Infectious disease outbreaks reported in the Eastern Mediterranean Region in 2020
Background
In 2020, the World Health Organization’s (WHO) Eastern Mediterranean Region witnessed the coronavirus disease 2019 (COVID-19) pandemic as an emerging infectious disease caused by the high-threat pathogen named SARS-CoV-2. By the end of the year approximately 5 million cases were reported, including 121 778 associated deaths from all 22 countries of the Region, revealing a case-fatality ratio (CFR) of 2.5%.
Furthermore, 10 major outbreaks by other emerging infectious diseases occurred in 7 countries of the Region. These outbreaks included poliomyelitis in Afghanistan and Pakistan, chikungunya in Somalia and Sudan, cholera in Somalia and Yemen, dengue fever in Pakistan and Yemen, diphtheria in Sudan and Yemen, Crimean-Congo haemorrhagic fever in Afghanistan and Pakistan, chickenpox (varicella) in Pakistan, Middle East respiratory syndrome (MERS) in Saudi Arabia, and viral haemorrhagic fever in Sudan. More than 430 000 reported cases and more than 400 associated deaths resulted from these 10 outbreaks, which were monitored while technical, management and logistical support was provided to detect, confirm, and respond to these outbreaks. Failure to fully contain previous outbreaks also led to sporadic reporting of cases of other diseases in endemic patterns (Fig. 1).
The likelihood of the emergence and rapid transmission of high-threat pathogens in the Region has increased in recent times. Many countries are directly or indirectly affected by acute or protracted humanitarian emergencies, leading to fragile health systems, as well as high numbers of internally displaced persons and refugees, who have little or no access to basic health care services and environmental infrastructure.
Other risk factors for infectious disease outbreaks include rapid or unplanned urbanization, climate change, increased human-animal interaction, weak surveillance and limited laboratory diagnostic capacity, poor infection prevention and control measures in health facilities, and insufficient risk communication and community engagement efforts. Moreover, the COVID-19 pandemic has had a significant impact on various aspects of health and on the provision of health services, overstretching already fragile health systems.
The WHO Health Emergencies Programme (WHE) in the WHO Regional Office for the Eastern Mediterranean works on the prevention, preparedness, detection and response to high-threat pathogens and other public health emergencies. While these areas of work remain a top priority for WHE, available resources were repurposed in order to boost the COVID-19 pandemic response and minimize the impact of the pandemic on societies and economies.
In response to the second goal of WHO's Thirteenth General Programme of Work (GPW 13) to make “one billion more people better protected from health emergencies”, and its second programme budget outcome of “epidemics and pandemics prevented”, the Infectious Hazard Prevention and Preparedness (IHP) unit of WHE continued to provide technical support to affected countries to prevent or contain outbreaks through the application of proven and appropriate evidence-based public health control measures for priority pandemic- or epidemic-prone diseases. While responding to the urgent and unprecedented COVID-19 pandemic in this Region, WHO’s Regional Office has undertaken measures to protect and promote critical essential health services.
IHP maintains disease-specific epidemiological data received from country offices and ministries of health on major disease outbreaks through its central database ‒ the Outbreak and Public Health Event Portal (OPHEP). This online portal is used to monitor disease outbreak trends in the Region and the progress of response measures.
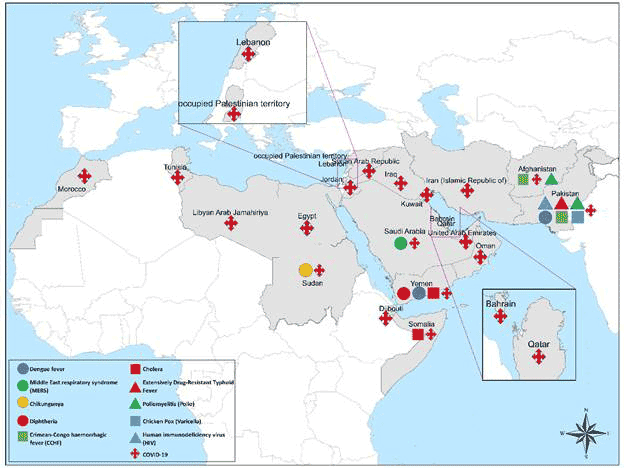
Fig. 1. Countries of WHO’s Eastern Mediterranean Region reporting infectious disease outbreaks in 2020
Challenges
WHO and other partners have faced multiple challenges in the provision of technical support to countries to improve their capacities to respond to these emerging and re-emerging infectious disease outbreaks. Most significantly, the majority of outbreak-affected countries were experiencing protracted or acute emergencies with disrupted or under-performing health systems, such as Somalia, Sudan and Yemen. In other countries, such as Afghanistan and Pakistan, financial and capacity issues impacted the performance of their health systems.
Prolonged insecurity and inaccessibility in countries with complex emergencies (such as Iraq, Somalia, Syria and Yemen) usually resulted in the delayed implementation of key planned activities and the under-utilization of committed resources, potentially leading to the rapid spread of high-threat pathogens to other areas. The high frequency of natural disasters (such as floods, droughts and heavy rains) was another major challenge, aggravating the existing situation and increasing the number of outbreaks. With persistent demand from countries for greater technical, logistical and financial support to tackle the outbreaks, it was sometimes difficult to find the required funding, technical staff and supplies. Many countries in the Region are lacking necessary political commitment and investment to improve preparedness, prevention and mitigation in the event of a major disease outbreak or pandemic.
Another challenge was the lack of integrated response plans within affected countries, and this can lead to fragmented response efforts to contain outbreaks. Some outbreaks required the involvement of multiple ministries for infrastructure development (such as clean water supply, sanitation and disaster preparedness) and improvement of preparedness and response capacities. The lack of public awareness on preventative measures against common infectious diseases, such as cholera and vector-borne diseases, contributed to the rapid spread of these outbreaks.
Recommendations
Governments and all stakeholders should allow local partners and donor organizations to access emergency-affected areas and provide essential health services.
Ensure continuous engagement with external partners and donors to build trust, encourage the pooling of resources and help build consensus on division of responsibilities, thus avoiding wastage and duplication of efforts and resources. Local partners should be engaged to provide logistical support within country, if WHO is not present.
Comprehensive joint preparedness and response strategies should be developed through coordination between governments and external partners to enable a coordinated response and the pooling of resources. Countries facing multiple vector-related outbreaks should develop integrated plans for optimal use of resources and simultaneous control. Countries facing repeated waterborne outbreaks should update or develop comprehensive national cholera control plans aligned with “Ending cholera: a global roadmap to 2030”.
Regular evaluations (external, internal and joint) should be conducted to assess the impact of response activities and identify and address gaps. Prioritization of issues should be based on threat perception and sensitivity, with resources allocated accordingly. New efficient tools should be developed and adapted for capacity-building in case diagnosis, investigation and prevention.
The COVID-19 response should be reinforced at the regional, national, subnational, and community levels, particularly by strengthening existing partnerships and multisectoral collaboration, addressing misinformation, improving surveillance and reporting, encouraging research, innovation, and information-sharing, maintaining essential health services, and building capacity in infection prevention and control.
Laboratory capacity should continue to expand across the Region to test for SARS-CoV-2 and to sequence the virus.
Adherence to public health and social measures should be reinforced and maintained alongside the COVID-19 vaccine rollout.
Fair and equitable distribution of COVID-19 vaccines, COVID-19 diagnostic tests, therapeutics, and personal protective equipment (PPE) must be ensured.
Specific efforts are required to:
strengthen infectious disease surveillance systems;
improve diagnostic capacities and laboratory systems;
strengthen infection prevention and control;
improve clinical case management to minimize mortality;
improve risk communications and engagement with communities;
strengthen rapid response capabilities for more timely response and containment; and
conduct operational research on high-threat infectious diseases to improve preparedness, particularly through studies on the burden of disease, modelling and forecasting.
Disease outbreaks responded to in 2020 by country
1. Chickenpox (Varicella)
Pakistan
Since April 2017, Pakistan has faced a significant upsurge in reported chickenpox (varicella) cases and up until September 2020, a total of 19 097 cases with 21 related deaths (CFR = 0.1%) had been reported. Between January and September 2020, a total of 235 cases of chickenpox were reported in Punjab province without any deaths (Fig. 2). A higher number of cases was reported during the first quarter of the year, but sporadic cases continued to be reported until epidemiological week 36.
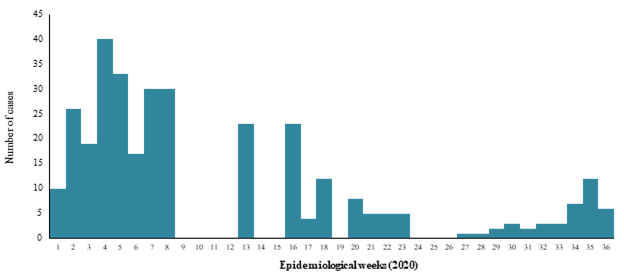
Fig 2. Number of suspected chickenpox cases reported in weeks 1-36, Punjab, Pakistan
WHO is providing support to Pakistan to enhance disease surveillance and laboratory confirmation of suspected cases, map hotspots, strengthen risk communication and community engagement, promote routine vaccination, and share guidelines for case management to reduce morbidity and mortality from disease.
2. Chikungunya
Sudan
From week 33 (16‒22 August 2020) to week 47, 2020, Sudan reported 577 cases of chikungunya from 4 states (Fig. 3). The most affected state was West Darfur (500 cases). Cases were also reported from North Darfur (62 cases), East Darfur (14 cases) and South Darfur (1 case). The samples were laboratory-confirmed both by rt-PCR and serology. Sudan reported its first ever outbreak of chikungunya in 2018 (48 763 cases, 0 deaths) with far fewer numbers of cases reported in the year 2020. This decrease is mostly due to enhanced surveillance and the implementation of response measures, including extensive vector surveillance and management. Fig. 4 shows the geographical distribution of chikungunya cases reported in 2020.
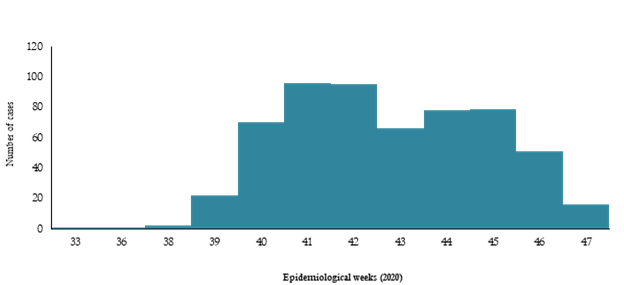
Fig. 3. Number of chikungunya cases reported in 2020, Sudan
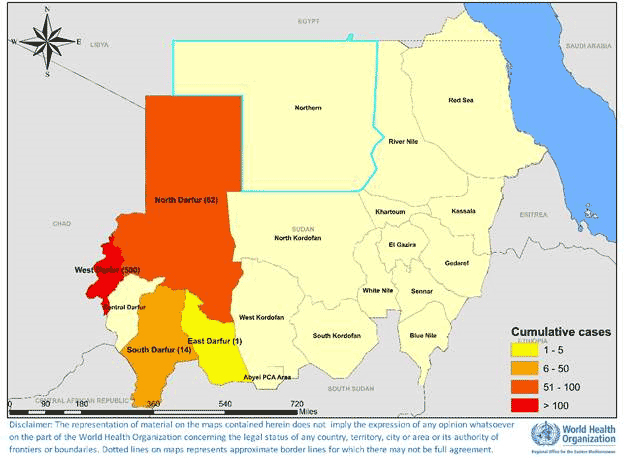
Fig. 4. Geographical distribution of chikungunya cases reported in 2020, Sudan
WHO provided support to the Ministry of Health in disease surveillance, capacity-building for laboratory confirmation of suspected cases and provision of testing kits, health awareness and risk communication materials, and funding for vector control activities, such as larvae control, adult control, spraying and fogging, and provision of mosquito nets. Experts from the Regional Office were also deployed on a rotational basis to build capacity at the country level.
3. Cholera
Somalia
Cholera is a disease endemic to Somalia. Since December 2017, when the first cholera cases were laboratory-confirmed in Beletweyne district of the Hiraan region following heavy rains, the outbreak spread to 27 districts in 4 regions located in the river basins of Jubba and Shabelle. The outbreak has continued since then and was exacerbated by the flash floods caused by heavy Gu rains in April 2020 that displaced over 400 000 people in 23 districts of the country. Moreover, in June, towns located along the Shabelle River suffered from Hagaa rains that led to the contamination of the water source and an increase in cholera cases. During 2020 (January to December), a total of 6582 suspected cholera cases, including 33 associated deaths, were reported (CFR = 0.5%). Most of the reported cases were from the Banadir region. The cumulative number of suspected cases reported since December 2017 are 16 756, including 83 deaths (CFR = 0.49%). Of the 587 stool samples that were tested at the National Public Health Laboratory in Mogadishu since the start of the outbreak, a total of 175 samples tested positive for Vibrio cholerae, serotype O1 Ogawa (Fig. 5).
In Baidoa, Bay region, a new outbreak started at the beginning of May 2020 among 50 000 people who were internally displaced following flash floods. In 2020, a total of 935 cholera cases including 3 deaths (CFR = 0.3%) were reported between weeks 22 and 52, of which 459 cases (49%) were children aged 2 years and younger. Fig. 6 shows the geographical distribution of suspected cholera cases reported from Somalia in 2020.
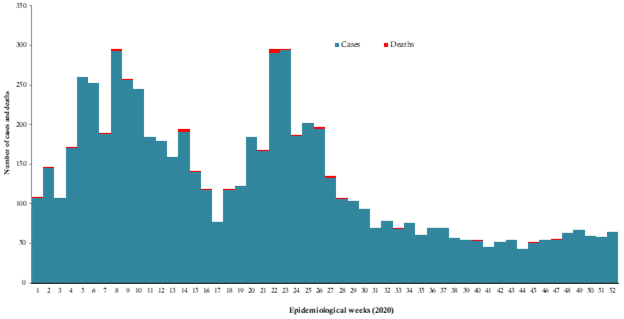
Fig. 5. Suspected cholera cases and deaths reported in Somalia, weeks 1-52, 2020
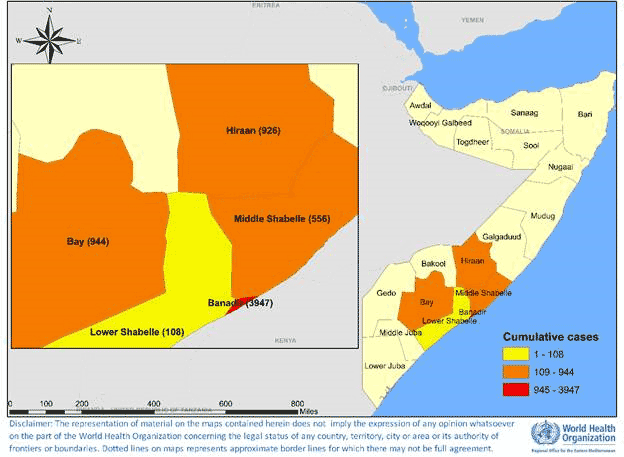
Fig. 6. Geographical distribution of suspected cholera cases reported from Somalia in 2020
WHO has continued to support the Government of Somalia since the start of the outbreak in 2017. The overall reduction in the number of new cholera cases as compared to the beginning of the outbreak is attributed to enhanced implementation of preventive interventions, including oral cholera vaccination campaigns, distribution of risk communication materials and the strengthening of water, sanitation and hygiene (WaSH) activities in hotspots. Disease surveillance is being managed with the support of WHO through an electronic system known as the Early Warning Alert and Response Network (EWARN). WHO and the Ministry of Health continuously monitored outbreak trends through EWARN to promptly investigate and respond to all alerts.
Yemen
The cholera outbreak reported in Yemen since October 2016 continued to affect the entire country in 2020. Although the trend was on the increase at the beginning of the year with the number of cases continuing to be reported at a steadily high level until week 14, it later started to decline although the number of cases remained relatively high. The cumulative number of suspected cholera cases reported from January to December in 2020 was 230 121 with 84 associated deaths (CFR = 0.04%). A total of 1360 samples were tested at the central public health laboratories during the year, of which 134 were confirmed as cholera-positive by culture (Fig. 7). Fig. 8 shows the geographical distribution of suspected cholera cases reported from Yemen in 2020.
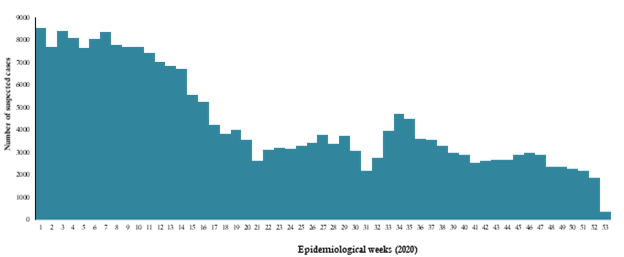
Fig. 7 Susspected cholera cases and deaths reported in Sudan in 2019
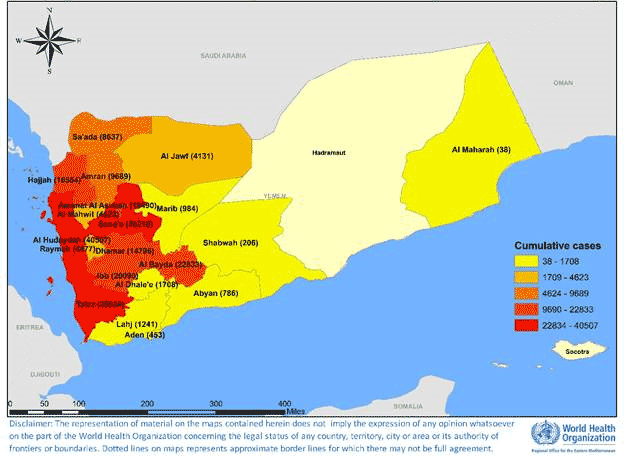
Fig. 8. Geographical distribution of suspected cholera cases reported from Yemen in 2020
The health system in Yemen has been severely weakened as a result of the ongoing conflict. WHO is supporting the Ministry of Public Health and Population in multiple ways, including enhancing disease surveillance through EWARN, providing rapid diagnostic and laboratory testing kits, mapping hotspot areas, implementing WASH activities, administering oral cholera vaccines to high-risk populations, providing supportive medicines and conducting case management training.
In 2020 support was also provided for cholera case management, laboratory investigation, oral cholera vaccination campaigns and upgrading electronic Disease Early Warning System (eDEWS) surveillance. However, the outbreak has still not been well contained due to the complexity of the situation, including lack of infrastructure, limited resources and inadequate staffing.
4. Crimean-Congo haemorrhagic fever (CCHF)
Afghanistan
Crimean-Congo haemorrhagic fever is endemic to Afghanistan, with an upsurge in cases reported in 2018 and 2020. The number of reported cases peaked in August 2020 (Fig. 9). From January to December 2020, a total of 184 suspected cases, including 15 associated deaths (CFR = 8.2%) were reported in the country. Most of the cases were reported from Herat and Kabul provinces (Fig. 10). The increase in the number of cases reported in recent years has been mainly attributed to improved surveillance and reporting mechanisms.
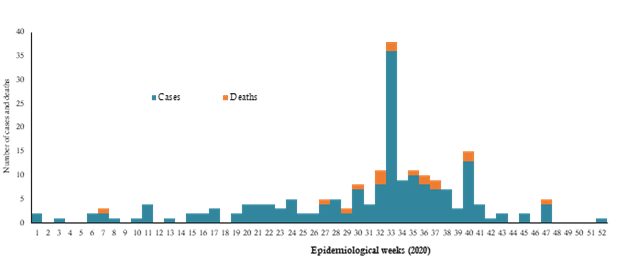
Fig. 9. Crimean-Congo haemorrhagic fever cases and deaths reported from Afghanistan, weeks 1-52, 2020
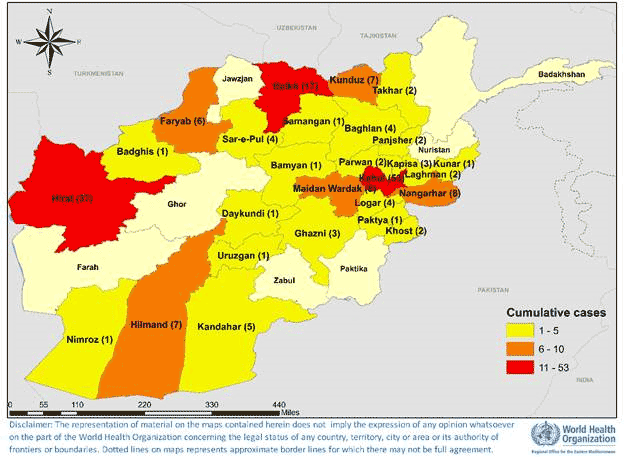
Fig. 10. Geographical distribution of Crimean-Congo haemorrhagic fever cases reported from Afghanistan in 2020
WHO continued to support the Ministry of Public Health of Afghanistan to strengthen multisectoral coordination and ensure the integration of outbreak response and control interventions. The frequency of reporting was increased to daily reporting to enhance surveillance, and health awareness was raised by targeting high-risk areas through the sharing of information, education and communication materials. The capacities of rapid response teams in outbreak response were built with a focus on Crimean-Congo haemorrhagic fever. Operational plans to accelerate the response were developed.
Pakistan
Crimean-Congo haemorrhagic fever also remains endemic to Pakistan, where the country has experienced a number of outbreaks during the last few years. Initially, cases were reported from its established foci, such as Balochistan, but other provinces and areas are currently reporting as well. The frequent unmonitored movement of animals and animal products remains the major cause of the spread of the virus throughout the country. In 2020, a total of 19 confirmed cases were reported (Fig. 11).
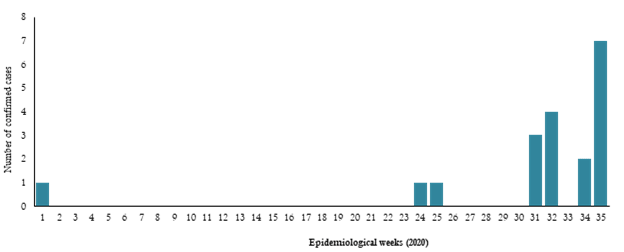
Fig. 11. Laboratory-confirmed cases of Crimean-Congo haemorrhagic fever in 2020, Pakistan
WHO extended support to Pakistan to enhance coordination in detecting Crimean-Congo haemorrhagic fever, as well as building laboratory capacity to confirm suspected cases. Laboratory kits and training were provided to the central public health laboratory. Some gaps were identified in surveillance and response measures during periodic reviews and WHO is engaged with the Government to strengthen the measures currently in place.
5. Dengue fever
Pakistan
Pakistan has been experiencing outbreaks of dengue fever for the past several years, affecting different parts of the country on a regular basis. The main vector of dengue virus transmission, Aedes aegypti, is well established in all parts of the country. In 2020, a total number of 5758 confirmed dengue cases were reported with 125 794 suspected cases from all 4 provinces and the Islamabad Capital Territory (ICT) of Pakistan. Ten (10) deaths were reported from dengue (6 from Punjab, 3 from Karachi and 1 from Islamabad) in 2020 (CFR = 0.01%).
The number of deaths was the lowest in 2020 compared to previous dengue outbreaks in the country. The epidemic reached its peak in November but the number of reported cases started declining from late November in all parts of the country (Fig. 12). Fig. 13 shows the geographical distribution of confirmed dengue fever cases reported from Pakistan in 2020.
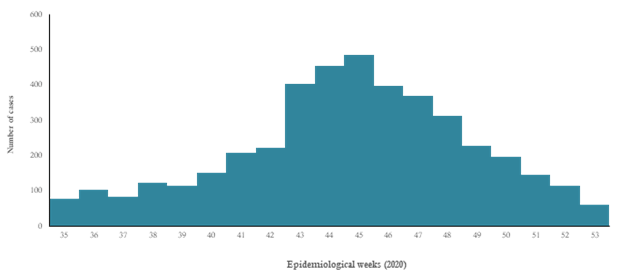
Fig. 12. Laboratory-confirmed cases of dengue fever in 2020, Pakistan
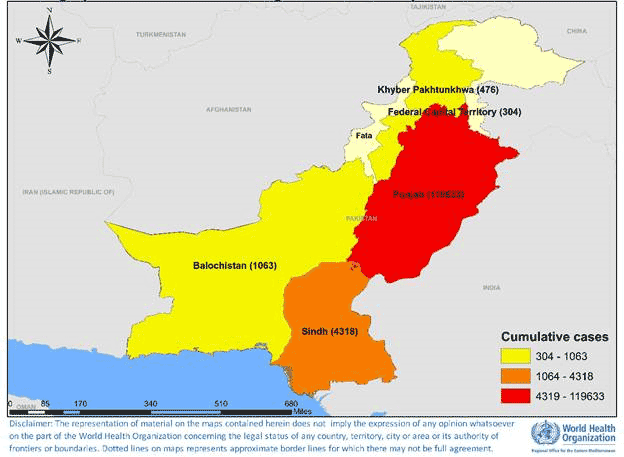
Fig. 13. Geographical distribution of suspected and confirmed dengue fever cases reported from Pakistan in 2020
WHO supported the Government with the provision of case diagnosis and management guidelines throughout the country. Information, education and communication materials were distributed to raise the awareness of the general public on prevention measures to reduce risks. WHO also deployed experts for dengue vector control activities, as well as for case management, laboratory investigation and emergency risk communication. Support was also provided to the Government through the timely arrangement of medical supplies for management of severe cases (including fluids and crystalloids).
Yemen
A dengue fever outbreak was reported from the Shabwah governorate of Yemen in January 2018, which continued into 2020. From January to December 2020, a total of 65 183 cases, including 175 deaths (CFR = 0.3%), was reported across the country. In total 1187 (IgG) and 1550 (IgM) cases were confirmed by Elisa at the National Center for Public Health Laboratories. Owing to the presence of Aedes mosquitoes in the country and heavy rains during the end of 2019, a continuous increase in the number of reported cases was observed during the start of 2020 until week 2 before it started to decline. (Fig. 14). Fig. 15 shows the geographical distribution of dengue fever cases reported from Yemen in 2020.
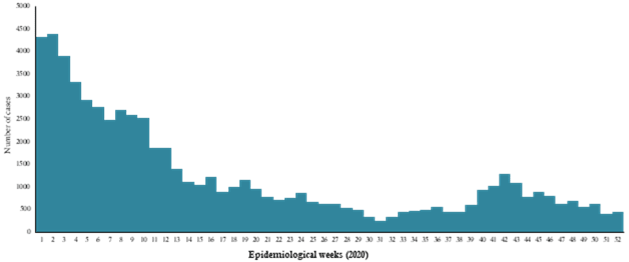
Fig. 14. Suspected dengue fever cases reported from Yemen in 2020
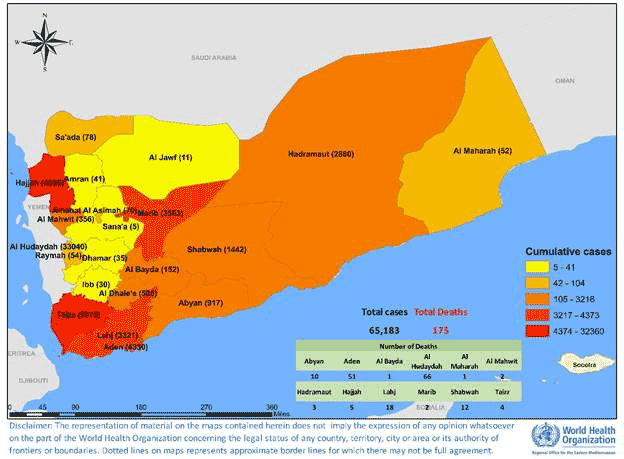
Fig. 15. Geographical distribution of dengue fever cases reported from Yemen in 2020
WHO is supporting the Government to conduct disease surveillance through the electronic Diseases Early Warning System (eDEWS) due to disruption of the routine surveillance system. Regular technical and financial support is also being extended for laboratory diagnosis and confirmation, case management and vector control activities. Efforts are under way to strengthen the surveillance system for better case detection, as well as mapping hotspot areas for targeted campaigns to control the outbreak. Collaboration is continuing with national and international partners to conduct an integrated response and for optimal utilization of resources.
6. Diphtheria
Yemen
In October 2017, Yemen began experiencing an outbreak of diphtheria that spread to most districts in 23 governorates. By December 2020, a total of 6765 suspected cases were reported with 429 related deaths (CFR = 6.3%), including 700 laboratory-confirmed cases. From January to December 2020 a total of 1710 cases were reported with 134 associated deaths (CFR = 7.8%) (Fig. 16). The most affected age group was 6‒15 years. In 2020, most of the cases reported were from Sa’ada governorate (Fig. 17).
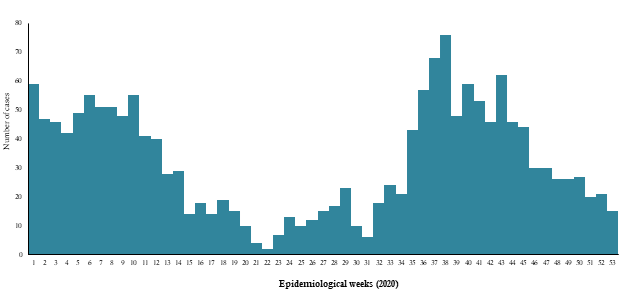
Fig. 16. Diphtheria cases reported in Yemen, 2020
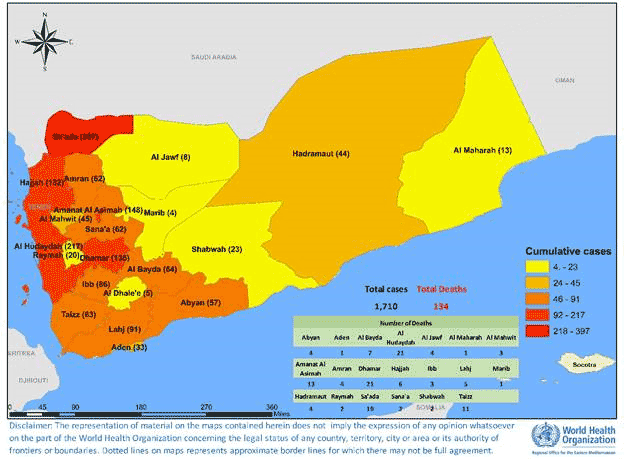
Fig. 17. Geographical distribution of diphtheria cases reported from Yemen in 2020
WHO provided support to the local health authorities in disease surveillance and laboratory confirmation of suspected cases through the provision of logistical and technical resources. In addition to routine immunization activities, supplementary immunization campaigns were conducted to protect those people at high risk for diphtheria. During 2020, targeted immunization campaigns in high-risk governorates were held to boost the number of immunized children, with the Penta vaccine administered to children from 6 weeks to 5 years old while the tetanus-diphtheria (Td) vaccine was administered to children 5‒15 years old.
7. Extensively drug-resistant typhoid fever
Pakistan
Since November 2016, Pakistan has continued to report cases of extensively drug-resistant (XDR) typhoid fever after cases were first detected in the district of Hyderabad in Sindh province. Cases continued to be reported from other districts of Sindh province, with most (72%) being reported from Karachi district (Fig. 18). Up until December 2020, a total of 18 850 cases were reported from different districts of Sindh province (Table 1), of which 3633 cases were reported during 2020.
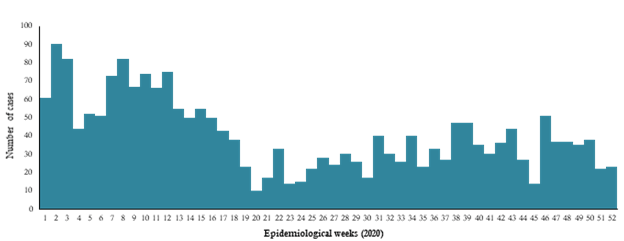
Fig. 18. Extensively drug-resistant typhoid fever cases reported in Karachi, Pakistan in 2020
Table 1. Extensively drug-resistant typhoid fever cases reported from December 2016 to December 2019, Sindh, Pakistan
|
Year |
Karachi |
Hyderabad |
Other districts |
Total |
|
2016 |
0 |
12 |
0 |
12 |
|
2017 |
175 |
485 |
4 |
664 |
|
2018 |
3712 |
891 |
207 |
4810 |
|
2019 |
7088 |
1645 |
998 |
9731 |
|
2020 |
2510 |
708 |
415 |
3633 |
|
Grand Total |
13 485 |
3741 |
1624 |
18 850 |
The number of suspected cases of XDR typhoid fever increased during each successive year (only one province, Sindh, reported cases), with the highest number reported in 2019 (9731). WHO extended support for laboratory confirmation of suspected cases and the preparation of case management guidelines for confirmed cases. Pakistan became the first country in the world to introduce the WHO-approved typhoid conjugate vaccine in its Expanded Programme on Immunization on 18 November 2020.
8. Middle East respiratory syndrome (MERS)
Saudi Arabia and Qatar
MERS cases continued to be reported sporadically throughout 2020, mostly from Saudi Arabia. During this year, a total of 61 laboratory laboratory-confirmed cases were reported as compared to 223 cases in 2019, 147 in 2018, 250 in 2017 and 249 in 2016. Of the total cases reported in 2020, Saudi Arabia reported 60 cases while Qatar reported one case (Fig. 19).
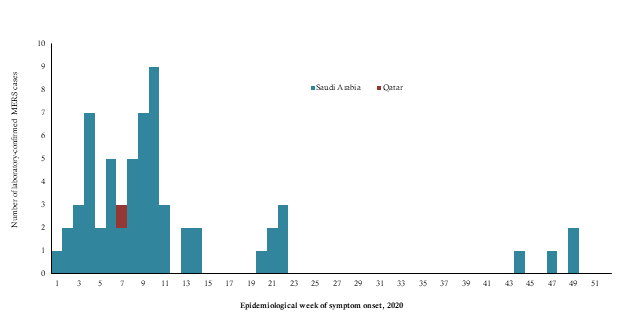
Fig. 19. MERS cases reported in the Region by week of symptom onset, 2020
MERS hospital and household clusters reported in 2020
In 2020, 2 nosocomial outbreaks of MERS were reported from Saudi Arabia (Table 2). The first outbreak was reported in January with a cluster of 6 cases. Three (3) of the cases were health care workers, 2 were patients (one of whom died) and one was a visitor. The source of infection of the first case reported in the cluster is still unknown. The second outbreak was reported in May with a total of 6 laboratory-confirmed cases with 4 associated deaths. Five cases had a history of contact with the first reported case (probable index case), whose source of infection is still unknown.
Table 2. MERS hospital outbreaks reported in 2020
|
Outbreak |
Date of first reported case |
Date of last reported case |
Total cases |
Died |
Health care worker |
Asymptomatic |
|
Asir |
20 January 2020 |
12 March 2019 |
6 |
1 |
3 |
2 |
|
Alkharj |
21 May 2020 |
31 May 2020 |
6 |
4 |
1 |
0 |
9. Poliomyelitis
Polio is the second vaccine-preventable disease that the world is working to eradicate in the near future. On World Polio Day 2020 (October 24) it was announced that wild poliovirus (WPV) type 3 was eradicated worldwide following the eradication of WPV type 2 in 2015. The Eastern Mediterranean Region contains the last 2 polio-endemic countries worldwide, namely Afghanistan and Pakistan. As of 31 December 2020, a total of 140 WPV1 cases were reported in the Region: 84 from Pakistan and 56 from Afghanistan (Fig. 20).
_cases_reported_from_afghanistan_and_pakistan_in_2020.png)
Fig. 20. Geographical distribution of poliomyelitis (WPV1) cases reported from Afghanistan and Pakistan in 2020
Afghanistan
In 2020, 56 WPV1 cases were reported: 38 cases from the southern region, 8 from the western region, 6 from the southeastern region, 2 from the eastern region and 1 each from the northern and Badakhshan regions. (Fig. 20).
Pakistan
In 2020, 84 WPV1 cases were reported: 26 from Balochistan province, 22 cases each from Khyber Pakhtunkhwa and Sindh provinces, and 14 from Punjab province. (Fig. 20).
Circulating vaccine-derived poliovirus-2 (cVDPV) cases
In 2020, 5 countries in the Region reported vaccine-derived polioviruses (VDPV) cases: 422 cVDPV type 2 (240 from Afghanistan, 121 from Pakistan, 13 from Somalia and 48 from Sudan) and 18 cVDVP type 1 from Yemen.
Furthermore, there were 106 positive environmental samples for cVDPV2 (including 77 a mixture of WPV1 and cVDPV2). Also, there were 12 aVDPV2 isolates detected in the environment samples, which include 4 combined (WPV1 + aVDPV2) from Pakistan. From Afghanistan a total of 149 cVDPV2-positive environmental samples, including 6 a mixture of WPV1 and cVDPV2, were reported. Also, there is 1 aVDPV2 isolate detected in the environment. Positive environmental samples were also reported from Egypt (1 positive sample for cVDPV2) and Islamic Republic of Iran (2 positive samples for VDPV2).
10. Coronavirus disease 2019 (COVID-19)
On 31 December 2019, WHO was informed of the detection of a cluster of pneumonia of unknown aetiology in Wuhan City, Hubei Province of China. A novel coronavirus (tentatively named 2019-nCoV) was identified as the causative virus on 7 January 2020. As the emergence of this new deadly pathogen in China posed a significant global health challenge due to its rapid proliferation in China making global human-to-human transmission possible, the Emergency Committee was convened by WHO’s Director General under the International Health Regulations (IHR 2005) and COVID-19 was declared a Public Health Emergency of International Concern (PHEIC) on 30 January 2020.
On 29 January, the Eastern Mediterranean reported its first cases of 2019-nCoV following confirmation on the same day of 4 cases by the Ministry of Health and Prevention in the United Arab Emirates. On 11 February, WHO announced “COVID-19” as the official name of this new disease and on 11 March WHO described the COVID-19 outbreak as a pandemic. This description was associated with concerns over the geographical spread of the disease as it affected countries on all continents. The COVID-19 outbreak continued to spread, and cases were eventually reported from over 180 countries, territories and areas globally.
In 2020, the Region reported approximately 5 million cases with 121 778 associated deaths (CFR = 2.5%) from all 22 countries of the Region. There were 2 waves of the pandemic observed in 2020 across the Region (Fig. 21.). The first wave started in epidemiological week 16 with a gradual increase until it peaked in epidemiological week 25 with more than 130 000 reported cases. A steady decline followed with the implementation of strict public health and social measures. The second wave started around epidemiological week 36, peaking in week 47 when the highest recorded number of cases reached 251 530.
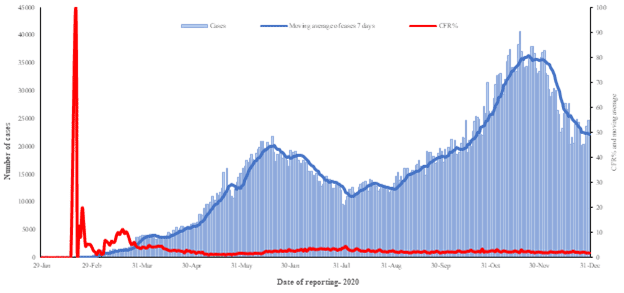
Fig. 21. Distribution of daily COVID-19 cases and CFR in the Region, 29 January to 31 December 2020
Since the beginning of the outbreak, Islamic Republic of Iran has reported the highest number of total cases in the Region (1 237 474 cases; 24.8% of the Region’s total), followed by Iraq (597 033; 12%) and Pakistan (486 634; 9.8%). Islamic Republic of Iran also reported the highest number of total associated deaths (55 438; CFR = 4.5%) followed by Iraq (12 829; CFR = 2.1%) and Pakistan (10 311; CFR = 2.1%). The highest CFRs were reported by Yemen (29%) followed by Sudan (6.3%), while the lowest CFRs were reported by Qatar (0.2%) followed by the United Arab Emirates (0.3%) and Bahrain (0.4%).
In terms of testing, a total of 70 629 404 laboratory PCR tests have been conducted since the start of the outbreak across the Region. The highest number of PCR tests conducted were reported from the United Arab Emirates (21.2/million), followed by Saudi Arabia (11.1/million) and Islamic Republic of Iran (7.7/million). The United Arab Emirates and Bahrain have the highest rates of testing per capita (2142/1000 and 1400/1000, respectively). Throughout 2020, the average positivity rate for the Region ranged between 5.5% and 7.1%.
Over a year has passed since the reporting of the first COVID-19 case detected in the Region. At the time, the WHO Regional Office for the Eastern Mediterranean had activated the Incident Management Support Team (IMST) structure to support and coordinate readiness and response efforts to the COVID-19 pandemic. The IMST at the Regional Office provided the link between the headquarter-level IMST and the WHO country offices to enable a methodical response both at the regional level and through technical support to countries in the Region. Since its establishment on 22 January 2020, the IMST has coordinated the COVID-19 response by providing strategic, operational and technical support to countries. Throughout 2020, the IMST consisted of 8 pillars, key technical and operational groups working together for increased regional collaboration, timely response and country support. Cross-cutting support functions enabled the smooth-running of the structure, as well as improved coordination and planning. In December 2020, the IMST structure was revisited to adapt to the evolving COVID-19 situation and response, including the addition of a COVID-19 vaccine pillar.
Coordination, leadership, strategic and technical guidance, surveillance, capacity-building, logistics, research, and innovation to adapt to the everchanging situation, were the main roles of the IMST. With over US$ 483 million mobilized for the regional COVID-19 response, the Regional Office had secured the highest funding and utilization of received funds of any WHO Regional Office. The Dubai Logistics Hub dispatched a record-breaking value of supplies in 2020 (US$ 58.9 million), serving as the largest repository of medical equipment and supplies in the world. Moreover, engaging in global efforts was one of IMST’s main achievements over the past year. For example, the involvement of 10 countries of the Region in the global Solidarity trial, and establishing 2 reference laboratories in the Region, were significant accomplishments. Despite pre-existing emergencies in the Region, the IMST scaled up the genetic sequencing capacity of SARS-CoV-2, the virus that causes COVID-19, to 14 countries in the midst of the pandemic.
Communicating effectively with WHO country offices, partners, communities and other stakeholders was an essential part of the response, including providing accurate and timely information to the general public especially regarding hygiene etiquette and how to fight the “infodemic”. External communication and risk communication and community engagement were also paired with technical guidance to countries on a regular basis and were tailored to the regional situation through interim guidance documents, review and assessment missions to countries (see below), training courses and webinars. In addition, the IMST developed technical tools to improve data management and analysis, including through interactive dashboards and modelling tools, to assist countries in implementing the most effective measures nationally and sub-nationally.
In order to strengthen its technical support to countries, the IMST deployed experts to conduct initial assessment missions in 8 countries and review and assessment missions of the COVID-19 response in 4 countries following that: Afghanistan, Pakistan, Tunisia, and Lebanon. The purpose of those missions was to identify and document strengths and areas for improvement while supporting ministries of health to review and assess their national COVID-19 response. Throughout the missions, experts reviewed background documents, engaged with key stakeholders and conducted several site visits. Technical and operational advice was given to stakeholders throughout, and recommendations were made in the context of the emergency response, and in terms of longer term health systems strengthening.
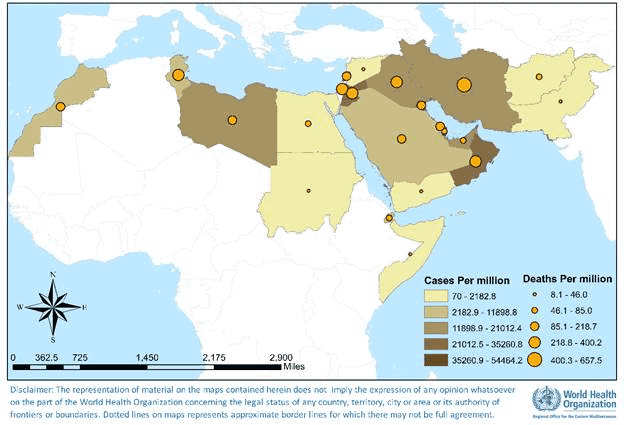
Fig. 22. Geographical distribution of COVID-19 cases and deaths per million reported from the Region, 29 January to 31 December 2020
Table 3. Infectious disease outbreaks reported from the countries of the Region in 2020
|
Disease |
Country |
First reported case |
Last reported case |
Total cases* |
Deaths |
CFR (%) |
|
Chickenpox (varicella) |
Pakistan |
January 2020 |
September 2020 |
235 |
0 |
- |
|
Chikungunya |
Sudan |
August 2020 |
November 2020 |
577 |
0 |
- |
|
Cholera |
Somalia |
January 2020 |
December 2020 |
6582 |
33 |
0.5 |
|
Yemen |
January 2020 |
December 2020 |
230 121 |
84 |
0.04 |
|
|
Crimean-Congo haemorrhagic fever |
Afghanistan |
January 2020 |
December 2020 |
184 |
15 |
8.2 |
|
Pakistan |
January 2020 |
August 2020 |
19 |
- |
- |
|
|
Dengue |
Yemen |
January 2020 |
December 2020 |
65 183 |
175 |
0.3 |
|
Pakistan |
August 2020 |
December 2020 |
125 794 |
10 |
0.01 |
|
|
Diphtheria |
Yemen |
January 2020 |
December 2020 |
1710 |
134 |
7.8 |
|
Extensively drug-resistant typhoid fever |
Pakistan |
January 2020 |
December 2020 |
3633 |
0 |
- |
|
Middle East respiratory syndrome |
Saudi Arabia |
January 2020 |
December 2020 |
60 |
20 |
33.3 |
|
Qatar |
February 2020 |
February 2020 |
01 |
- |
- |
|
|
Poliomyelitis (WPV1) |
Afghanistan |
January 2020 |
December 2020 |
56 |
- |
- |
|
Pakistan |
January 2020 |
December 2020 |
84 |
- |
- |
|
|
COVID-19 |
Afghanistan |
February 2020 |
December 2020 |
52 586 |
2211 |
4.2 |
|
Bahrain |
February 2020 |
December 2020 |
92 675 |
352 |
0.4 |
|
|
Djibouti |
March 2020 |
December 2020 |
5831 |
61 |
1.0 |
|
|
Egypt |
February 2020 |
December 2020 |
138 062 |
7631 |
5.5 |
|
|
Islamic Republic of Iran |
February 2020 |
December 2020 |
1 225 143 |
55 223 |
4.5 |
|
|
Iraq |
February 2020 |
December 2020 |
595 291 |
12 813 |
2.2 |
|
|
Jordan |
March 2020 |
December 2020 |
294 494 |
3834 |
1.3 |
|
|
Kuwait |
February 2020 |
December 2020 |
150 584 |
934 |
0.6 |
|
|
Lebanon |
February 2020 |
December 2020 |
181 503 |
1745 |
1.0 |
|
|
Libya |
March 2020 |
December 2020 |
100 744 |
1487 |
1.5 |
|
|
Morocco |
March 2020 |
December 2020 |
439 193 |
7388 |
1.7 |
|
|
occupied Palestinian territory |
March 2020 |
December 2020 |
155 365 |
1529 |
1.0 |
|
|
Oman |
February 2020 |
December 2020 |
128 867 |
1499 |
1.2 |
|
|
Pakistan |
February 2020 |
December 2020 |
482 178 |
10 176 |
2.1 |
|
|
Qatar |
February 2020 |
December 2020 |
143 834 |
245 |
0.2 |
|
|
Saudi Arabia |
March 2020 |
December 2020 |
362 741 |
6223 |
1.7 |
|
|
Somalia |
March 2020 |
December 2020 |
4714 |
130 |
2.8 |
|
|
Sudan |
March 2020 |
December 2020 |
25 730 |
1576 |
6.1 |
|
|
Syrian Arab Republic |
March 2020 |
December 2020 |
11 434 |
711 |
6.2 |
|
|
Tunisia |
March 2020 |
December 2020 |
140 557 |
4730 |
3.4 |
|
|
United Arab Emirates |
January 2020 |
December 2020 |
207 822 |
669 |
0.3 |
|
|
Yemen |
April 2020 |
December 2020 |
2103 |
611 |
29.1 |
Includes both suspected and laboratory-confirmed cases


