Infectious disease outbreaks reported in the Eastern Mediterranean Region in 2019
In 2019, WHO’s Eastern Mediterranean Region witnessed several new emerging infectious disease outbreaks caused by high threat pathogens. Failure to fully contain previous outbreaks also led to sporadic reporting of cases of other diseases in endemic patterns. Eight countries in the Region reported outbreaks, with over 2.3 million cases resulting in more than 5000 deaths.
Diseases that caused outbreaks within countries in 2019 included cholera, Crimean-Congo haemorrhagic fever (CCHF), chikungunya, chickenpox (Varicella), dengue fever, diphtheria, extensively drug-resistant (XDR) typhoid fever, human immunodeficiency virus (HIV), hepatitis A, measles, Middle East respiratory syndrome (MERS), poliomyelitis and Rift Valley fever (Fig. 1).
The likelihood of the emergence and rapid transmission of high-threat pathogens in the Region has increased in recent times. Many countries are directly or indirectly affected by acute and protracted humanitarian emergencies, leading to fragile health systems, as well as high numbers of internally displaced persons and refugees, who have little or no access to basic health care services and environmental infrastructure.
Other risk factors for infectious disease outbreaks include rapid or unplanned urbanization, climate change, increased human-animal interaction, weak surveillance and limited laboratory diagnostic capacity, poor infection prevention and control measures in health facilities, and insufficient risk communication and community engagement efforts.
The Regional Office for the Eastern Mediterranean provides technical support to affected countries to contain outbreaks through the application of appropriate science-based public health control measures. The WHO Regional Office maintains epidemiological data received from country offices and ministries of health on major outbreaks through its central database ‒ the Outbreak and Public Health Event Portal (OPHEP). This portal monitors outbreak trends in the Region and the progress of response measures.
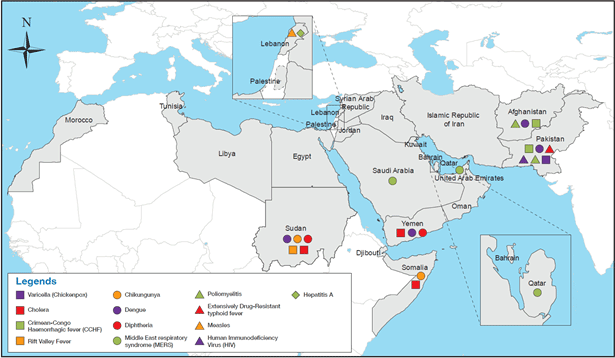
Fig 1. Countries of WHO Eastern Mediterranean Region reporting infectious disease outbreaks in 2019
Multiple challenges were faced by countries, WHO and other partners in responding to these emerging and re-emerging infectious disease outbreaks. Most significantly, the majority of outbreak-affected countries were experiencing protracted or acute emergencies with disrupted or under-performing health systems, such as Somalia, Sudan and Yemen. In other countries like Afghanistan and Pakistan, financial and capacity issues limited health system performance.
The prolonged insecurity and inaccessibility in emergency settings (such as Iraq, Somalia, Syria and Yemen) usually resulted in delayed implementation of key planned activities and under-utilization of committed funding, potentially leading to the spread of high-threat diseases to other areas. The high frequency of natural disasters (such as floods, droughts and heavy rains) was another major challenge, aggravating the existing situation and increasing the number of cases. With persistent demand from countries for more technical, logistic and financial support to tackle the outbreaks, it was sometimes difficult to meet the need for resources, technical staff and supplies.
Another challenge was the lack of integrated response plans within affected countries, with fragmented efforts to deal with the specific outbreaks. Some outbreaks required the involvement of multiple ministries for infrastructure development (such as clean water supply, sanitation and disaster preparedness) and delayed construction activities. Lack of public awareness on prevention of common diseases such as cholera and vector-borne diseases contributed to the rapid spread of these outbreaks.
This report recommends the following:
Governments and stakeholders should be engaged, allowing partners and donor organizations to gain access to affected areas and provide essential health services. Continuous engagement with external donors by sharing activities and objectives will encourage pooling of resources and division of responsibilities, thus avoiding wastage and duplication. Furthermore, where WHO does not have direct access, local partners should be engaged to provide logistical support within country.
Comprehensive joint strategies should be developed in coordination with government and external partners to enable coordinated responses and pooling of resources. Countries facing multiple vector-related outbreaks should develop integrated plans for optimal use of resources and simultaneous control. Countries facing repeated waterborne outbreaks should update or develop comprehensive national cholera control plans aligned with “Ending cholera: a global roadmap to 2030”.
Regular evaluations (external, internal and joint) should be conducted to assess the impact of activities and find and correct gaps. Prioritization of issues should be based on threat perception and sensitivity, with resources allocated accordingly. New efficient tools should be developed and adapted for capacity-building in case diagnosis, investigation and prevention.
Specific efforts are required to:
strengthen infectious disease surveillance systems;
improve diagnostic capacities and laboratory systems;
strengthen rapid response capabilities for more timely response and containment;
conduct operational research on high-threat infectious diseases in order to improve preparedness, particularly studies on the burden of disease, modelling and forecasting.
Disease outbreaks responded to in 2019 by country
1. Chickenpox (Varicella)
Pakistan
Since April 2017, Pakistan has faced a significant upsurge in reported chickenpox (Varicella) cases and up until December 2019, a total of 18 883 cases with 21 related deaths (case-fatality rate 0.11%) were reported. Between January and December 2019, a total of 1285 cases of chickenpox, with no deaths were reported in Punjab province (Fig. 2). The outbreak has not yet been fully contained. A higher number of cases were reported during the summer months of each year (2017‒2019) but sporadic cases continued to be reported until the end of the year.
WHO is providing support to countries in disease surveillance and laboratory confirmation of suspected cases, mapping of hotspots, risk communication, promoting routine EPI vaccination, and sharing guidelines for case management to reduce morbidity and mortality from disease.
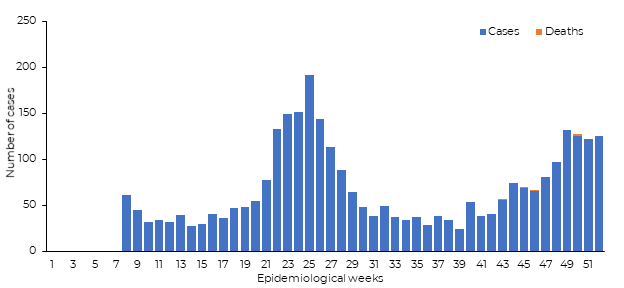
Fig 2. Number of suspected chickenpox cases reported in 2019, Punjab, Pakistan
2. Chikungunya
Sudan
Since Week 38, 2019 (September 15‒21) Sudan reported 281 cases with 5 associated deaths from 10 states (Table 1). The most affected states were West Darfur (224 cases), East Darfur (24 cases) and South Darfur (23 cases). The samples were laboratory-confirmed both by rt-PCR and serology. Sudan reported its first ever outbreak of chikungunya in 2018 (48 763 cases, 0 deaths) and the number of cases in 2019 outbreak are far fewer as compared to last year, which is due to implementation of better surveillance and response measures (Fig. 3).
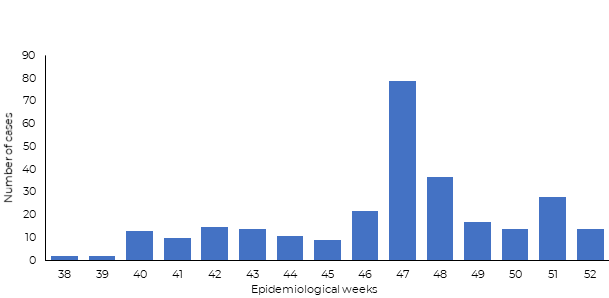
Fig 3. Number of chikungunya cases reported in Sudan during 2019
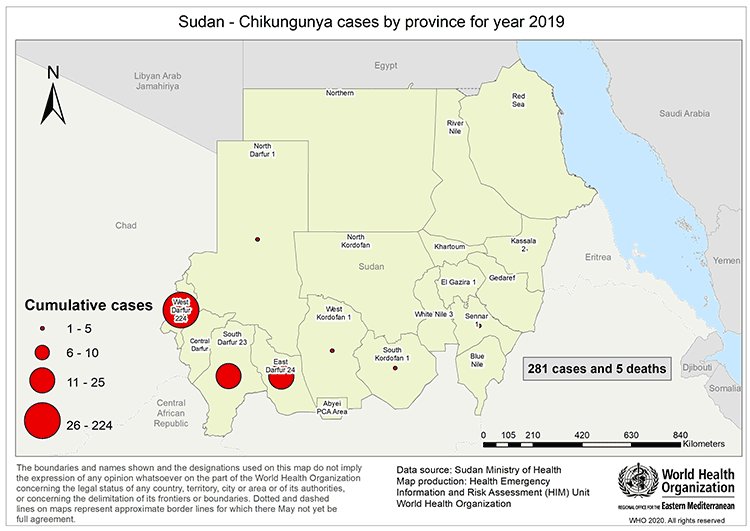
Fig 4. Geographical distribution of chikungunya cases reported in 2019 (Week 38‒52), Sudan
WHO provided support to the Ministry of Health in disease surveillance, capacity-building for laboratory confirmation of suspected cases and provision of testing kits, health awareness and risk communication materials and funding for vector control activities, such as larvae control, adult control, spraying and fogging, and provision of mosquito nets. WHO also provided support for deployment of one laboratory expert (October 2019) and two epidemiologists (October and November 2019) to strengthen laboratory capacity at central and state level for confirmation of suspected cases of emerging infectious diseases as well as to strengthen epidemiologic and data management capacity for field investigation. Further, experts from the Regional Office were deployed on a rotational basis to build capacity at country level.
3. Cholera
Somalia
Cholera is an endemic disease in Somalia. Since December 2017, when first cholera cases were laboratory-confirmed in Beletweyne district of the Hiraan region following heavy rains, the outbreak spread to 27 districts in four regions located in the river basins in Jubba and Shabelle. No case was reported from Week 1 to 7 (2019) due to the closure of the main cholera treatment centre from which the data were collected. During 2019 (January to December), a total of 3100 suspected cases of cholera, including 4 deaths, were reported (case-fatality rate 0.13). The cumulative number of suspected cases reported since December 2017 are 9681, including 50 deaths (case-fatality rate 0.52%). Of 983 stool samples that were tested at the National Public Health Laboratory in Mogadishu since the start of the outbreak, a total of 222 samples tested positive for Vibrio cholerae, serotype O1 Ogawa (Fig. 5). The outbreak has not yet levelled off fully and with recent floods in October 2019, the number of reported cases increased since Week 44 in 2019.
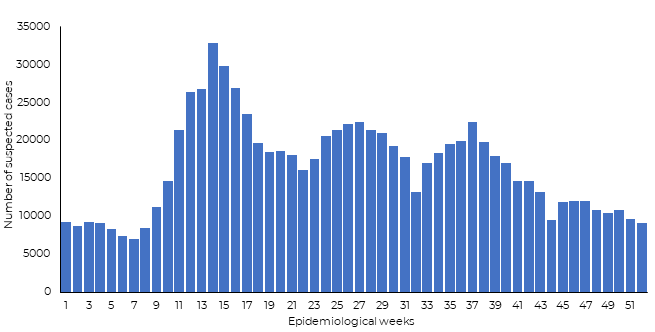
Fig. 5 Suspected cholera cases reported in Somalia during 2019
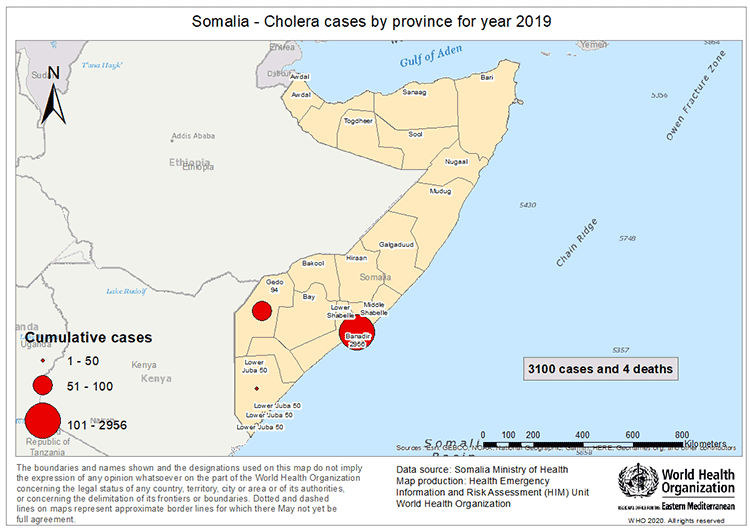
Fig. 6 Geographical distribution of suspected cholera cases reported from Somalia in 2019
WHO has supported the Government of Somalia since the start of the outbreak in 2017. Overall reduction in the number of new cholera cases as compared to the cases at the beginning is attributed to enhanced implementation of preventive interventions including oral cholera vaccination, distribution of risk communication materials and the strengthening of water, sanitation and hygiene (WaSH) activities in hotspots. Disease surveillance is being managed with the support of WHO through an electronic system known as the Early Warning Alert and Response Network (EWARN). WHO and the Ministry of Health continuously monitored outbreak trends through EWARN to promptly investigate and respond to all alerts.
Sudan
The Ministry of Health of Sudan declared a cholera outbreak on 8 September 2019 (Epi Week 37) and reported the first case from El Rosaires locality of Blue Nile State. A total of 346 cases, including 11 deaths, were reported in 2019 (case-fatality rate 3.18%). More than 95% of all the cases were reported from two states; Blue Nile (204) and Sennar (130). The 11 deaths were reported from these two states as well. But due to better surveillance and response measures in place, the outbreak was controlled within record time and only sporadic cases were reported from Week 44 onward. The last suspected cases were reported on 16 December 2019; these were negative (Fig. 7).
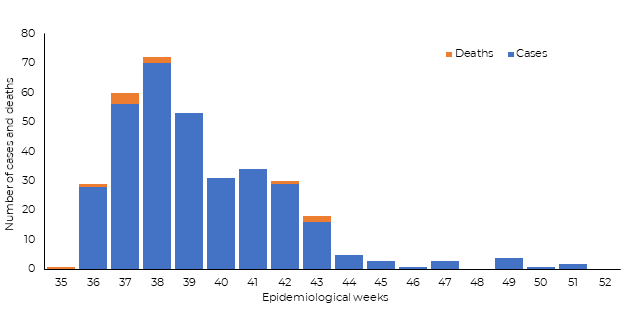
Fig. 7 Susspected cholera cases and deaths reported in Sudan in 2019
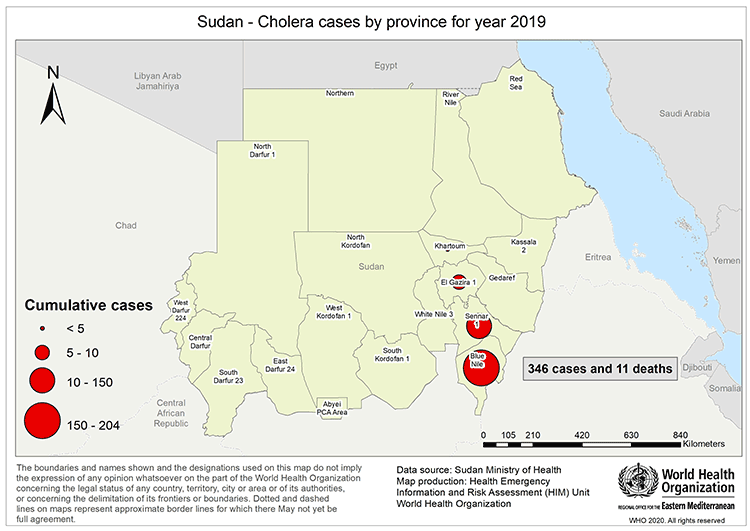
Fig. 8 Geographical distribution of suspected cholera cases reported from Sudan in 2019
WHO supported the Ministry of Health in implementation of WaSH activities and two rounds of an oral cholera vaccination campaign during October and November to vaccinate target populations in the most affected states (Blue Nile State (coverage 85%), Sennar (coverage 98%). WHO also provided regular support to health authorities for laboratory confirmation of suspected cases and in sustained implementation of WaSH activities for long-term prevention and control.
Yemen
The cholera outbreak reported in Yemen, since October 2016 continued in year 2019 as well. This ongoing outbreak affected the whole country, and although the trend was on the decline at the beginning of the year in 2019, the number of cases continued to increase from Week 8 and reached a peak in Week 14. They started declining after that but the number of cases reported each Week were still relatively high. The cumulative number of suspected cholera cases reported from January to December in 2019 were 861 096 with 1025 deaths (case-fatality rate 0.12%). Since January 2019 a total of 10 005 samples were tested at the central public health laboratories, out of which 5371 were confirmed as cholera-positive by culture (Fig. 9).
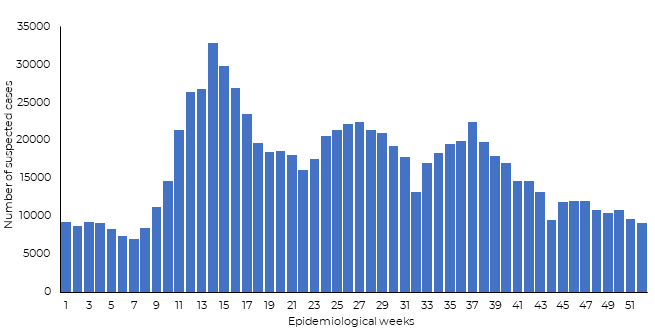
Fig. 9 Suspected cholera cases reported in Yemen in 2019
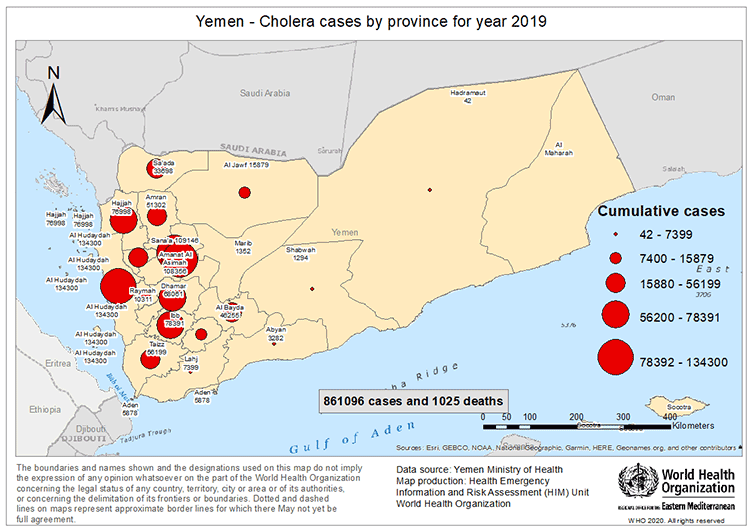
Fig. 10 Geographical distribution of suspected cholera cases reported from Yemen in 2019
The health system in Yemen is severely weakened due to ongoing conflict. WHO is supporting the Ministry of Health in multiple ways, including enhancing disease surveillance through EWARN, providing testing kits (rapid diagnostic and laboratory), mapping hotspot areas, implementing WaSH activities, administering oral cholera vaccination to high-risk populations, providing supportive drugs and conducting case management training.
In 2019 support was also provided to deploy 10 experts for cholera case management, laboratory investigation, oral cholera vaccination campaigns and electronic Disease Early Warning System (eDEWS) surveillance. However, the outbreak is still not well contained due to the complexity of the situation, including lack of infrastructure, limited resources and inadequate staffing.
4. Crimean-Congo haemorrhagic fever (CCHF)
Afghanistan
CCHF is endemic in Afghanistan, and an upsurge of reported cases was reported in 2017 and 2018. The number of reported cases continued to be high throughout 2019 and peaked during the month of August (Fig. 11). From January to December 2019, a total of 583 suspected cases, including 63 associated deaths (case-fatality rate 10.81%) were reported in Afghanistan. The majority of the cases were reported from Herat and Kabul provinces. The increase in the number of cases seen in recent years was mainly due to better surveillance and reporting mechanism.
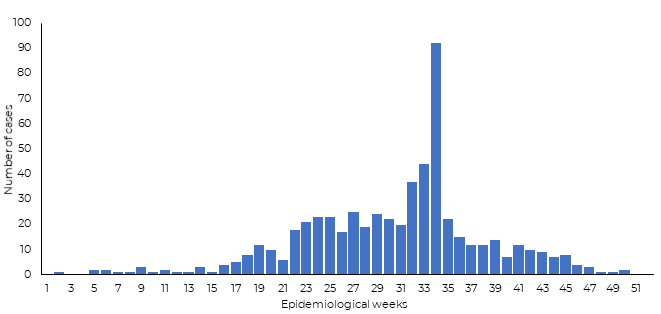
Fig. 11 Suspected cases of CCHF reported in Afghanistan in 2019
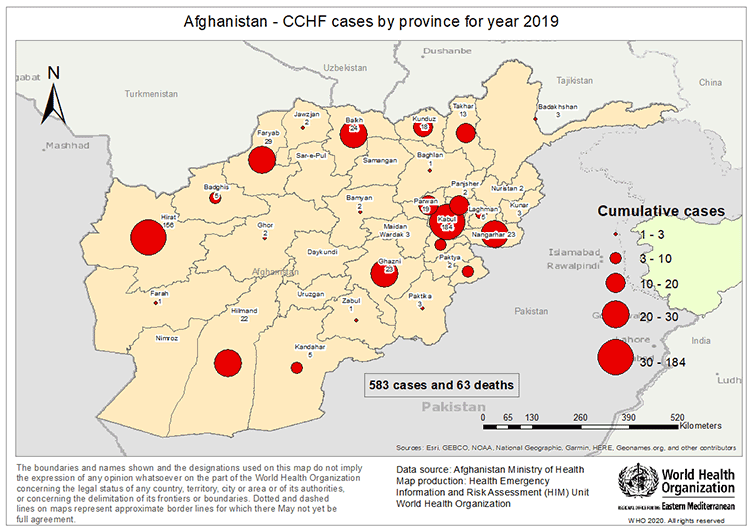
Fig. 12 Geographical distribution of CCHF cases and related deaths reported from Afghanistan in 2019
WHO supported the Ministry of Health of Afghanistan in enhancing coordination among involved sectors for an integrated response to control the outbreak. The surveillance mechanism was enhanced to report all suspected cases on a daily basis and information, education and communication materials were distributed to high-risk areas to raise awareness about prevention and control measures. WHO also extended support through rapid response team training focused on CCHF and in drafting an operational plan to accelerate the response.
Pakistan
CCHF also remains an endemic disease in Pakistan. During the last few years, the country has encountered a number of outbreaks. Initially, CCHF cases were reported from its established foci, such as Balochistan, and but now it is reported from other provinces/areas. The frequent unmonitored movement of animals and animal products remained the major cause of the spread of the virus throughout the country. From January to December 2019, a total of 75 suspected cases with 9 associated deaths (case-fatality rate 12%) were reported throughout the country (Fig. 13).
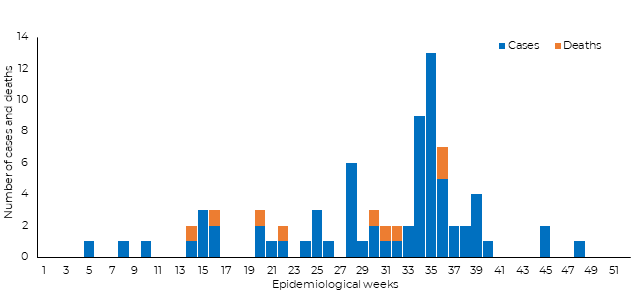
Fig. 13 Suspected and laboratory-confirmed CCHF cases and deaths from Pakistan in 2019
WHO extended support to the country for enhancing coordination in detecting CCHF, as well as conducting capacity-building for laboratory confirmation of suspected cases. Laboratory kits and training were provided to the central laboratory. Gaps were identified in surveillance and response measures during periodic reviews and WHO is engaged with the Government in strengthening the existing measures currently in place.
5. Dengue fever
Pakistan
Pakistan has been experiencing outbreaks of dengue fever for the past several years, affecting different parts of the country on a regular basis. The main vector of dengue virus transmission, Aedes aegypti is well established in all parts of the country. In August 2019 the country initially reported a huge number of dengue cases from the twin cities (Islamabad and Rawalpindi) but within Weeks the outbreak had spread all over the country. By the end of 2019, a total of 54 079 confirmed dengue fever cases with 95 associated deaths (case-fatality rate 0.18%) were reported all over the country, except Gilgit Baltistan. Thirty-one percent (31%) of the total cases this year were reported from Sindh province.
Compared to previous dengue outbreaks from the country, the number of deaths were the highest this time. The epidemic reached its peak during the month of October (2019) but the number of reported cases started declining from early November in all parts of the country, except Sindh province (Fig. 14).
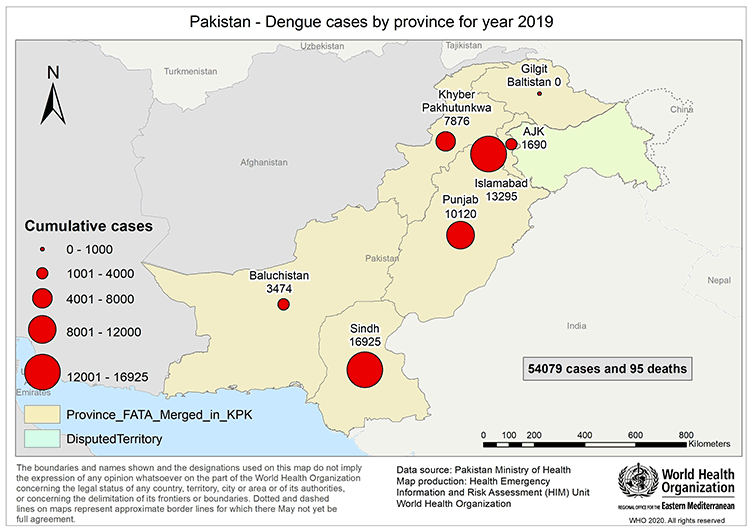
Fig. 14 Geographical distribution of confirmed dengue fever cases reported from Pakistan in 2019
WHO supported the government with provision of case diagnosis and management guidelines throughout the country. Information, education and communication materials were distributed to raise awareness of the general public on prevention measures through source reduction and preventive measures. WHO also provided support by deploying 5 experts (2019) for dengue case management, laboratory investigation and emergency risk communication. Support was also provided to the Government in timely arrangement of medical supplies for severe case management (fluids, crystalloids etc.). Due to the concerted efforts of WHO and the Ministry of Health, the outbreak was contained quickly in almost all parts of the country and plans are already under way to prepare for the next season to better control the disease.
Sudan
The Federal Ministry of Health of Sudan declared an official dengue outbreak in Kassala State after cases were first confirmed in epidemiological Week 31 (July 28‒August 3) and then it spread to nine other states. From the onset of the outbreak until December 2019, the country reported 4205 dengue cases with 13 associated deaths (case-fatality rate 0.31%). The majority of the cases (94%) were from Kassala State (3953,). The epidemic reached its peak during Week 46 (761 cases) and then gradually started to taper off. However, cases were continuously reported until the end of 2019. Out of 207 samples, 79 tested positive for dengue virus. Out of the total reported cases 306 cases (7.2%) presented with bleeding symptoms and more than 59% of them reported with nasal bleeding (Fig. 15).
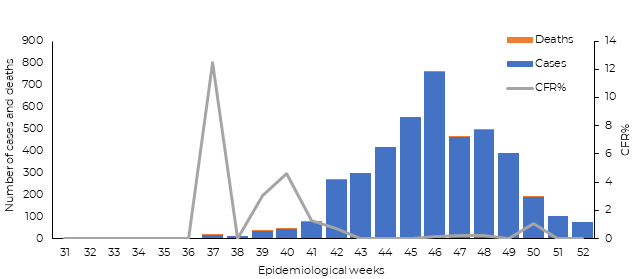
Fig. 15 Dengue fever cases, deaths and case-fatality rate reported from Sudan in 2019
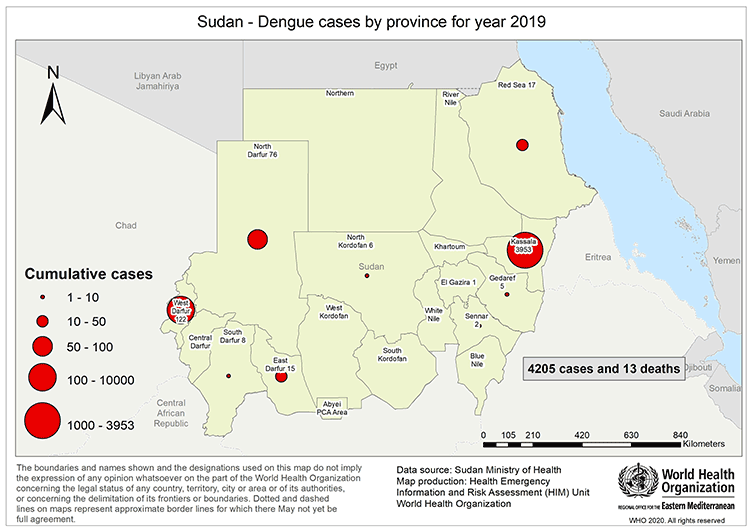
Fig. 16 Geographical distribution of dengue fever cases reported from Sudan in 2019
Sudan is facing multiple arboviral disease outbreaks and the Government is taking all out measures to launch integrated vector control activities to combat all related outbreaks in collaboration with WHO. WHO is providing technical, financial and logistical support to Sudan to overcome the challenges in controlling vector-borne outbreaks. Several experts (epidemiologists, laboratory specialists, clinicians, entomologists) were deployed by WHO to support the Government in case diagnosis, management, mapping of hotspot areas, as well as vector surveillance and control measures. Funding is also being provided for vector control activities and arrangements of medicines and insecticides.
Yemen
A dengue fever outbreak was reported from Yemen in January 2018 from Shabwah governorate. The outbreak continued throughout 2018 and into 2019. From January to December 2019, a total of 71 688 cases, including 258 deaths (case-fatality rate 0.36%), were reported across the country. In total 794 (IgG) and 590 (IgM) cases were confirmed by Elisa at the National Center for Public Health Laboratories. Owing to the presence of Aedes mosquitoes in the country and heavy rains during October and November (2019), the number of reported cases increased exponentially during last 6 weeks of 2019. The total cases reported during last 6 weeks were greater than those reported from January to mid-November (Fig. 17).
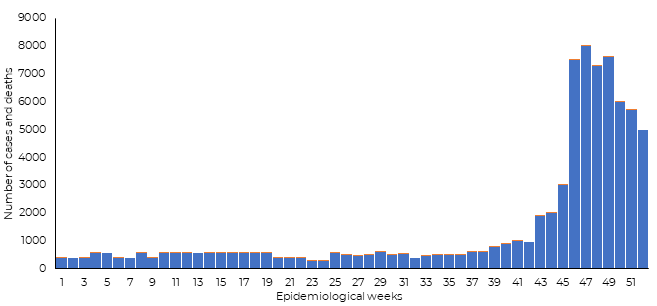
Fig. 17 Dengue fever cases and deaths reported from Yemen in 2019
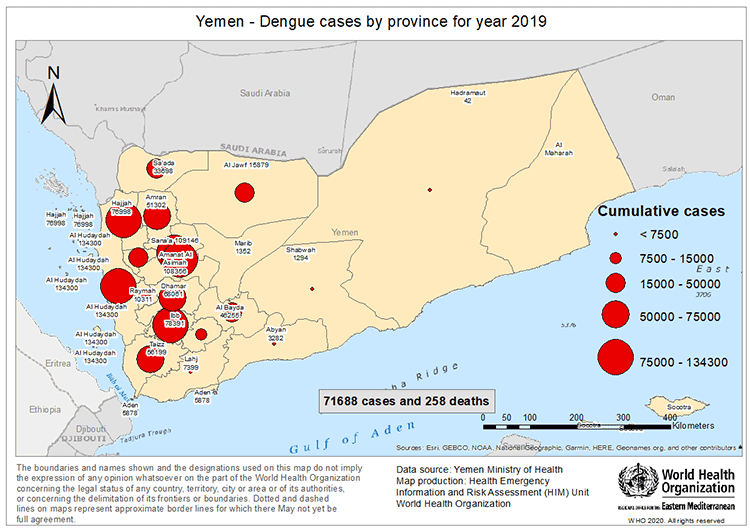
Fig. 18 Geographical distribution of dengue fever cases reported from Yemen in 2019
WHO is supporting the Government in conducting disease surveillance through eDEWS due to disruption of the routine surveillance system. Further, regular technical and financial support is being extended for case diagnosis, management and vector control activities. Efforts are under way to strengthen the surveillance system for better case diagnosis, as well as mapping of hotspot areas for targeted campaigns to control the outbreak. Regular contact is being made with other international partners working in the country for integrated response and optimal resource utilization.
6. Diphtheria
Sudan
In November 2019, Sudan started reporting an unusually high number of suspected cases of diphtheria that caused concern among public health experts who were then mobilized for timely response for effective case management and prevention measures.
According to epidemiological and EPI data, the first case was reported on 5 February 2019 but the cases were sporadic until October 2019 (only 12 cases). Afterwards an outbreak was reported from Al-Santa locality of South Darfur state and spread to other states. Up until December 2019 a total of 93 suspected cases with 13 associated deaths were reported from 6 different states (case-fatality rate 13.98%). The majority of cases were from South Darfur State with more than 98% cases in Al-Sunta locality, which borders South Sudan. Of the cases reported 82% of people had not been vaccinated and the most affected age group was 5‒14 years old (63.2% cases). Only one case was laboratory confirmed and the rest of the cases were clinically confirmed, this was due to lack of laboratory reagents for PCR and culture (Fig. 19).
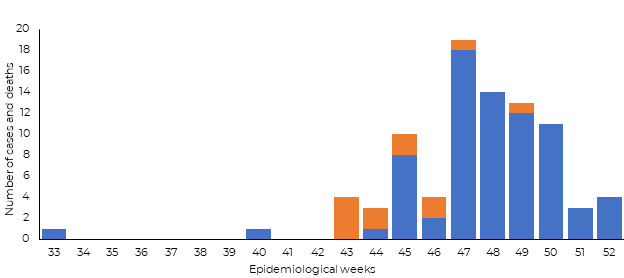
Fig. 19 Diphtheria cases and deaths reported in Sudan in 2019
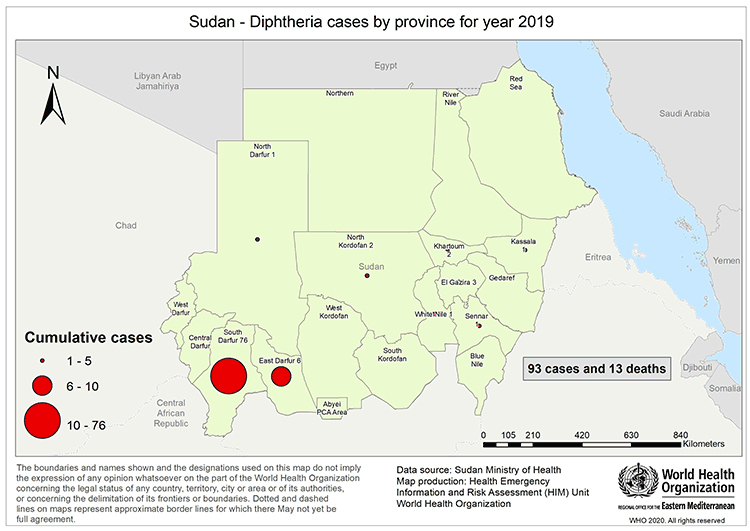
Fig. 20 Geographical distribution of diphtheria cases reported from Sudan in 2019
In response, WHO provided 200 DAT doses to Sudan to manage the most severe cases. Furthermore, WHO joined a joint mission with the Federal Ministry of Health to conduct a field survey in the third Week of November 2019 in the most affected locality to identify the possible causes and devise a response strategy. WHO also supported the authorities by providing case management guidelines to reduce morbidity and mortality and strengthen the immunization activities to control the outbreak. Two vaccination drives were conducted in Al Sunta locality; for children aged 1‒7 years old Penta vaccine was administered and DT vaccine for 7‒15 year olds.
Yemen
In October 2017, Yemen began experiencing an outbreak of diphtheria that spread to most of the districts in 23 governorates. By December 2019, a total of 5055 suspected cases were reported with 299 related deaths (case-fatality rate 5.92%), including 501 laboratory-confirmed cases of diphtheria. From January to December 2019 a total of 2020 cases were reported with 129 associated deaths (case-fatality rate 6.39%). In 2019, the most affected age group was 6‒10 years olds (26%) followed by 11‒15 year olds (20%). In 2019, the majority of the cases reported were from Hudaydah governorate (Fig. 21).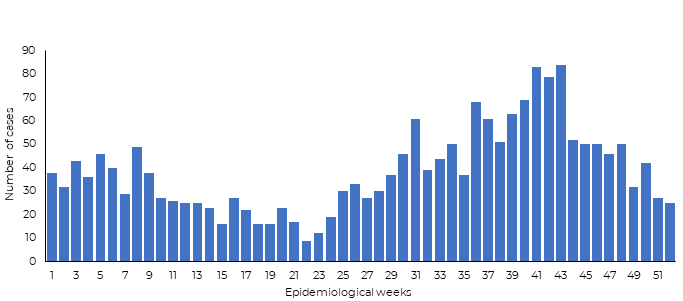
Fig. 21 Diphtheria cases reported in Yemen in 2019
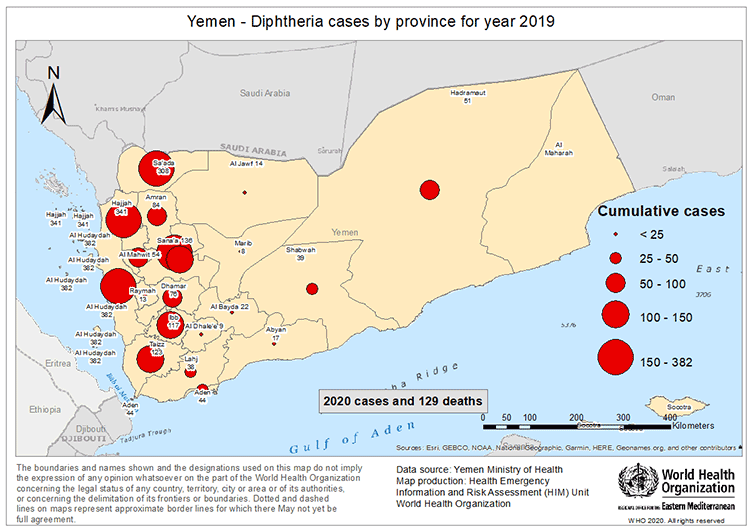
Fig. 22 Geographical distribution of diphtheria cases reported from Yemen in 2019
WHO provided support to the local health authorities in disease surveillance and laboratory confirmation of suspected cases through provision of logistical and technical resources. Further, in addition to routine immunization activities, supplementary immunization campaigns were conducted to protect the people at high risk for diphtheria. During 2019, two targeted immunization campaigns in high-risk governorates were held to boost the number of immunized children and Penta vaccine was administered to children from 6 weeks to 5 years old and TD was administered to children 5‒15 years old.
7. Extensively drug-resistant typhoid fever
Pakistan
Since November 2016, Pakistan has reported cases of extensively drug-resistant typhoid fever (XDR). Cases were first detected in a district called Hyderabad of Sindh province. Afterwards, cases continued to be reported from other districts of Sindh province. However, most of the reported cases (72%) are from Karachi district of Sindh province (Fig. 23). Up until December 2019 a total of 15 217 cases of XDR typhoid fever were reported from different districts of Sindh province (Table 1) out of which 9731 cases were reported from January to December 2019.
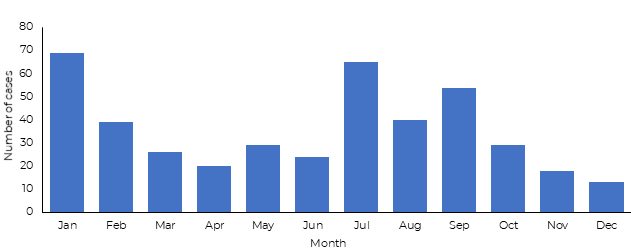
Fig. 23 Extensively drug-resistant typhoid fever cases reported in Karachi (Pakistan) in 2019
Table 1. Extensively drug-resistant typhoid fever cases reported from December 2016 to December 2019, Sindh, Pakistan
|
Year |
Karachi |
Hyderabad |
Other districts |
Total |
|
2016 |
0 |
12 |
0 |
12 |
|
2017 |
175 |
485 |
4 |
664 |
|
2018 |
3712 |
891 |
207 |
4810 |
|
2019 |
7088 |
1645 |
998 |
9731 |
|
Grand Total |
10 975 |
3033 |
1209 |
15 217 |
The number of suspected cases of extensive drug resistance typhoid reported increased during each successive year (only one province, Sindh, reported cases). WHO extended support for laboratory confirmation of suspected cases and preparation of case management guidelines for confirmed cases. Pakistan became the first country in the world to introduce the WHO-approved typhoid conjugate vaccine in its Expanded Programme on Immunization on 18 November 2019 and more than 9.5 million children aged 9 months to 15 years were vaccinated until November 30 and the coverage was 90%.
8. Hepatitis A
Lebanon
Lebanon reported a hepatitis A outbreak from Rachidiyi camp (Palestine refugees camp in South Lebanon), which started during Week 35 (25‒31 August 2019) as one case was reported during that week. Later it reached a peak in Week 36 (27 cases), Week 37 (24 cases) and started to decline in Week 38 (12 cases) in Rachidiyi camp. Later it was also reported from two other camps (Burj Shamali at 13 cases and El Buss at one case) and other residential areas of Lebanon (among local people). Up until the end of December 2019, a total of 426 hepatitis A cases were reported from Lebanon, including refugee camps. The most affected age groups were 5‒9 and 10‒19 years old (Fig. 24).
Fig. 24 Hepititis A cases reported from Lebanon in 2019
WHO is extending continuous support to the Ministry of Public Health of Lebanon in surveillance and confirmation of suspected cases, as well as testing the water samples for contamination with virus. Awareness-raising campaigns were conducted to sensitize parents about the safety of water and support for water chlorination at schools was also extended to protect high-risk age groups.
9. HIV/AIDS
Pakistan
Pakistan declared a HIV outbreak on 25 April 2019 in the Ratodero area of the district Larkana, where initially a number of children were reported HIV-positive from one locality after screening. By the end of December 2019, a total of 38 366 people were screened for HIV in Ratodero locality, of whom 1228 tested positive for HIV (3.2%) and around 80% were children aged under 11 years. A total of 1306 patients were registered at ART centres (ART Centre, Sheikh Zayed Children’s Hospital, Larkana, ART Centre at THQ Hospital Ratodero, and Adult ART centre, civil hospital, Larkana) and 1258 were receiving antiretroviral drugs. These also included 17 children born to HIV-positive mothers and put on prophylaxis to prevent mother-to-child transmission. The outbreak is still ongoing and each week new cases are reported during screening (Fig. 25).
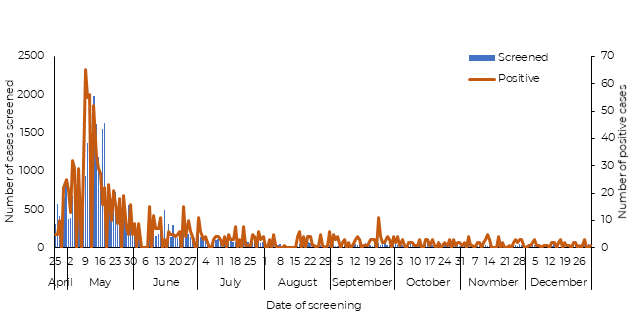
Fig. 25 Number of HIV cases screened and positive in Ratodero, Pakistan in 2019
Immediately after report of initial cases from the locality, WHO coordinated with the Ministry of National Health Services, Regulations and Coordination and arranged WHO pre-qualified screening kits and arranged funds for provision of ARVs in the local centres for HIV-positive individuals. WHO supported the deployment of 25 experts in 2019 to provide support for the HIV outbreak (Larkana district, Sindh province) for HIV care, laboratory support, infection prevention and control, blood safety, outbreak investigation and case-control study. Collaboration was undertaken with other donors to arrange laboratory testing equipment and establishment of HIV treatment centres at local hospitals to provide treatment to positive cases. In addition, a WHO expert mission provided clinicians and technical staff with “hands-on training” at adult, paediatric and prevention of mother-to-child transmission clinics. Communication materials were distributed to raise awareness and urge people to practise safe behaviours. Response measures are still under way, and efforts are being made to control its spread to others in the locality and outside through education and awareness campaigns, improved infection prevention and control measures and establishment of treatment centres.
10. Measles
Lebanon
Since January 2019, Lebanon has reported 1067 cases of measles, with no associated deaths. 58% of the total cases were laboratory confirmed and 42% clinically confirmed. Lebanon’s Ministry of Public Health categorized the disease in inter-epidemic stage and most affected age groups are under 5 and 5‒9 years old. The measles vaccination coverage is very diverse in different areas. For children aged 1‒9 years old, 29% received at least one dose of vaccine (Fig. 26).
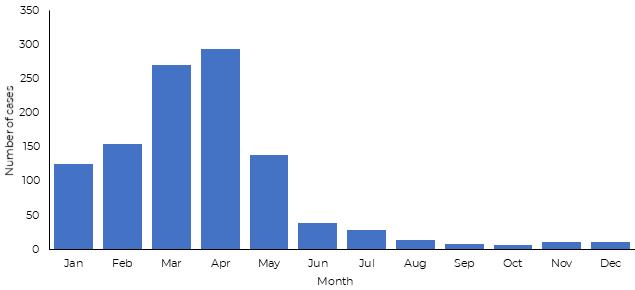
Fig. 26 Measles cases reported from Lebanon in 2019
The re-emergence of this vaccine-preventable disease is an alarming sign and necessitates to re-focus on improving routine immunization coverage, as well as conducting targeted immunization campaigns for better control of these diseases. WHO is extending support to the Ministry for enhanced epidemiologic surveillance and investigation and social mobilization to sensitize people about importance of vaccines for protection of their children. Furthermore, supplementary immunization campaigns were conducted in various high-risk areas to target unvaccinated children. The latest such campaign was launched on 6 December 2019 in three high-risk governorates to target all children between 6 months to 9 years of age, irrespective of their previous vaccination status and nationality, to control the spread of disease.
11. Middle East respiratory syndrome (MERS)
Saudi Arabia, Oman, United Arab Emirates and Qatar
MERS cases continued to be reported sporadically throughout 2019 especially from Saudi Arabia. In 2019, a total of 223 laboratory laboratory-confirmed cases of MERS were reported as compared to 147 (2018), 250 (2017), 249 (2016), and 492 (2015). Of these total cases reported in 2019, Saudi Arabia reported 205 cases. Other countries that reported laboratory-confirmed cases of MERS in 2019 are Oman (13 cases), United Arab Emirates (2 cases) and Qatar (3 cases) (Fig. 27).
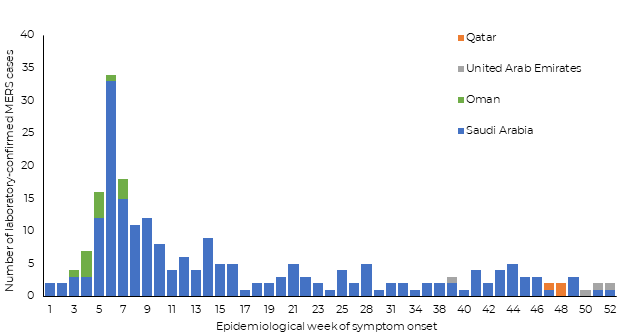
Fig. 27 MERS cases reported in the Region by week of symptom onset, 2019
MERS hospital and household clusters reported in 2019
In 2019, 2 nosocomial outbreaks of MERS were reported from Saudi Arabia (Table 2). A total of 61 laboratory-confirmed cases with 8 associated deaths were reported from one hospital outbreak (Fig. 28) and 13 cases with 6 associated deaths were reported from another hospital (Fig. 29). Additionally, two non-linked clusters of cases were reported from Oman with a total of 13 cases and 4 associated deaths (Fig. 30).
Table 2. MERS hospital outbreaks reported in 2019
|
Outbreak |
Date of first reported case |
Date of last reported case |
Total cases |
Died |
CFR% |
HCW |
Asymptomatic |
|
Wadi Al-Dawasir |
29 January 2019 |
12 March 2019 |
61 |
8 |
13.1 |
14 |
6 |
|
Al-Khafji |
29 March 2019 |
17 April 2019 |
13 |
6 |
46.1 |
5 |
3 |
|
North Batinah |
27 January 2019 |
18 February 2019 |
9 |
2 |
22.2 |
1 |
3 |
|
South Sharquia |
12 February 2019 |
14 February 2019 |
4 |
2 |
50 |
1 |
4 |
|
Grand Total |
74 |
14 |
19 |
9 |
|||
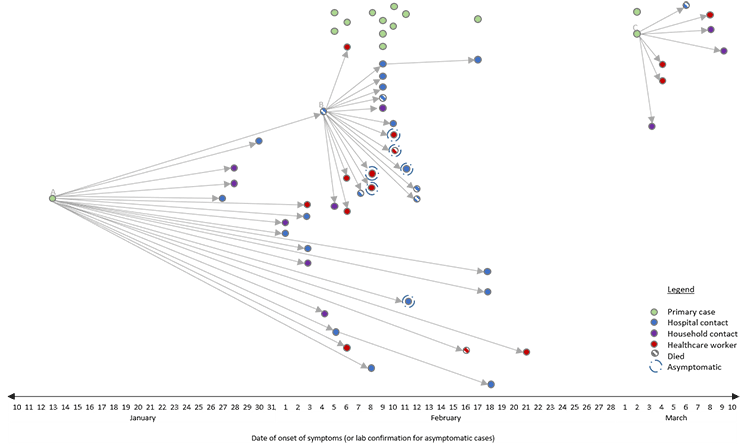
Figure 28. Transmission chain of Wadi Aldawaser outbreak, Saudi Arabia, 2019
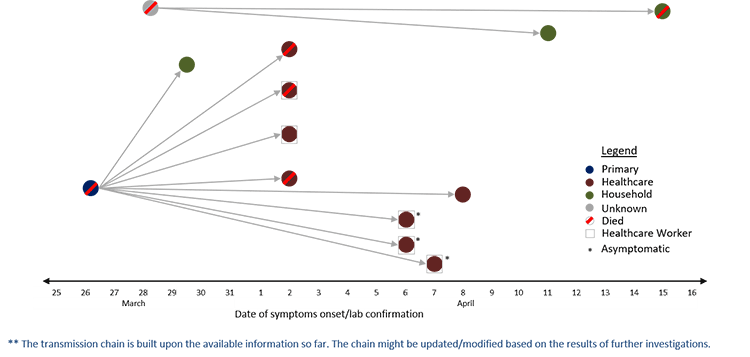
Figure 29. Transmission chain of Al-Khafji outbreak, Saudi Arabia, 2019
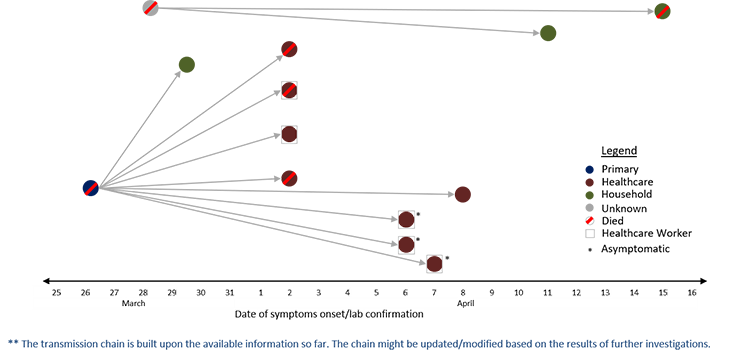
Fig. 30 Transmission chain of non-linked clusters reported from Oman, 2019
12. Poliomyelitis
Polio is the second vaccine-preventable disease that the world is hoping to eradicate in the near future. On World Polio Day 2019 (October 24) it was announced that wild poliovirus (WPV) type 3 was also eradicated from all over the world after eradication of WPV type 2 in 2015. But two countries (Afghanistan and Pakistan) are still reporting continuous transmission of the disease and the global community is providing support to help these last two neighbouring countries eradicate this disease. Now only cases of WPV1 are being reported by these two endemic countries.
Afghanistan
In 2019 a total of 29 WPV1 cases were reported. They include 9 cases from Uruzgan province, 5 cases from Hilmand province, 6 from Kandahar province, 2 each from Paktika and Farah provinces and 1 each from Kunar, Nangarhar, Badghis, Baghlan and Herat provinces (Fig. 31).
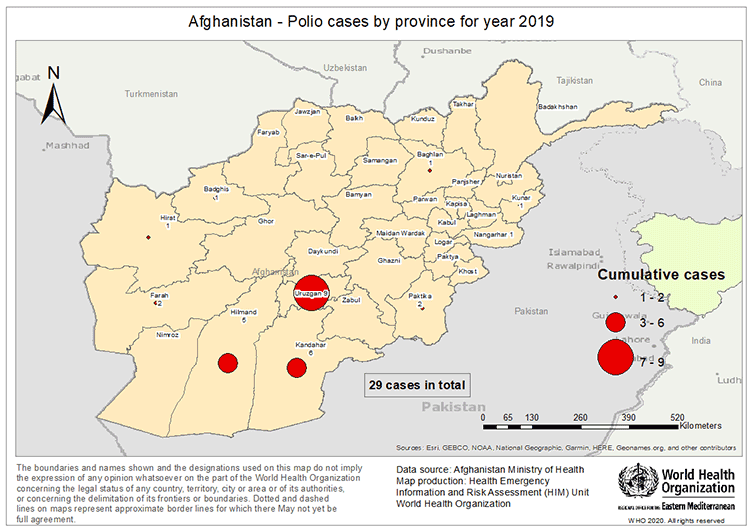
Fig. 31 Geographical distribution of poliomyelitis (WPV1) cases reported from Afghanistan in 2019
Pakistan
In 2019 a total of 144 WPV1 cases were reported from Pakistan. They included 80 from Khyber Pakhtunkhwa (KP) province, 12 from KP Tribal Districts (KPTD), 30 from Sindh province, 12 from Balochistan province and 10 from Punjab province. While in 2020, 12 WPV1 cases are reported, 6 from KP, 5 from Sindh and 1 from Balochistan provinces (Fig. 32).
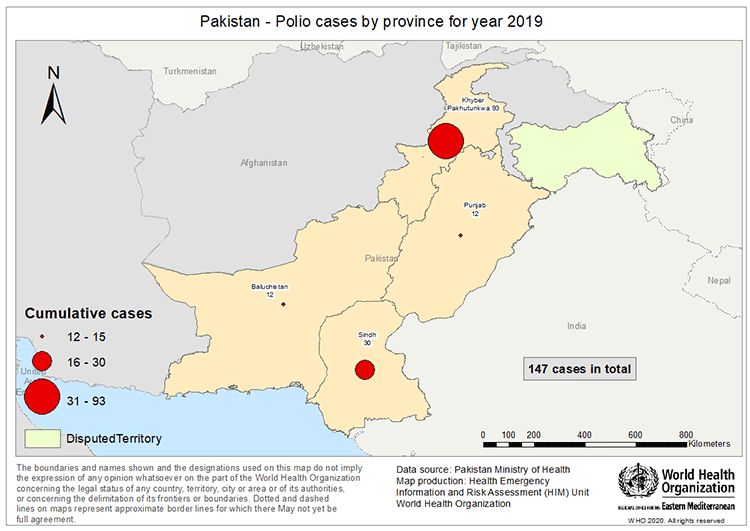
Fig. 32 Geographical distribution of poliomyelitis (WPV1) cases reported from Pakistan in 2019
Circulating vaccine-derived poliovirus-2 (cVDPV) cases
In 2019 a total of 22 cVDPV2 cases were reported. Cases included 4 from Diamir district of Gilgit-Baltistan (GB) province; 3 each from Torghar, Khyber and Mohmand; 2 from Kohistan Lower; and one each from Charsadda, Kohistan Upper, Bajour, Lakki Marwat and Peshawar districts in KP; one each from Islamabad and Gujranwala district, Punjab province.
WHO provided support to the governments in both countries to boost efforts for eradication of the disease through regular surveillance for identification of hotspots through testing of the sewage water/environmental samples for WPV subtypes. In addition to EPI polio doses, a number of supplementary immunization campaigns were conducted in high-risk areas to vaccinate missed children. Internal displacement and the prevailing security situation in both countries, has resulted in the number of reported cases being higher compared to the last few years and efforts are being made to reduce and eradicate the disease from both countries with commitment from the highest levels and partnering agencies.
13. Rift Valley fever
Sudan
The Federal Ministry of Health of Sudan declared a Rift Valley fever outbreak in Week 37 (8‒17 September) and the first case was reported from the Red Sea State (Tohashban Village) and later it spread to five other states. From January to December 2019, a total of 548 cases were reported, including 11 deaths with a case-fatality rate of 2%. The Red Sea State (58% cases) and River Nile State (41% cases) were the most affected states. These two states accounted for 99% of the total cases. Out of the total samples collected, 44% were tested positive (Fig. 33).
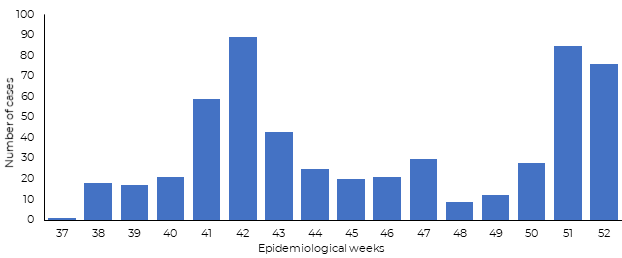
Fig. 33 Rift Valley fever cases reported from Sudan in 2019
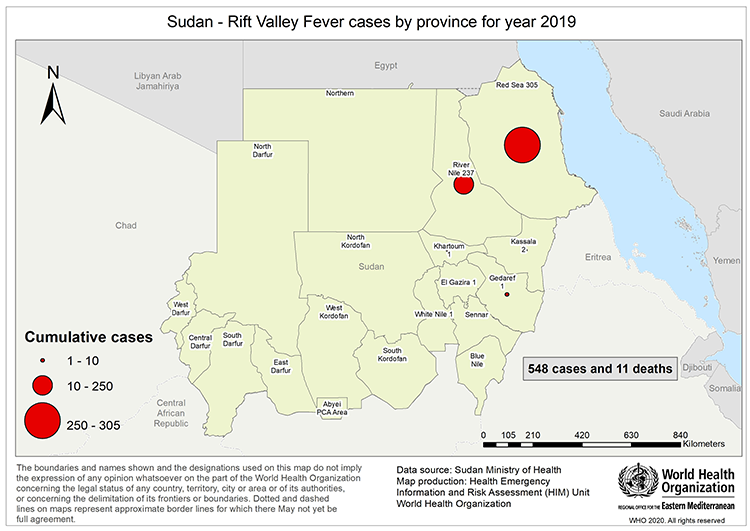
Fig. 34 Geographical distribution of Rift Valley fever cases reported from Sudan in 2019
WHO extended support to Sudan for the prevention and control of this outbreak as it also impacted the economy due to a ban on export of meat/animals, which is a major source of livelihood for most people. The Ministry of Livestock was involved in daily Emergency Operations Centres meetings at the Federal Ministry of Heath for a joint planning and investigation to control the outbreak. Further, training was provided for capacity-building of health staff in case diagnosis, laboratory testing and case management. Health education was conducted through focused group discussions, religious places and distribution of communications materials. Integrated vector control measures (fogging and spray, insect and larvae control, etc.) were taken for prevention and control of all arboviral diseases, including Rift Valley fever. The governments of member countries of the Gulf Cooperation Council, the major destination for livestock and meat export, were involved in developing a mechanism for testing and export of disease-free animals to these countries in order to curtail the economic loss to the country. The Ministry of Livestock and Fisheries declared an end to the animal side of the outbreak on 31 December 2019.
Table 3. Infectious disease outbreaks reported from the countries of the Region in 2019
|
Disease |
Country |
First reported case |
Last reported case |
Total cases* |
Deaths |
CFR (%) |
|
Chickenpox (Varicella) |
Pakistan |
January 2019 |
December 2019 |
1285 |
0 |
- |
|
Chikungunya |
Sudan |
15 September 2019 |
December 2019 |
281 |
5 |
1.78 |
|
Cholera |
Somalia |
January 2019 |
December 2019 |
3100 |
4 |
0.13 |
|
Yemen |
January 2019 |
December 2019 |
861 096 |
1 025 |
0.11 |
|
|
Sudan |
08 September 2019 |
16 December 2019 |
346 |
11 |
3.18 |
|
|
Crimean-Congo haemorrhagic fever |
Afghanistan |
January 2019 |
December 2019 |
583 |
63 |
10.81 |
|
Pakistan |
January 2019 |
December 2019 |
75 |
9 |
12 |
|
|
Dengue |
Yemen |
January 2019 |
December 2019 |
71 688 |
258 |
0.35 |
|
Pakistan |
August 2019 |
December 2019 |
54 079 |
95 |
0.18 |
|
|
Sudan |
28 July 2019 |
December 2019 |
4 205 |
13 |
0.31 |
|
|
Diphtheria |
Yemen |
January 2019 |
December 2019 |
2 020 |
129 |
6.39 |
|
Sudan |
05 February 2019 |
December 2019 |
100 |
13 |
13 |
|
|
Extensively drug-resistant typhoid fever |
Pakistan |
January 2019 |
December 2019 |
9 731 |
0 |
- |
|
Hepatitis A |
Lebanon |
25 August 2019 |
December 2019 |
426 |
- |
- |
|
HIV/AIDS |
Pakistan |
25 April 2019 |
December 2019 |
1 228 |
- |
- |
|
Measles |
Lebanon |
January 2019 |
December 2019 |
1067 |
- |
- |
|
Middle East respiratory syndrome |
Oman |
27 January 2019 |
18-February-2019 |
13 |
4 |
30.78 |
|
Saudi Arabia |
January 2019 |
December 2019 |
205 |
52 |
25.4 |
|
|
United Arab Emirates |
07 October 2019 |
29 December 2019 |
02 |
0 |
- |
|
|
Qatar |
05 December 2019 |
05 December 2019 |
03 |
- |
- |
|
|
Poliomyelitis (WPV1) |
Afghanistan |
January 2019 |
December 2019 |
29 |
- |
- |
|
Pakistan |
January 2019 |
December 2019 |
147 |
- |
- |
|
|
Poliomyelitis (cVDPV2) |
Pakistan |
January 2019 |
December 2019 |
22 |
- |
- |
|
Rift Valley fever |
Sudan |
January 2019 |
December 2019 |
548 |
11 |
2 |


