 Environmental surveillance officers collect wastewater samples during the environmental surveillance activity in Mogadishu, Somalia.
Environmental surveillance officers collect wastewater samples during the environmental surveillance activity in Mogadishu, Somalia.
Quality surveillance is foundational to the polio eradication initiative. Surveillance both detects the presence of poliovirus and informs the programme’s actions — typically, whether to launch a vaccination campaign in response to disease detection, and if so, what sort of campaign. As the world moves closer to polio eradication, surveillance becomes ever more important: the final determination to certify the Eastern Mediterranean Region free of wild poliovirus will rest on the basis of surveillance data. Accordingly, in the Region, the world’s last with transmission of wild poliovirus, the programme directs a significant amount of funding and expertise into the establishment, maintenance and improvement of polio surveillance networks.
How polio surveillance works
Polio surveillance is the practice of exhaustively searching for poliovirus in its only known reservoir — humans. This happens two ways: through surveillance for acute flaccid paralysis (AFP), the primary symptom of poliomyelitis infection, and through surveillance of sewage outflow, to search for virus that has been shed in the stool of infected people. AFP surveillance is known as the gold standard of polio surveillance, but environmental surveillance has an increasingly important role in the Region. For both practices, there are a set of clear surveillance indicators that must be met.
Acute flaccid paralysis (AFP) surveillance
The polio programme relies on a vast network of health care workers, traditional healers, pharmacists and community leaders around the Region to look for, and report, any case of AFP in their community. The main sign or symptom of poliomyelitis, the disease caused by poliovirus, is acute flaccid paralysis (AFP). This is mainly seen in children below 15 years of age. Accordingly, the goal of AFP surveillance is to detect, report and investigate all AFP cases so that poliomyelitis can be ruled out as the cause of the paralysis.
When a person with AFP is reported, a polio surveillance officer travels to their home or the nearest health clinic to collect stool samples. These samples are transported to a WHO-accredited polio laboratory for testing and analysis, to see if poliovirus is present. The journey to the lab can be long, and a key challenge for polio surveillance officers is to maintain the samples at a steady low temperature as they travel in cars, by foot, on donkey, motorbike, boat or airplane. This is called the reverse cold chain, and maintaining it so that the sample arrives at the lab in a testable condition is a critical performance indicator of AFP surveillance.
These are the four steps of AFP surveillance
- Find and report children with AFP
- Transport stool samples for analysis
- Isolate poliovirus
- Map the virus
Environmental surveillance
Environmental surveillance involves testing sewage runoff for the presence of poliovirus. Because the majority of cases of poliomyelitis are asymptomatic, but all infected people shed virus in their stool, environmental surveillance has the benefit of allowing us to detect the presence of polio in an area before any case of paralysis appears.
In places that are polio-free, regular environmental surveillance allows us to detect any new emergence or international spread of polioviruses — a significant threat until polio is eradicated. Environmental surveillance also allows the programme to assess the quality of outbreak response, as it can detect the vaccine-virus used in immunization activities. Genetic data analysis of polioviruses detected from sewage runoff can also show how viruses are related to each other, helping eradicators map their paths of transmission and determine the scope of the vaccination response, if appropriate.
Between 2020 and 2021, the polio programme expanded its environmental surveillance network in the Region, particularly in Afghanistan, Egypt, Somalia and Sudan. Work also began in Djibouti, Iraq, Saudi Arabia and Yemen towards the establishment of laboratory capacity for environmental surveillance.
The Eastern Mediterranean Region Polio Laboratory Network (EPLN)
The Eastern Mediterranean Region Polio Laboratory Network was established in 1991 by WHO and national governments. Its key role is to provide virological information that can be used to target resources on eradicating and, in the case of importations, containing the spread of wild polioviruses.
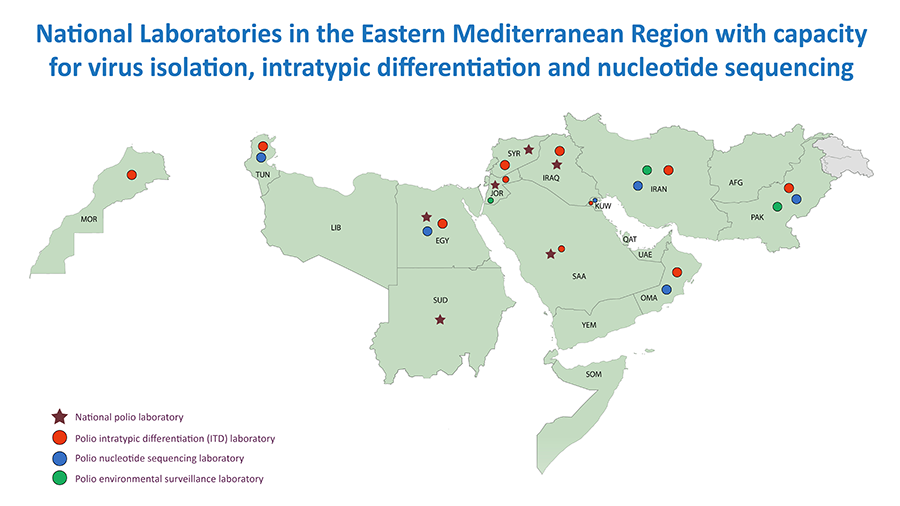
The Network consists of 12 laboratories in a 3-tiered structure: national laboratories, environmental surveillance laboratories, and intratypic differentiation laboratories.
At 12 national laboratories in Egypt, the Islamic Republic of Iran, Iraq, Jordan, Kuwait, Morocco, Oman, Pakistan, Saudi Arabia, Sudan, Syria and Tunisia, polioviruses isolated from fecal samples collected from AFP cases are tested using standardized procedures and reagents. Countries without national laboratories are served by others in the network: Afghanistan is served by Pakistan; Bahrain, Qatar, United Arab Emirates and Yemen are served by Oman; Lebanon is served by Syria; Libya is served by Tunisia. Djibouti, Somalia and Yemen are served by the Kenya Medical Research Institute (KEMRI) laboratory which is not part of the Eastern Mediterranean Region network.
There are seven environment surveillance laboratories across the Region, in Egypt, Jordan, the Islamic Republic of Iran, Kuwait, Pakistan, Sudan and Syria. These laboratories support the environment surveillance activities for their own countries, although the Syria laboratory also tests samples from Lebanon. Djibouti, Somalia and Yemen are served by KEMRI.
The EMR also has 10 intratypic differentiation laboratories, in Egypt, the Islamic Republic of Iran, Jordan, Kuwait, Morocco, Oman, Pakistan, Saudi Arabia, Syria and Tunisia, which perform intratypic differentiation of isolates to confirm whether they are wild poliovirus, vaccine-derived polioviruses, or vaccine-virus.
All networks carry out real-time reverse transcription-polymerase chain reactions (rRT-PCR) for intratypic differentiation laboratories and screening of vaccine-derived polioviruses. There are 5 in the Region (Pakistan, Tunisia, Egypt, Oman and the Islamic Republic of Iran). All wild viruses are subjected to nucleotide sequencing to monitor the virus transmission pattern and relationships.
The Eastern Mediterranean Region Polio Laboratory Network is subject regularly to accreditation visits; separately, the network’s senior supervisors meet annually to develop recommendations to improve performance and adopt new technologies and methods.
Related links
Reports of intercountry meetings for directors of polio laboratories in the Region
Surveillance indicators in the Region
The impact of the COVID-19 pandemic on poliovirus surveillance
Although surveillance systems across the Region were impacted by the COVID-19 pandemic, regional surveillance have continued to function through the pandemic and have done so in line with special guidelines set by the GPEI to ensure the safety of workers. What’s more, the polio surveillance network, in both the field and the laboratory, has supported the pandemic response in setting up surveillance for reporting and detection of COVID-19 cases, contact tracing, laboratory testing and data management.
Even alongside this increase in workload and the complexities wrought by the COVID-19 pandemic, most countries in the Region have met and continue to meet global standards for surveillance indicators.




