About UHC
Universal health coverage (UHC) means that all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship. For countries to achieve UHC they require a strong, efficient, well-run health system that meets priority health needs through people-centred integrated care and a system for financing health services so people do not suffer financial hardship when using them.
Universal health coverage has a direct impact on a population’s health. Access to health services enables people to be more productive and active contributors to their families and communities. It also ensures that children can go to school and learn. At the same time, financial risk protection prevents people from being pushed into poverty when they have to pay for health services out of their own pockets. Universal health coverage is thus a critical component of sustainable development and poverty reduction, and a key element of any effort to reduce social inequities. Universal coverage is the hallmark of a government’s commitment to improve the well-being of all its citizens.
UHC is firmly based on the WHO Constitution of 1948 declaring health a fundamental human right and on the Health for All agenda set by the Alma-Ata declaration in 1978.
WHO identifies UHC as a strategic priority, with the goal of 1 billion more people benefiting from universal health coverage by 2023.
UHC does not mean free access to every possible health service for every person. Every country has a different path to achieving UHC and deciding what to cover based on the needs of their people and the resources at hand. It does, however, emphasize the importance of access to health services and information as a basic human right.
Related link
UHC service coverage index
UHC is the overarching platform for achieving the health-related SDGs and one of the key objectives of WHO’s 13th General Programme of Work (2019–2023). The ministers of health of the Region signed the UHC2030 Global Compact collectively at the Ministerial Meeting on the Road to Universal Health Coverage in Salalah, Oman, in September 2018. The ministers confirmed their commitment to achieving UHC through a whole-of-government and whole-of-society approach, and endorsed the Salalah Declaration to “Recognise the key role of Universal Health Coverage in realizing the right to health care and the right to health of all people in the Eastern Mediterranean Region”.
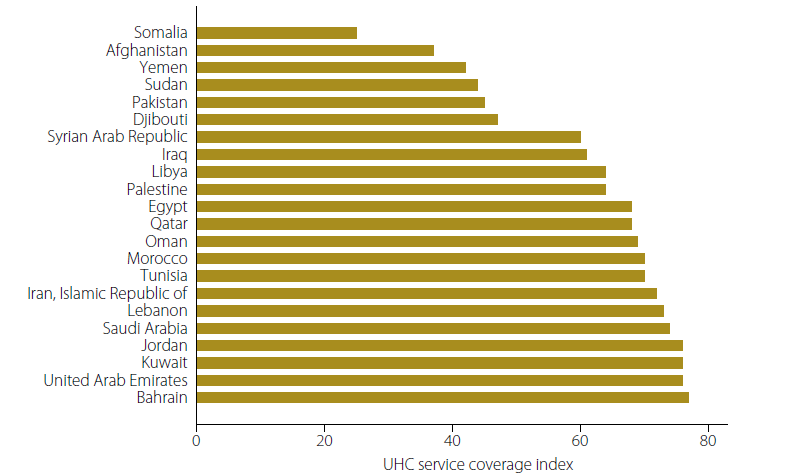
Sixteen tracer indicators that include reproductive, maternal, newborn and child health, infectious diseases, noncommunicable diseases, and service capacity and access, have been selected to measure the breadth of essential health services for UHC (SDG target 3.8). The UHC service coverage index combines the 16 tracer indicators of service coverage into a single summary measure. According to the UHC index, essential health services are less widely available in the Eastern Mediterranean Region than in most regions of the world. In 2015, the UHC service coverage index had a global value of 64 (out of 100), based on data from the WHO/World Bank 2017 global monitoring report.
Ten countries in the Region stand at 64 or less on the UHC service coverage index. This translates to about 347 million people, or a weighted average of 53% of the Region’s population, having access to basic UHC services. Therefore, almost half of the Region’s population do not have access to 16 essential health services.
The 2019 global monitoring report shows that between 2000 and 2017, the UHC global index value increased from 45 to 66 (out of 100); however, the value remained at less than 60 for the Eastern Mediterranean Region.