A.K. Sandhu1 and F.E. Mustafa2
وفيات الأمهات في البحرين بين عامَيْ 1987 – 2004: تدقيق في الأسباب التي يمكن تفاديها
ساندو أمرجيت كور، فكرية إبراهيم مصطفى
الخلاصـة: يستهدف هذا التقرير التعرف على معدل وفيات الأمهات في البحرين في ما بين عامَيْ 1987 – 2004 وعلى عوامل وفيات الأمهات التي يمكن توقِّيها، وعلى إصدار توصيات خاصة بالأمومة المأمونة. وقد وجدت الباحثتان أن عدد وفيات الأمهات 60 وفاة من بين 232 243 ولادة، أي بمعدل 24.7 وفاة لكل 000 100 ولادة. ومن أهم أسباب الوفاة مرض الخلايا المنجلية (25.0%)، وارتفاع ضغط الدم (18.3%)، والانصمام (13.3%)، والنزوف (13.3%)، وأمراض القلب (11.7%)، والعدوى (8.3%)، وأسباب أخرى (10.0%). ولدى التدقيق في الرعاية، وجد أن 17 وفاة من بين الوفيات الستين يمكن الحكم عليها بأنها كان يمكن تلافيها، وأن نصف هذه الوفيات ناجمة عن نقص في أسرَّة الرعاية المركَّزة. وتوصي الباحثتان بإجراء استقصاء متكتِّم حول وفيات الأمهات على المستوى الوطني كل 3 أو 5 سنوات.
ABSTRACT: The aim of this report was to establish the national maternal mortality rate in Bahrain over the period 1987–2004, to identify preventable factors in maternal deaths and to make recommendations for safe motherhood. There were 60 maternal deaths out of 243 232 deliveries giving an average maternal mortality rate of 24.7 per 100 000 total births. The main causes of death were sickle-cell disease (25.0%), hypertension (18.3%), embolism (13.3%), haemorrhage (13.3%), heart disease (11.7%), infection (8.3%) and other (10.0%). In an audit of care, 17 (28.3%) out of 60 deaths were judged to be avoidable, nearly half of which were due to a shortage of intensive care beds. We recommend that a confidential enquiry of maternal deaths be conducted at the national level every 3 to 5 years.
Mortalité maternelle à Bahreïn entre 1987 et 2004 : examen des causes de décès évitable
RÉSUMÉ: L’objectif de ce rapport était d’établir le taux national de mortalité maternelle à Bahreïn sur la période comprise entre 1987 et 2004, afin de recenser les facteurs de décès maternel évitables et de formuler des recommandations pour une maternité sans risque. On a dénombré 60 décès maternels sur 243 232 accouchements, soit un taux moyen de mortalité maternelle de 24,7 pour 100 000 naissances au total. Les causes de décès étaient les suivantes : drépanocytose (25,0 %), hypertension (18,3 %), embolie (13,3 %), hémorragie (13,3 %), cardiopathie (11,7 %), infection (8,3 %) et autres causes (10,0 %). Lors d’un audit des soins, 17 (28,3 %) des 60 décès ont été jugés évitables, près d’un sur deux étant du à un manque de lits de soins intensifs. Nous recommandons la réalisation d’une enquête confidentielle sur les décès maternels à l’échelle nationale tous les 3 à 5 ans.
1Department of Obstetrics and Gynaecology, Salmaniya Medical Centre, Ministry of Health, Bahrain (Correspondence to A.K. Sandhu:
2College of Medicine and Medical Sciences, Arabian Gulf University, Manama, Bahrain.
Received: 20/12/05; accepted: 23/02/06
EMHJ, 2008, 14(3):720-730
Introduction
Each case of maternal death in this report represents an individual tragedy, as pregnancy is not a disease and as pregnancy-related mortality is almost always preventable. Yet more than half a million women die each year due to pregnancy-related complications and 99% of these are from the developing world [1]. For example, in northern England there are 2–9 maternal deaths for every 100 000 births, whereas in Africa there is 1 maternal death for every 1000 births [2].
The overall maternal mortality rate in Bahrain has dropped from 42.3 per 100 000 total births in the period 1977–1981 to 24.7 per 100 000 in the period 1987–2004 [3]. While some maternal deaths occurring in this country may not be included in the statistics, their number is negligible as the population is only 707 160, with 62.0% Bahraini, 38.0% non-Bahraini and the crude birth rate is 21.1 per 1000 population [4]. Over 80% of deliveries take place in the main government hospitals and the rest are in the Bahrain Defence Force hospital and other private hospitals.
The main objective of this paper was to report the national maternal mortality rate in Bahrain over an 18-year period and the main causes of maternal death, and to compare these data with regional and international data. The other objective was to establish the causes of avoidable death and to highlight where improvements in care and services can be made.
Methods
Salmaniya Medical Complex is the main government hospital in Bahrain where most high-risk deliveries take place with an annual number of births of about 5000–6000. There are 2 other peripheral maternity hospitals (Jidhafs and Muharraq), both run by the staff of Salmaniya Medical Complex. The number of deliveries at Jidhafs is about 3500 per year, while in Muharraq about 1500–2000 per year. The second largest hospital in Bahrain is the Bahrain Defence Force hospital where the number of deliveries is about 3000 per year. This hospital serves mainly military families, emergency cases and private patients. There are several private hospitals in Bahrain where the number of deliveries varies from 30–300 per year. So Salmaniya Medical Complex is the main referral centre for all other hospitals in Bahrain, because a blood bank and all key facilities are available here.
In Bahrain all maternal deaths are reported to the Health Information Directory at the Ministry of Health (MOH). There were 60 maternal deaths during the 18 years 1987–2004. With the help of the administration department of Salmaniya Medical Complex and Bahrain Defence Force hospitals all the medical files were obtained and reviewed by the authors. Out of 60 cases, 1 patient had arrived in the accident and emergency department dead, at term, and her medical file could not be traced in any hospital. However, some data were available from the data processing office in Bahrain and from interviews with the relatives of the patient.
The information extracted from the files included the following: date of admission, date of death, age, parity, period of gestation, diagnosis, mode of delivery, management and outcome. All maternal deaths were discussed at the departmental meetings along with a maternal mortality meeting at both these hospitals and decisions were made as to whether the death was avoidable or unavoidable. Where avoidable, factors were identified such as a fault with the clinical management, failure of medical facilities or a failure on the part of the patient. The immediate cause of death was classified into direct and indirect causes. Direct causes were deaths resulting from obstetric complications due to interventions, omissions or incorrect treatment. Indirect causes of death were due to an existing disease or disease aggravated during pregnancy, as defined by the World Health Organization. The deaths were studied in relation to age, parity, period of gestation and mode of delivery. For religious reasons, autopsies were not performed. We followed the definition of maternal death in the International statistical classification of diseases and related health problems, 10th revision [5] and the denominator was the total births, which includes live births and stillbirths.
Results
There were a total of 243 232 deliveries during the study period 1987–2004 and 60 maternal deaths, giving an average maternal mortality rate of 24.7 per 100 000 total births. Figure 1 shows the annual distribution.
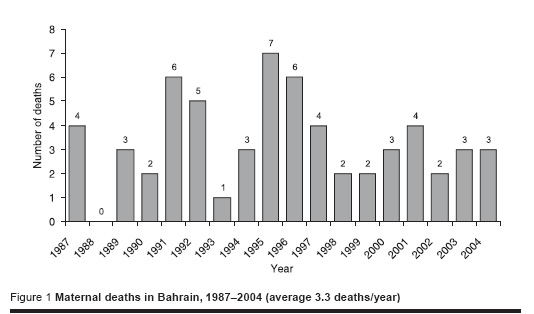
Table 1 shows maternal deaths by age and parity. The proportion of maternal deaths was highest in patients in the age group 35–39 years (30.0%) and in those with parity 5+ (28.3%).
Of the maternal deaths, 81.7% were in the MOH hospitals and 18.3% were in the Bahrain Defence Force hospital. Of all deaths, 40.0% were at term, 21.7% at 30–36 weeks, 28.3% at 21–29 weeks and 10.0% at 20 weeks or less. There were 20 antenatal deaths and of the remaining postnatal deaths 18 women had a vaginal delivery, 16 had caesarean section and 6 had an abortion.
Out of 60 deaths, 43 (71.7%) were judged to be unavoidable and 17 (28.3%) were avoidable due substandard care provided by the medical team in 8 deaths (47.1%), administrative problems (lack of an ICU bed) in 7 (41.1%) and failure on the part of the patient in 2 (11.8%) (Table 2).
The main causes of death were sickle-cell disease (25.0%), hypertensive diseases (18.3%), haemorrhage (13.3%), embolism (13.3%), heart disease (11.7%), infection (8.4%) and other (10.0%).
Direct causes were responsible in 32 (53.3%) cases and indirect causes in 28 (46.7%) cases (Table 3). Sickle-cell disease was the leading cause of death (15 cases) and the main indirect cause of death. In this group 7 (46.7%) deaths were due to acute chest syndrome, 7 (46.7%) due to vaso-occlusive crises and 1 (6.6) due to haemolytic crises. Of these women 8 (53.3%) died in the antenatal period, 6 (40.0%) in the postnatal period and 1 (6.7%) following abortion.
Hypertensive disease was the 2nd commonest cause of maternal death (11 cases) and the leading direct cause of death. The age of these women varied from 29 to 44 years; parity was 0–5 in 4 cases (36.3%) and 6+ in 7 cases (63.7%). The cause of death was encephalopathy in 4 (37.4%) cases, haemolytic elevated liver enzymes and platelets (HELLP) in 3 (27.2%) cases, pulmonary oedema and heart failure in 2 (18.2%) and disseminated intravascular coagulopathy in 2 (18.2%). There were 5 (45.4%) cases of eclampsia; 1 of the women was not booked into hospital and suffered a fit after home delivery. Out of these cases of hypertensive disease, 3 (27.2%) women died undelivered and 8 (72.8%) died in the postnatal period.
Obstetric haemorrhage was the 3rd commonest direct cause of death in this study (8 cases) and the age of the women varied from 28 years to 44 years and parity from 0–5 in 3 cases (37.5%) and 6+ in 5 cases (62.5%). The cause of bleeding was atonic haemorrhage due to placenta praevia with previous caesarean section in 3 (37.5%) cases, placenta accreta in 2 (25.0%), abruptio placenta in 2 (25.0%) and delayed postpartum haemorrhage in 1 (12.5%). Six of these women (75.0%) needed hysterectomy.
Discussion
Conducting audits of maternal deaths is one of the key steps towards improving maternity services. Every minute a woman dies from complications related to pregnancy and childbirth worldwide, which means 1500 deaths every day, more than half a million deaths every year; 99% of these deaths occur in the developing world [6]. The causes of maternal mortality are multiple, complex and inter-related and almost always preventable. When compared with other Gulf countries, such as Saudi Arabia and Oman, our results are similar [7,8]. The recording and auditing systems for these deaths need attention at the national level. A committee needs to be constituted to review each case of maternal mortality and identify preventable factors without blaming any individual.
Sickle-cell disease
Sickle-cell disease was the leading cause of death in our study (15 cases) and has remained the leading cause of indirect maternal deaths for the last 3 decades in this country [9,10], as this condition is endemic in this region. Since sickle-cell disease is a hereditary disease, it needs public education, frequent antenatal checkups, delivery in tertiary hospitals, family planning advice and compulsory premarital screening, which has been started already in this country. Pulmonary embolism and septicaemia was the ultimate cause of death in the majority of these women. Almost half the women with sickle-cell disease died due to acute chest syndrome and half due to vaso-occlusive crises; the remainder were due to haemolytic crises. Acute chest syndrome is known to be a common problem causing significant morbidity and mortality that may reach 50% [11]. Cases usually present with symptoms and signs of pneumonia, which could be due to infection, infarction, pulmonary sequestration or in situ thrombosis [12]. The cases with vaso-occlusive crises were due to ischaemia in the long bones and joints. So far there is no effective long-term method to reduce these crises. Combined care with the haematologist is required during the antenatal period or if there are any complications. Controversy surrounds prophylactic blood transfusion but we followed the policy of therapeutic transfusion [13]. An ICU bed was not available for 2 cases due to a shortage of beds, so we considered these deaths avoidable.
Hypertensive diseases
Hypertensive diseases are the commonest medical disorder affecting 7%–10% of all pregnancies in the United States [14]. They are known as one of the main causes of maternal death in both the developed and developing world. It was found to be the 2nd cause of maternal death in our study and the main direct cause (11 cases). The majority of cases were intracranial haemorrhage followed by HELLP, pulmonary oedema and heart failure and disseminated intravascular coagulopathy. The largest single cause of death with pre-eclampsia and eclampsia was intracranial haemorrhage, reflecting a failure in effective antihypertensive treatment [13].
There were 5% of patients who had eclampsia, which contributed to 8.3% of maternal mortality and this is comparable to some reported studies [15,16]. Three-quarters of the women had seizures in the intrapartum or postnatal period with one-quarter in the antenatal period. Magnesium sulfate has been the anticonvulsant of choice in eclampsia for the last 7 years [17]. A total of 3 out of 11 cases had HELLP syndrome, which is similar to some studies reported elsewhere [18]. HELLP is a rare but potentially serious complication of hypertension and in such cases the delivery of the baby should be commenced as the liver function can deteriorate rapidly.
There were 2 avoidable hypertensive disease deaths; 1 due to failure on the part of the patient to book into the clinic despite having very high blood pressure and the other died due to intracranial haemorrhage in a peripheral hospital as there was no ICU bed.
Haemorrhage
Life-threatening haemorrhage may occur in 6.7 in 1000 deliveries and can occur rapidly [19]. Worldwide, haemorrhage remains the most important cause of maternal mortality and almost 130 000 women bleed to death each year [20]. In 75% of women with haemorrhage there are no risk factors identified and some studies indicate that 90% could be due to uterine atony [21]. In our study we found that obstetric haemorrhage was the 2nd equal direct cause of death (8 cases). It is known that risks of haemorrhage rise significantly with age and parity as two-thirds of our patients were grand multiparas. The causes of bleeding were atonic haemorrhage due to placenta praevia, placenta accreta, delayed postpartum haemorrhage and abruptio placenta; 75% of patients needed hysterectomy. All the women who died with placenta praevia had had a previous caesarean section. Life-threatening haemorrhage occurs in 1 in 1000 deliveries with previous caesarean section and may need caesarean hysterectomy or uterine artery ligation or internal iliac artery ligation or uterine artery embolization [22]. Avoidable factors were identified in 3 cases due to delay in taking decisions for hysterectomy or to perform internal iliac artery ligation and in 1 case it was also due to delivery in the peripheral hospital where the facilities for blood transfusion were not adequate. Isolated maternity units distant from blood transfusion services and the lack of ICU present a particular risk when major haemorrhage occurs.
Pulmonary embolism (amniotic fluid embolism)
Pregnancy is a state of hypercoagulability and therefore there is an increased risk of thromboembolism. Pulmonary embolism is still the leading direct cause of maternal death in United Kingdom [23] and in our study it was the 2nd equal direct cause of maternal death (8 cases), out of which 3 cases were due to amniotic fluid embolism. All patients weighed more than 100 kg, so women with obesity, caesarean section and past history of pulmonary embolism should be considered as high-risk for pulmonary embolism [24]. Since the clinical diagnosis is unreliable, we suggest Doppler ultrasound and ventilation–perfusion scanning of the lungs as an important test to detect this disease, and the Royal College of Obstetricians and Gynaecologists guidelines for thromboprophylaxis should be followed strictly [25].
We lost 3 patients with the probable diagnosis of amniotic fluid embolism, which is a rare, unpredictable, unpreventable and often lethal condition [26[. The incidence in our institution is 1 in 12 000, which is comparable with the global incidence of 1 in 8000 to 1 in 80 000 pregnancies with a maternal mortality rate of 86% [27]. It was suspected in these patients as they suddenly developed marked cardiopulmonary distress in the absence of any other pathology.
Substandard care was identified in 3 cases as there was no ICU bed available for such cases and in 1 case there was also failure to give thromboprophylaxis to a patient with so many risk factors.
Cardiac disease
Haemodynamic changes during pregnancy are stressful to the cardiovascular system and become complicated with congestive heart failure in patients with heart lesions. The incidence of heart disease in Bahrain is about 0.7% [28]. Heart disease was responsible for 7 cases of indirect maternal deaths and similar results have been reported where cardiac disease still accounts for 15% of pregnancy-related mortality [29]. Valvular heart disease was once more common than congenital heart disease but now the ratio is 1 to 1.5 in favour of congenital heart disease. Valvular heart disease, either alone or in combination, was diagnosed in 5 cases and 1 case had atrial myxoma and 1 had postpartum cardiomyopathy. In the presence of heart disease, careful cardiac and obstetric management in a tertiary referral centre is recommended. Good patient compliance and high quality antenatal care may reduce mortality.
Substandard care was identified in 2 patients, in 1 due to inadequate heparinization in a patient with prosthetic valvular disease and in the other failure to terminate the pregnancy in the 1st trimester of pregnancy so that she could have valvotomy for tight mitral stenosis. Although surgery can be performed in pregnancy, most authors recommend early intervention in the nonpregnant state [30].
Genital tract sepsis
Maternal mortality due to sepsis is definitively decreasing and this change is attributed to good hygiene, less illegal abortion and use of broad-spectrum antibiotics [31]. However, sepsis can be life-threatening and can be of sudden onset. Infection was the direct cause of death in 5 patients in our study; 1 case had encephalopathy in the postpartum period, 3 had severe haemorrhage due to septicaemia and 1 had peritonitis due to undetected bowel injury following caesarean section. The risk of sepsis was increased as they had prolonged rupture of the membranes and the same findings have been seen by other studies [32]. We followed the policy of prophylactic antibiotics for all major surgery.
Avoidable death was found in 1 case where it was due to undetected bowel injury causing peritonitis after caesarean section in a patient who had previous 3 caesarean sections. Timely detection and management could have avoided this death.
Other causes
Six of the maternal deaths were due to various causes such as myeloid leukaemia, intracranial haemorrhage, liver cirrhosis, respiratory obstruction due to stricture in the neck and restricted mandibular moment, which made intubation impossible. We had no deaths due to ectopic pregnancy, multiple gestations or anaesthesia, and no late maternal deaths.
Conclusion and recommendations
We recommend that a confidential enquiry into maternal deaths be carried out at the national level every 3–5 years. In view of the fact that nearly half of avoidable deaths in this audit were due to lack of availability of ICU beds, we recommend that special ICU beds are made available for every sick patient near the labour room. Guidelines or protocols should be prominently placed in all wards and delivery suites and implementation of guidelines should be the subject of regular audit.
The following guidelines are suggested for the main categories of maternal death established in this study.
Sickle-cell disease. Combined care is needed with the haematologist. Patients should deliver in a tertiary hospital and emphasis should be given to family planning.
Hypertensive diseases. Educational material should be available to make women aware of symptoms associated with gestational hypertension. Protocols for the use of magnesium sulfate should be available for the prophylaxis of seizures, and strict attention given to fluid balance to avoid pulmonary oedema.
Pulmonary embolism. Basal body mass index should be calculated in all pregnant patients and the Royal College of Obstetricians and Gynaecologists guidelines for thromboprophylaxis should be followed.
Haemorrhage. An experienced consultant, anaesthetist and haematologist should be involved in any case of haemorrhage and the role of timely hysterectomy or internal iliac ligation or embolization should be emphasized.
Cardiac diseases. Termination, if indicated, should be done at an early stage of pregnancy without delay. Protocols for adequate heparinization for prosthetic valve disease along with combined care with the cardiologist should be practised.
Genital infections. Signs and symptoms of septicaemia should be recognized and adequate doses of antibiotics administered.
References
- Maternal mortality in 2000: estimates developed by WHO, UNICEF and UNFPA. Geneva, World Health Organization, 2004.
- Ghosh MK. Maternal mortality. A global perspective. Journal of reproductive medicine, 2001, 46:427–33.
- El-Shafei AM, Sandhu AK, Dhaliwal JK. A review of maternal death in Bahrain 1977–1986. Bahrain, Government Press, Ministry of Information, 1989.
- Health statistics 2004. Bahrain, Health Information Directorate, Ministry of Health, 2004.
- International statistical classification of diseases and related health problems, 10th revision. Geneva, World Health Organization, 1992.
- Reducing maternal deaths, The challenge of the New Millennium in Africa Region. Brazzaville, Congo, WHO Regional Office for Africa, 2002.
- Al-Meshari A et al. Epidemiology of maternal mortality in Saudi Arabia. Annals of Saudi medicine, 1995, 15(4):317–23.
- Suleiman AJM. Review of maternal mortality in Oman, 1992–2000. Community health and disease surveillance newsletter, 2000, 4:1–3.
- El-Shafei AM, Sandhu AK, Dhaliwal JK. Maternal mortality in Bahrain with special reference to sickle cell disease. Australian and New Zealand journal of obstetrics and gynaecology, 1988, 28:41–4.
- El-Shafei AM, Dhaliwal JK, Sandhu AK Pregnancy in sickle cell disease in Bahrain British journal of obstetrics and gynaecology,1992, 99:101–4.
- Al-Dabbous IA. Acute chest syndrome Saudi medical journal, 2002, 23(9):1037–44.
- Al-Hawsawi ZM. Acute chest syndrome in sickle cell disease. Saudi medical journal, 2004, 25(1):116–7.
- El-Shafei AM et al. Indications for blood transfusion in pregnancy with sickle cell disease. Australian and New Zealand journal of obstetrics and gynaecology, 1995, 35(4):405–8.
- August P, Lindheimer MD. Pathophysiology of preeclampsia. In: Laragh JL, Brenner BM, eds. Hypertension, 2nd ed. New York, Raven Press, 1995:2407–26.
- Davies JA, Prentice CRM. Coagulation changes in pregnancy-induced hypertension and growth retardation. In: Greer IA, Turpie AGG, Forbes CD, eds. Haemostasis and thrombosis in obstetrics and gynaecology London, Chapman and Hall, 1992:143–62.
- Granger JP et al. Pathophysiology of hypertension during preeclampsia linking placental ischemia with endothelial dysfunction Hypertension, 2001, 38:718–23.
- Magpie Trial Collaborative Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomized placebo–controlled trial. Lancet, 2002, 359:1877–90.
- Rajab KE, Abdull AA, Skerman JH. Help syndrome: incidence and management of such cases in the Kingdom of Bahrain Bahrain medical bulletin, 2003, 24:141–6.
- Rizvi F et al. Successful reduction of massive postpartum haemorrhage by use of guidelines and staff education. British journal of obstetrics and gynaecology, 2004, 111:495–8.
- Chong YS, Su LL, Arulkumaran S. Current strategies for the prevention of postpartum haemorrhage in the third stage of labour. Current opinion in obstetrics and gynecology, 2004, 16:143–50.
- O’Leary JA. Uterine artery ligation in the control of postpartum haemorrhage. Journal of reproductive medicine, 1995, 40:189–93.
- Hong TM et al. Uterine artery embolisation: an effective treatment for intractable obstetric haemorrhage. Clinical radiology, 2004, 59:96–101
- Drife J. Thromboembolism. British medical bulletin, 2003, 67:177–90.
- Greer IA. Epidemiology, risk factors and prophylaxis of venous thromboembolism in obstetrics and gynecology. Clinical obstetrics and gynecology, 1997, 11:403– 30.
- Thromboprophylaxis during pregnancy, labour and after normal vaginal delivery.Guideline No. 37. London, Royal College of Obstetricians and Gynaecologists, 2004.
- Tuffnell D. Amniotic fluid embolism. Current opinion in obstetrics and gynecology, 2003, 15:119–22.
- Martin RW. Amniotic fluid embolism. Clinical obstetrics and gynecology, 1996, 39(1):101–6.
- Rajab KE, Issa AA. Peripartum cardiomyopathy: a five-year hospital-based analytical study. Bahrain medical bulletin, 2004, 26(3):95–8.
- Faiz SA, Al-Meshari AA, Sporrong BG. Pregnancy and valvular heart disease.Saudi medical journal, 2003, 24(10):1098–101.
- Thilen U, Olsson SB. Pregnancy and heart disease: a review. European journal of obstetrics, gynecology, and reproductive biology, 1997, 75:43–50.
- Chabra K, Kaipa A, Kakani A. Reduction in maternal mortality due to sepsis. Journal of obstetrics and gynaecology, 2005, 25(2):140–2.
- Giles M, Garland S, Oats JJ. Management of preterm prelabour rupture of membranes: an audit. How do the results compare with clinical practice guidelines? Australian and New Zealand journal of obstetrics and gynaecology, 2005, 45(3):201–6.








