Houssain Abouzaid1
1WHO Representative, Lebanon; Former Coordinator, Healthy Environments Programmes, World Health Organization Regional Office for the Eastern Mediterranean, Cairo, Egypt (Correspondence to Houssain Abouzaid:
EMHJ, 2008, 14(Supplement): S132-S142
Introduction
Environmental effects on health are associated with several factors: absent or inadequate environmental health services, such as water supply, sanitation, solid and hazardous waste management and shelter; environmental degradation, such as pollution of air, water and soil, and food contamination; global environmental problems, such as reduction of biodiversity and degradation of ecosystems through deforestation, global warming, ozone layer depletion and contamination by persistent organic chemicals; and industrial accidents. The indirect health effects of environmental conditions and changes, such as the implications of a limited episode of food contamination on a country’s food exports, may be more significant than their direct health effects.
A significant part of the population of the Eastern Mediterranean Region (EMR) suffers from an insecure or low level of income. In 2006 the average GDP per capita in the Region was estimated at only US$ 2030. Moreover, out of 530 million inhabitants, 226 million lived in countries with a GDP per capita less than US$ 1000 [1]. This has far-reaching effects on environmental degradation and impairment of health; poor people are not protected against disease and lack the resources and motivation to protect the environment. The Region is also experiencing rapid urbanization, which leads in many instances to haphazard development. Urban facilities and services are often unplanned and overwhelmed by population growth and overcrowding, resulting in various health hazards. The high regional population growth rate (2.1%) often outpaces the capacity to provide environmental health services, amplifying adverse effects of environmental pollution.
Environmental factors linked to health
Water access and quality
Water demand in the Region is growing fast and water availability is decreasing to crisis levels. Nevertheless wastage of water is widespread, and the water resources available are threatened by salt intrusion and other kinds of pollution; indeed the whole issue of water shortage has not been addressed in depth. Mitigation measures are rarely defined in an integrated manner and water demand management is practised in only a few countries. The reuse of wastewater in agriculture, and for the development of green belts and recreational areas, is practised to varying degrees to alleviate water shortages. However, in many cases, raw or inadequately treated sewage is used in an unregulated manner. Such practices can affect the health of agricultural workers and lead to contaminated foodstuffs, which expose consumers to health risks [2].
Polluted water can be a source of deadly disease: globally, 1.5 million people, most of them children, die each year of diarrhoeal disease linked to inadequate water supply and hygiene and 860 000 deaths per year are caused by malnutrition induced by unsafe water, inadequate sanitation and insufficient hygiene in children under 5 years [3], and in Bangladesh over 35 million people are at risk from drinking-water supplies with high levels of arsenic [4].
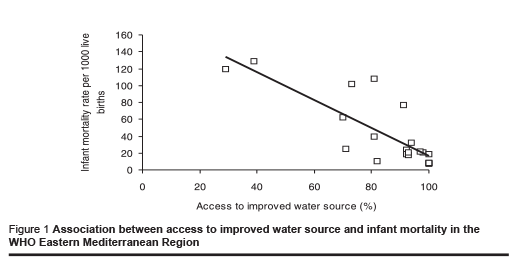
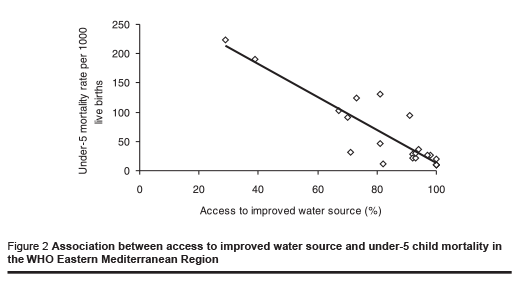
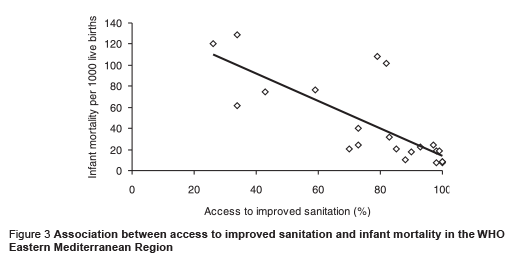
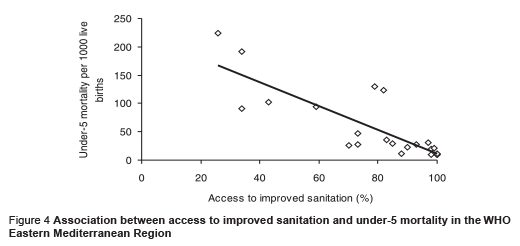
In the Region, 78 million people had no access to improved water sources in 2004 and 177 million had no access to sanitation facilities [5]. Figures 1, 2, 3 and 4 based on data in Table 1, show the association between level of access to water supply and sanitation and child mortality. In addition, water supply is intermittent in many countries and may compromise the integrity of the water distribution network and the quality of the water distributed.
Desalination is one strategy that has been used in the EMR to address water scarcity, mainly in the Gulf Cooperation Council countries where drinking-water is a blend of desalinated water and groundwater. The need to assess the technical problems associated with water quality at the different stages of the desalination processes and the distribution and consumption of water with very low mineral content was addressed by the World Health Organization (WHO) Regional Office for the Eastern Mediterranean (EMRO), who, on behalf of WHO as a whole, led the preparation of the WHO Guidance Document on desalination for safe water supply [6]. Assessments of the vulnerability of desalination facilities to accidental pollution and other emergencies are also needed.
Safe water and adequate sanitation are basic human rights and, together with hygiene education, are fundamental to protecting health, increasing the sense of well-being, and improving, economic and social productivity. EMRO has a 3-year plan to gather scientific data which will allow it to undertake work to determine the minimum water requirement for health, a critical issue in a region where water scarcity is the rule and drought an inescapable fact.
Air quality
Anthropogenic sources of air pollution have existed at least since humans discovered fire; investigations of ice in Greenland show that 2500 years ago lead and copper concentrations in the air exceeded natural levels due to extensive smelting of ores in the open air [7]. Air pollution has worsened rapidly with industrialization and the resultant widespread use of fossil energy sources, increased manufacturing and “chemicalization” of daily life.
Outdoor air quality is a matter of concern in many cities, particularly the megacities, but indoor air pollution is an even greater source of concern. Globally, indoor air pollution from solid fuel use is responsible for 1.6 million deaths due to pneumonia, chronic respiratory disease and lung cancer, with the overall disease burden exceeding the burden from outdoor air pollution fivefold [8]. High priority needs to be given to improving indoor air quality in both rural and urban areas. This should include strong action to prevent passive inhalation of tobacco smoke.
Solid waste disposal
In many countries of the Region, particularly in the secondary cities, there are serious shortcomings in the collection, transportation and disposal of solid waste. Uncollected solid wastes dumped near roads are common features in countries with large populations and high population densities. In some areas, housing may be situated in the midst of dumping sites. The indiscriminate burning of solid waste is also a major problem in certain countries; for example, it contributes to the well publicised autumnal black smoke events over Cairo. Scavengers in the solid waste disposal sites are at high health risk. Disposal of health care wastes mixed with municipal solid waste has been reported in many areas. In recent years, however, health care waste management has started to receive the necessary attention.
Climate change
The Fourth Assessment Report of the Intergovernmental Panel on Climate Change established that climate change is unequivocal and is caused by anthropogenic activities [9]. WHO has recognized the importance of climate change and its potential impact on health security for many years [10,11]. Indeed, climate change will adversely and profoundly affect the fundamental determinants of health – water, air and food – and is projected to decrease the availability of fresh water in the Region, with consequences for public health protection and food production.
The public health consequences of climate change include extreme weatherrelated mortality, affecting the elderly, the chronically sick and the poor; an increase in water-borne and food-borne diseases, and in acute respiratory infections and allergies due to dust storms; an increase in the geographic range and incidence of vector-borne diseases, such as malaria, leishmaniasis and schistosomiasis; and the emergence of diseases not seen much before in the Region, such as dengue fever. Forced migration and malnutrition are also likely to result, with health consequences of their own.
The public health action that is required includes preventative action aimed at moderating the impact of climate change on the key determinants of health (water, air and food) and measures to assess and manage the additional burden of disease that will be brought about.
Ionizing radiation and electromagnetic fields
The exposure of human beings to ionizing radiation from cosmic rays and radioactive nuclides in the earth’s crust is an inescapable feature of life. The application of ionizing radiation in medicine has become widely established for diagnosis and therapy, bringing overwhelming benefits to patients with proper use and represents the largest man-made source of radiation exposure for the global population. However, prolonged exposure to even low levels of ionizing radiation is associated with increased ill health, hence the importance of raising awareness of health workers and the population at large to this risk.
Concern has been expressed about the potential health risks associated with electromagnetic fields since the 1970s; suspected effects range from change in behaviour, childhood leukaemia and other forms of cancer, to Parkinson and Alzheimer diseases. Unlike ionizing radiation, which has enough energy to break chemical bonds (and thus can damage living cells), low frequency electromagnetic radiation (0–300 GHz) has insufficient energy to ionize atoms or fragments of molecules, but may interact with a biological system in a number of other ways, such as by inducing small changes of voltage and electrical current within the human body. Numerous studies have been published on the health effects of electromagnetic fields, and expert groups and panels have been established to review and evaluate the available data. So far, such efforts have not provided firm evidence to prove or disprove a causal association between exposure to electromagnetic fields and outcomes of public health significance.
Natural and man-made emergencies The Region is particularly affected by natural and man-made emergencies which degrade environmental conditions in two ways: through catastrophic events that markedly affect the environment, such as floods, drought, earthquakes, fire and industrial accidents; and through disruption of essential environmental health services, such as water supply and sanitation, solid waste and air quality management, which are often already strained [12].
The disruption of water and power supplies was widely witnessed during the invasion of the Palestinian territories in 2002. In Iraq, wastewater collection and treatment facilities throughout the country were nonfunctional after the Gulf Wars due to partial destruction of pumping and treatment facilities, lack of spare parts and intermittent lack of electricity.
Health effects of air pollution are normally characterized by long-term build up; in air pollution emergencies, however, such as in Bhopal, India in 1977, the effects are immediate and often lethal. In 1991, fires in hundreds of Kuwaiti oil wells caused dramatic, visible effects on air quality at the subregional level [13].
Industrial accidents and transport accidents involving hazardous materials are increasing worldwide. The impact on the affected communities is enormous and the medical, psychological and economic burden is heavy. Death and injury do not reflect the full health impact of these disasters, as the indirect effects, such as population displacement, economic losses, stress and social upheaval in the community, may be of even greater magnitude [12].
Though rare, radiation accidents have many medical, administrative, legal, social and psychological implications. The most serious nuclear accident occurred in 1986 in Chernobyl nuclear power station, releasing large amounts of radioactive material over vast areas of Belarus, Ukraine and the Russian Federation; even countries far from nuclear power stations need effective radiation protection programmes. Particular concerns were expressed in the Region in relation to the use of depleted uranium in Iraq and to nuclear powered ships cruising in the Gulf area. The possible use of depleted uranium during the 2006 war in Lebanon was the subject of intense debate, even after a joint International Atomic Energy Agency, United Nations Environment Programme and WHO joint fact-finding mission had concluded in February 2007 that there was no evidence of the use of depleted uranium in the conflict.
Emergencies are also often the occasion for spreading damaging rumours as the one regarding chemical and radiological contamination of seafood along the Somali coast in the aftermath of the 2006 Asian tsunami.
Other factors
Many other important sources of environmental health hazards are known to exist in the Region, such as noise pollution, soil contamination, and occupational hazards; in fact the Region is subject to the superposition of traditional, modern and emerging environmental health problems.
Health burden of environmental conditions
It is striking to note how the estimations made in 1948 regarding the health effects of environmental conditions (Box 1) are consistent with the recent WHO estimates, that globally 24% of the disease burden and 23% of all deaths are attributable to environmental factors. Among children 0–14 years of age, the proportion of deaths attributed to the environment was as high as 36% [14]. For the Region, it has been estimated that this proportion varies between 13% in countries where coverage with essential environmental health services is high and an alarming 30% in countries where access to such services is still problematic (Table 2). Table 2 also shows clearly the importance of indoor air pollution and water supply and sanitation in relation to health protection.
It should be noted that environmental health is not only important for health protection and promotion but also for health equity (Box 2). Indeed, environmental health is a pillar of health security.
Addressing the issue of health and the environment
Many national strategies and plans of action related to health and environment have been prepared and implemented throughout the Region but despite some progress in reducing mortality attributable to environmental causes in certain countries, sustained and amplified efforts are needed. The reasons why strategies and actions have not worked effectively relate primarily to weak institutional systems, unadapted and unenforced legislation, insufficient access to and use of health and environment information for decision-making, insufficient manpower both in number and training, and lack of leadership of the health sector in pushing for health and environmental action by other sectors and avoiding conflicting sectoral strategies in matters of health and environment. On the other hand, facilitating factors are often missing; the most important of these is political commitment, but include also linkage with the basic development needs approach, environmental health impact assessment and use of economic instruments.
WHO’s approach
The WHO Eleventh General Programme of Work 2006–2015 [15] has analysed current health challenges and concluded that health is increasingly seen as a key aspect of human security and occupies a prominent place in debates on priorities for development. Over the past 20 years there have been major gains in life expectancy overall, but there are widening gaps in health status. The importance of economic, social, and environmental determinants of health has grown. Demographic and epidemiological transitions now combine with nutritional and behavioural transitions, influenced by globalization and urbanization, to create unfavourable new trends.
To face health challenges in an efficient manner, WHO moved into a 6-year mid-term strategic plan, within which 13 organization-wide strategic objectives have been defined which are to be achieved by the Organization in the 6-year term. This should anchor the Organization in resultsbased management.
Strategic objective 8, which reads, “To promote a healthier environment, intensify primary prevention and influence public policies in all sectors so as to address the root causes of environmental threats to health”, is entirely relevant to health and environment; however other strategic objectives are equally relevant, namely Strategic objective 5 in relation to environmental health aspects of emergencies, Strategic objective 7 for the promotion of healthy settings approaches and Strategic objective 9 in regard to food safety.
An area where WHO/EMRO is looking to lead the way is in social responsibility. The regional Strategic objective 8 plans to demonstrate during the coming 6 years the feasibility that WHO only contract with corporations that respect at least occupational health and environmental legislation.
Given the emphasis WHO is placing on the determinants of health, prominent among which are environmental factors, it will be in good position in the coming few years to support its Member States in assessing, correcting and preventing health risks related to environmental factors and hence in achieving the health-related Millennium Development Goals [16].
There are however certain important prerequisites if we are to succeed in tackling the effects of environmental conditions and changes on health: individuals and communities need to become the guardians of their health and environment; shared agendas and plans of action need to be formulated around the core functions of public health and environmental management; and alliances need to be established between health and environment sectors to develop joint activities and programmes that would be beneficial for both sectors.
References
- Demographic, social and health indicators for countries of the Eastern Mediterranean, 2007. Cairo, WHO Regional Office for the Eastern Mediterranean, 2007 (http://www.emro.who.int/dsaf/dsa783. pdf, accessed 3 August 2008).
- Al Salem SS, Abouzaid H. Wastewater reuse for agriculture: regional health perspective. Eastern Mediterranean health journal, 2006, 12(3&4):446–58.
- Prüss-Üstün A et al. Safer water, better health – Costs, benefits and sustainability of interventions to protect and promote health. Geneva, World health Organization, 2008.
- World Water Day 2001. Water-related disease fact sheets (http://www.emro.who. int/wwd/, accessed 31 July 2008).
- WHO and UNICEF Joint Monitoring Programme for Water Supply and Sanitation. Water for life: making it happen. Geneva, World Health Organization, 2005.
- Desalination for safe water supply. Guidance for the health and environment aspects applicable to desalination. Geneva, World Health Organization, Public Health and Environment, 2007 (http://www.who. int/water_sanitation_health/gdwqrevision/ desalination.pdf, accessed 12 August 2008).
- Nriagu JO. A history of global metal pollution. Science, 1996, 272:223–4.
- Climate change 2007: The physical science basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, Cambridge University Press, 2007.
- Global burden of disease due to indoor air pollution. WHO indoor pollution website (http://www.who.int/indoorair/health_impacts/burden_global/en/index.html, accessed 3 August 2008).
- McMichael AJ et al., eds. Climate change and human health. An assessment prepared by a Task Group on behalf of the World Health Organization, World Meteorological Organization and United Nations Environmental Programme. Geneva, World Health Organization, 1996.
- World Health Organization. Protecting health from climate change – World Health Day 2008. (http://www.who.int/ world-health-day/toolkit/report_web.pdf, accessed 3 August 2008).
- Health effects of environmental conditions. Technical discussion presented at the Forty-ninth Session of the WHO Regional Committee for the Eastern Mediterranean, 30 September–3 October 2002 (EM/RC49/Tech.Disc.2).
- Regional report of the state of the marine environment. Kuwait, Regional Organization for the Protection of the Marine Environment, 1999.
- Prüss-Üstün A, Corvalán C. Preventing disease through healthy environments: towards an estimate of the environmental burden of disease. Geneva, World Health Organization, 2006.
- Engaging for health. Eleventh General Programme of Work 2006-2015. A global health agenda. Geneva, World Health Organization, 2006.
- UN Millennium Development Goals (http:// www.un.org/millenniumgoals/, accessed 4 August 2008).








