicion that trachoma might be under-diagnosed in our study. An interesting finding is that 86.5% of the diagnosed cases of trachoma were found in Ummbada locality. This area is poor and has harsh environmental conditions. A modest prevalence of trachoma has also been found in studies in Tanzania [20], Ethiopia [13] and Nigeria [28,29].
A small proportion of children in our study (0.04%) had visually disturbing cataract. This is lower than in children from South Africa (0.6%) [19] and Tanzania (0.22%) [20]. Zeidan Z et al. studied the prevalence and causes of visual impairment and blindness in children under 16 years among internally displaced people in Khartoum State [30]. They found that the commonest anatomical sites of visual loss in the 40 blind and/or severely visually impaired children were corneal scarring (mostly related to vitamin A deficiency disorders) and lens opacity (cataract).
The strength of this study comes from the large number of children examined. This is also a maiden study on childhood ocular morbidity in Sudan, and it provides baseline data for strategies of planning and implementation of the Vision 2020 initiative.
One of the weaknesses of this study is that data was collected by optometrists and ophthalmic technicians and that possibly limited the ability to detect posterior segment disorders and hence miss some of the morbidity.
Conclusion
This study shows that 99% of the eye ailments we identified in the schoolchildren we studied are either treatable or preventable. This is a very high proportion of avoidable and/or treatable eye disease compared with other countries.
In the absence of an efficient school screening programme, the prevalence of eye diseases in schoolchildren may rise. Refractive error, vitamin A deficiency, corneal opacities and ocular alignment problems are on the high priority list of the WHO Vision 2020 Programme. They are also the commonest causes of ocular morbidities in Sudanese children.
Our findings also indicate that if a trachoma campaign is to be started, Ummbada locality should have priority since more than 85% of the trachoma cases identified were in that locality.
To achieve the goals of Vision 2020 in Sudan, there is a need to start an effective and efficient school health programme. This will enable eye-health workers to prevent and/or treat 99% of eye diseases in school-going children.
Acknowledgements
We would like to give special thanks to the Sudanese Red Crescent, and the Health and Education Ministries of Khartoum State. Our gratitude is extended to all the teachers, medical teams and doctors who made the task possible as well as the management of Makkah Eye Complex, Khartoum.
This study was financially and administratively supported by the Qatar Red Crescent and Al-Basar International Foundation.
References
- Resnikoff S et al. Global data on visual impairment in the year 2002. Bulletin of the world Health Organization, 2004, 82(11):844–851.
- Gilbert C, Foster A. Childhood blindness in the context of VISION 2020–the right to sight. Bulletin of the World Health Organization, 2001, 79:227–232.
- (No authors listed). New issues in childhood blindness. Community Eye Health, 2001, 14(40):53–56.
- Thylefors B. A global initiative for the elimination of avoidable blindness. American Journal of Ophthalmology, 1998, 125:90–93.
- Yang YF, Cole MD. Visual acuity testing in schools: what needs to be done. BMJ (Clinical Research Ed.), 1996, 313(7064):1053.
- Preslan MW, Novak A. Baltimore Vision Screening Project. Ophthalmology,1996, 103(1): 105–109.
- Appelboom TM. A history of vision screening. Journal of School Health, 1985, 55:138–141.
- Curable blindness: Sudan (data table). CurableBlindness (Web page) http://www.curableblindness.org/region/africa/sudan.html, accessed 5 February 2012.
- Babiker A, Elsheikh E, Elawad M. Causes of low vision in Sudan: a study among the attendees of blind centres in Khartoum. Sudan Journal of Ophthalmology. 2009, 1(1):13–19.
- Khartoum (state). Wikipedia, 2009 http://en.wikipedia.org/wiki/khartoum (state).
- Lu P et al. Prevalence of ocular disease in Tibetan primary school children. Canadian Journal of Ophthalmology, 2008, 43(1):95–99.
- Nepal BP et al. Ocular morbidity in schoolchildren in Kathmandu. British Journal of Ophthalmology, 2003, 87:531–534.
- Worku Y, Bayu S. Screening for ocular abnormalities and subnormal vision in school children of Butajira Town, southern Ethiopia. Ethiopian Journal of Health Development, 2002, 16(2):165–171.
- Ayotunde I et al. Pattern of eye diseases and visual impairment among students in south western Nigeria. International Ophthalmology, 2007, 27(5):287–292.
- Lakho K, Khalid B, Jadoon M. Ocular disorders among school going Pakistani children. Sudan Medical Monitor. 2009, 4(1):35–39.
- Pokharel GP et al. Refractive error study in children: results from Mechi Zone, Nepal. American Journal of Ophthalmology, 2000, 129(4):436–444.
- Goh PP et al. Refractive error and visual impairment in school-age children in Gobak District, Malaysia. Ophthalmology, 2005, 112:678–685.
- He M et al. Refractive error and visual impairment in urban children in southern China. Investigative Ophthalmology & Visual Science, 2004, 45(3):793–799.
- Naidoo KS et al. Refractive error and visual impairment in African children in South Africa. Investigative Ophthalmology & Visual Science, 2003, 44:3764–3770.
- Wedner SH et al. Prevalence of eye diseases in primary school children in a rural area of Tanzania. British Journal of Ophthalmology, 2000, 84:1291–1297.
- Results-an evaluation of treatment of amblyopia in children 7 < 18 years old (ATS3). Bethesda, Maryland, National Institutes of Health, National Eye Institute, 2005 (http://www.nei.nih.gov/ats3/background.asp, accessed 5 February 20130.
- Elimination of avoidable visual disability due to refractive errors. Geneva, World Health Organization, 2000 (Report No.: WHO/PBL/00.79).
- Ayotunde I et al. Prevalence and causes of eye diseases amongst students in south-western Nigeria. Annals of African Medicine, 2006, 5(4):197–203.
- Dahan E, Appel R. Vernal keratoconjunctivitis in the black child and its response to therapy. British Journal of Ophthalmology, 1983, 67(10):688–692.
- Lithander J. Prevalence of amblyopia with anisometropia or strabismus among schoolchildren in the Sultanate of Oman. Acta Ophthalmologica Scandinavica, 1998, 76(6):658–662.
- Fotouhi A et al. The prevalence of refractive errors among schoolchildren in Dezful, Iran. British Journal of Ophthalmology, 2007, 91(3):287–292.
- Ngondi J et al. The epidemiology of trachoma in Eastern Equatoria and Upper Nile States, southern Sudan. Bulletin of the World Health Organization 2005, 83:904–912.
- Mpyet C, Ogoshi C, Goyo M. Prevalence of trachoma in Yobe State, north-eastern Nigeria. Ophthalmic Epidemiology, 2008, 15(5):303–307.
- Obikili AG et al. Prevalence of trachoma among school children in Plateau State, Nigeria. Revue internationale du Trachome et de Pathologie oculaire tropicale et subtropicale et de Santé publique, 1990, 67:181–192.
- Zeidan Z et al. Prevalence and causes of childhood blindness in camps for displaced persons in Khartoum: results of a household survey. Eastern Mediterranean Health Journal, 2007, 13(3):580–585.




 Volume 31, number 5 May 2025
Volume 31, number 5 May 2025 WHO Bulletin
WHO Bulletin Pan American Journal of Public Health
Pan American Journal of Public Health The WHO South-East Asia Journal of Public Health (WHO SEAJPH)
The WHO South-East Asia Journal of Public Health (WHO SEAJPH)