Close the gap in cancer care to CureAll children with cancer
For this year’s International Childhood Cancer Day, the World Health Organization and partners unite to make the world aware, to close the gap in cancer care – which is the focus of this year’s Day.
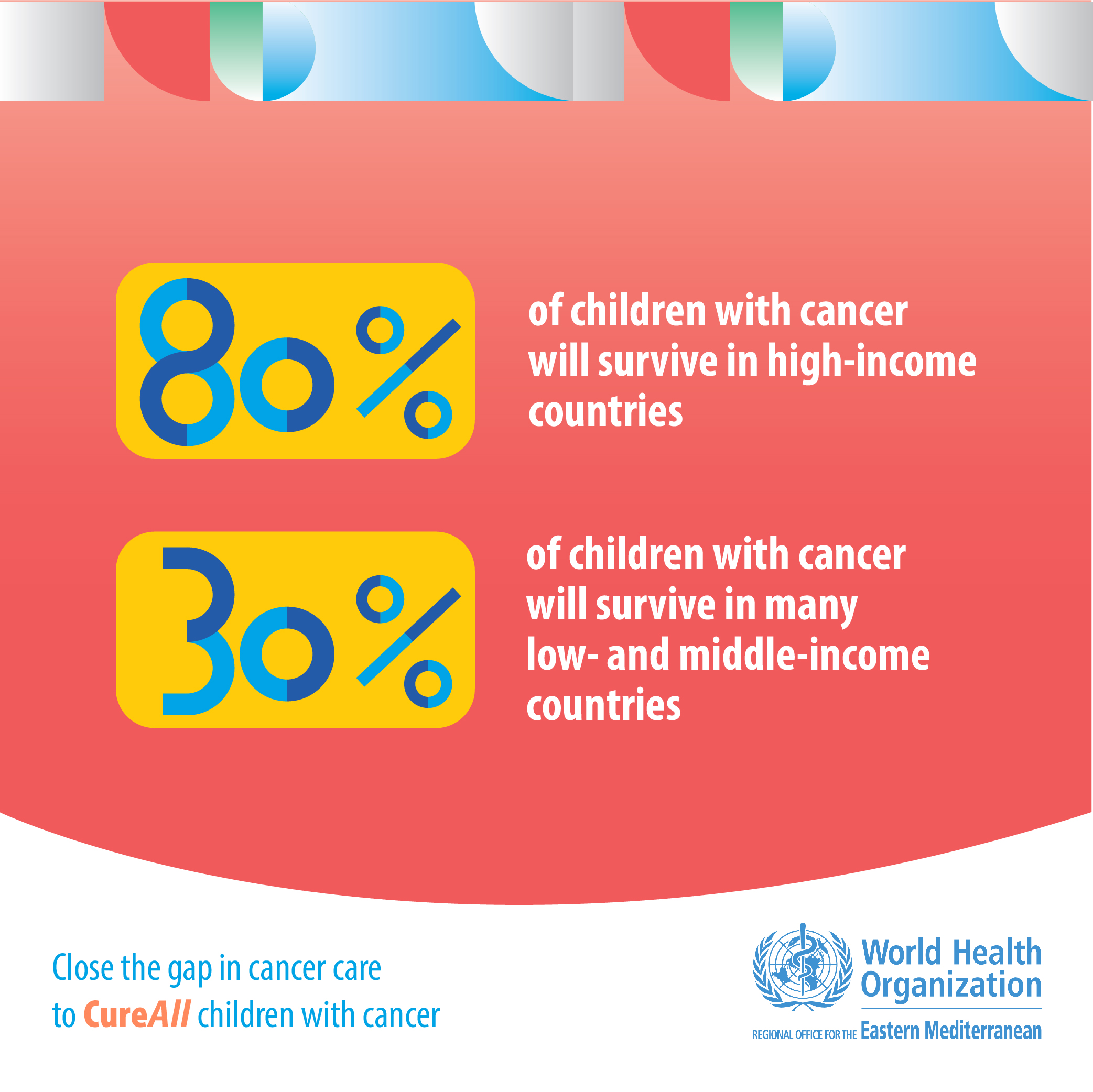
Every day, more than 1000 children are diagnosed with cancer. This news sets all concerned on a demanding and life-changing journey. For children in high-income countries, more than 80% survive. But, for many children living in low- or middle-income countries in the Eastern Mediterranean Region and beyond, the reality is death and immense family strain.
We can improve outcomes for children with cancer across our Region and beyond thus contributing to the WHO Global Initiative for Childhood Cancer, where we aim to reach at least a 60% survival rate for children with cancer by 2030. Join us to make the world aware, to close the gap in cancer care, and CureAll children with cancer. Work with us so we can give all children with cancer in our Region the best chance to survive, to live full and abundant lives and to live and die without suffering.
WHO Global Initiative for Childhood Cancer
In September 2018, WHO announced a new effort – the WHO Global Initiative for Childhood Cancer – with the aim of reaching at least a 60% survival rate for children with cancer by 2030, thereby saving an additional one million lives. This new target represents a doubling of the global cure rate for children with cancer.
The aims of the Initiative are two-fold: to increase prioritization of childhood cancer through awareness raising at global and national levels and to expand the capacity of countries to deliver best practice in childhood cancer care.
WHO Global Initiative for Childhood Cancer
IARC's Global Cancer Observatory (GCO)
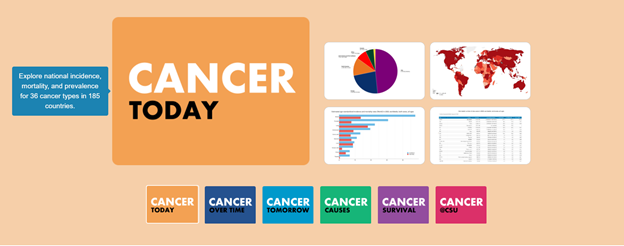
The Global Cancer Observatory (GCO) is an interactive web-based platform presenting global cancer statistics to inform cancer control and cancer research. The platform focuses on the visualization of cancer indicators using data from IARC’s (International Agency for Research on Cancer) Cancer Surveillance Branch, including GLOBOCAN, Cancer Incidence in Five Continents (CI5), International Incidence of Childhood Cancer (IICC), and several cancer survival benchmarking projects (SurvCan and SURVMARK).
The GCO is under continual development and the team will continually seek novel and informative ways of presenting global cancer data that link to IARC’s research activities.
IARC's Global Cancer Observatory
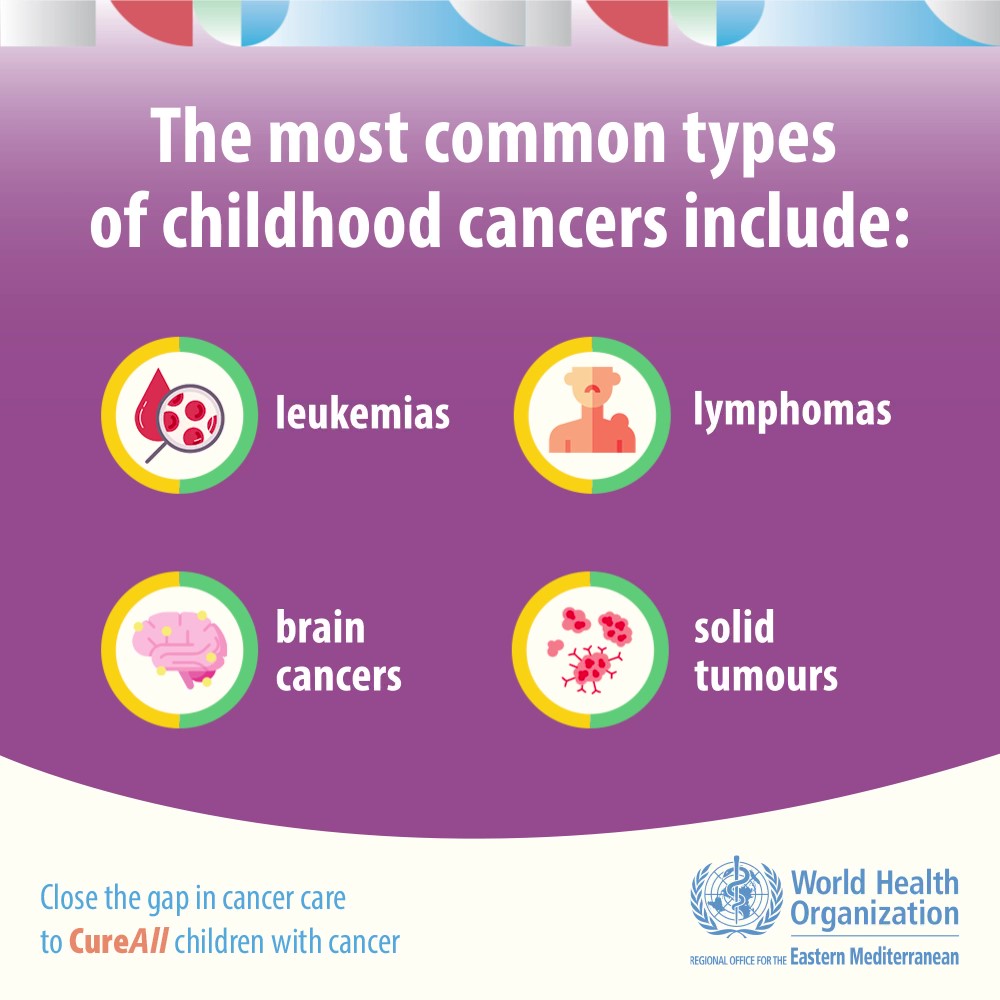
Childhood cancer
Cancer is a leading cause of death for children and adolescents. The likelihood of surviving a diagnosis of childhood cancer depends on the country in which the child lives: in high-income countries, more than 80% of children with cancer are cured, but in many low- and middle-income countries, less than 30% are cured.
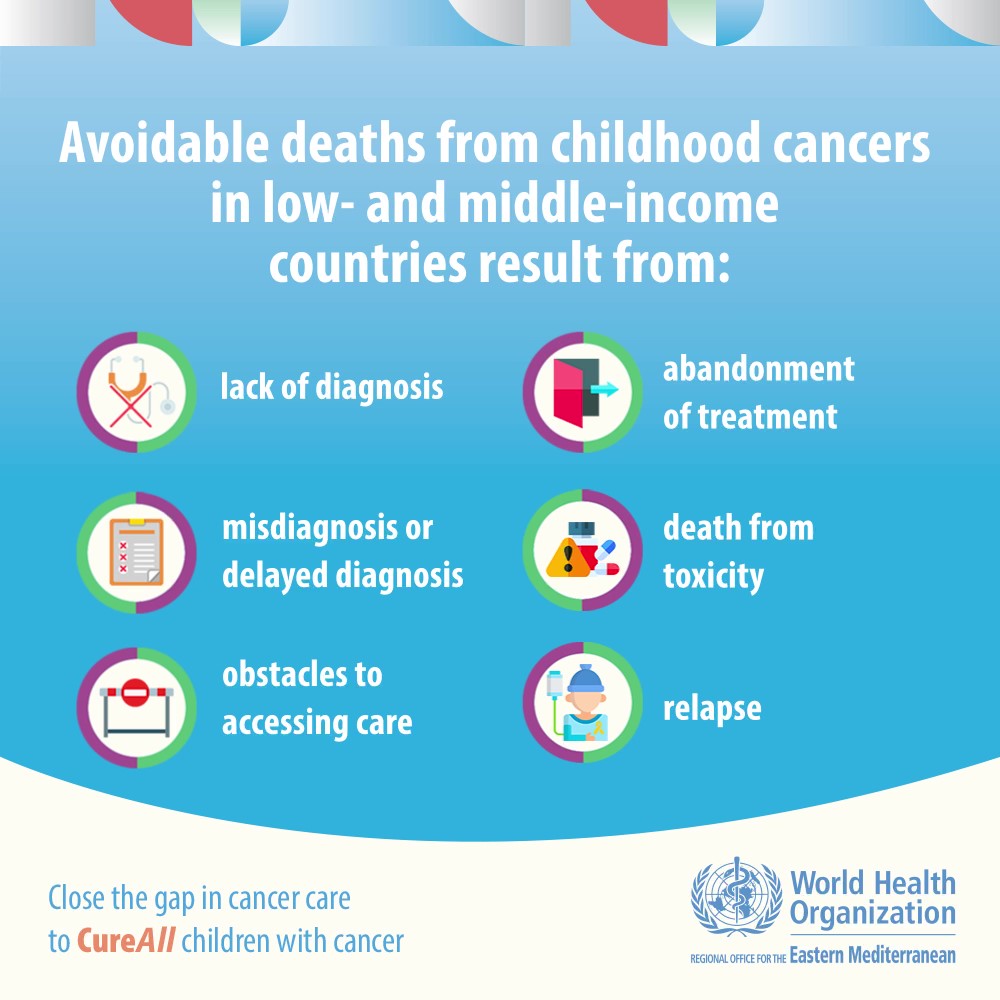
The reasons for lower survival rates in low- and middle-income countries include:
delay in diagnosis
an inability to obtain an accurate diagnosis
inaccessible therapy
abandonment of treatment
death from toxicity (side effects)
avoidable relapse.
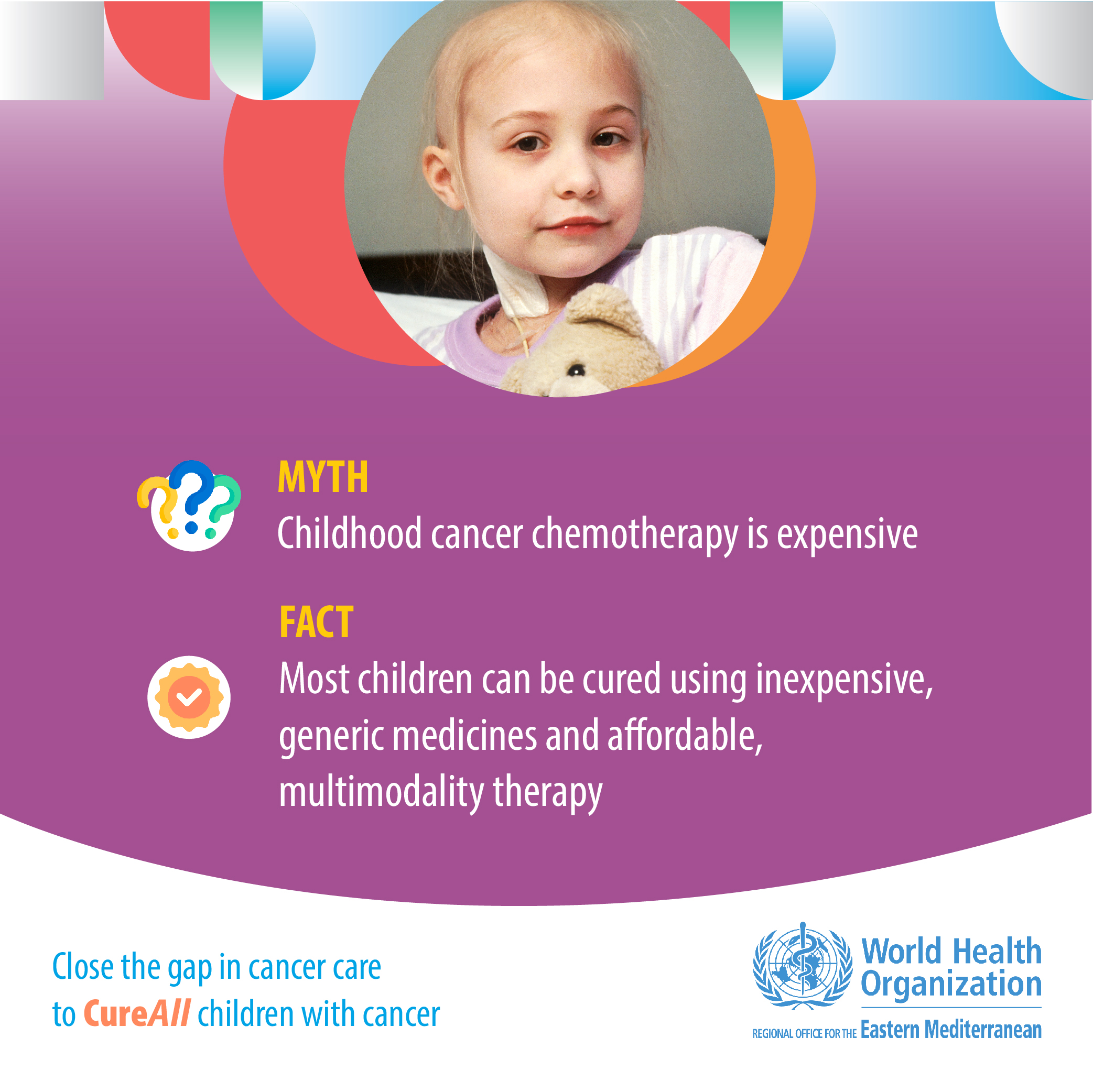
Improving access to childhood cancer care, including to essential medicines and technologies, is highly cost effective, feasible and can improve survival in all settings.
What causes cancer in children?
Cancer occurs in people of all ages and can affect any part of the body. It begins with genetic change in single cells, that then grow into a mass (or tumour), that invades other parts of the body and causes harm and death if left untreated. Unlike cancer in adults, the vast majority of childhood cancers do not have a known cause. Many studies have sought to identify the causes of childhood cancer, but very few cancers in children are caused by environmental or lifestyle factors. Cancer prevention efforts in children should focus on behaviours that will prevent the child from developing preventable cancer as an adult.
Some chronic infections such as HIV, Epstein-Barr virus and malaria, are risk factors for childhood cancer. They are particularly relevant in low- and middle-income countries. Other infections can increase a child’s risk of developing cancer as an adult, so it is important to be vaccinated (against hepatitis B to help prevent liver cancer and against human papillomavirus to help prevent cervical cancer) and to pursue other methods such as early detection and treatment of chronic infections that can lead to cancer.
Current data suggest that approximately 10% of all children with cancer have a predisposition because of genetic factors. Further research is needed to identify factors impacting cancer development in children.
How can we improve outcomes of childhood cancer?
Because it is generally not possible to prevent cancer in children, the most effective strategy to reduce the burden of cancer in children and improve outcomes is to focus on a prompt, correct diagnosis followed by effective, evidence-based therapy with tailored supportive care.
Early diagnosis
When identified early, cancer is more likely to respond to effective treatment and result in a greater probability of survival, less suffering, and often less expensive and less intensive treatment. Significant improvements can be made in the lives of children with cancer by detecting cancer early and avoiding delays in care. A correct diagnosis is essential to treat children with cancer because each cancer requires a specific treatment regimen that may include surgery, radiotherapy and chemotherapy.
Early diagnosis consists of three components:
awareness of symptoms by families and primary care providers;
accurate and timely clinical evaluation, diagnosis and staging (determining the extent to which a cancer has spread); and
access to prompt treatment.
Early diagnosis is relevant in all settings and improves survival for many cancers. Programmes to promote early and correct diagnosis have been successfully implemented in countries of all income levels, often through the collaborative efforts of governments, civil society and nongovernmental organizations, with vital roles played by parent groups. Childhood cancer is associated with a range of warning symptoms such as fever, severe and persistent headaches, bone pain and weight loss that can be detected by families and by trained primary health care providers.
Screening is generally not helpful for childhood cancers. In some select cases, it can be considered in high risk populations. For example, some eye cancers in children can be caused by a mutation that is inherited, so if that mutation or disease is identified in the family of a child with retinoblastoma, genetic counselling can be offered and siblings monitored with regular eye examinations early in life. Genetic causes of childhood cancers are relevant in only a small proportion of children with cancer. There is no high quality evidence to support population-based screening programmes in children.
Treatment
A correct diagnosis is essential to prescribe appropriate therapy for the type and extent of the disease. Standard therapies include chemotherapy, surgery and/or radiotherapy. Children also need special attention to their continued physical and cognitive growth and nutritional status, which requires a dedicated, multi-disciplinary team. Access to effective diagnosis, essential medicines, pathology, blood products, radiation therapy, technology and psychosocial and supportive care are variable and inequitable around the world.
However, cure is possible for more than 80% of children with cancer when childhood cancer services are accessible. Pharmacological treatment, for example, includes inexpensive generic medications included on the WHO List of Essential Medicines for Children. Children who complete treatment require ongoing care to monitor for cancer recurrence and to manage any possible long-term impact of treatment.
Palliative care
Palliative care relieves symptoms caused by cancer and improves the quality of life of patients and their families. Not all children with cancer can be cured, but relief of suffering is possible for everyone. Paediatric palliative care is considered a core component of comprehensive care, starting when the illness is diagnosed and continuing throughout treatment and care, regardless of whether or not a child receives treatment with curative intent.
Palliative care programmes can be delivered through community and home-based care, providing pain relief and psychosocial support to patients and their families. Adequate access to oral morphine and other pain medicines should be provided for the treatment of moderate to severe cancer pain, which affects more than 80% of cancer patients in the terminal phase.