Egypt
Building trust, saving lives: Egypt’s journey towards safer hospitals

17 September 2025 – As we mark World Patient Safety Day, we look at how Egypt has placed patient safety at the heart of the transformation of its health care system.
Egypt is currently on a path towards a health care system based on universal health coverage, placing equity, accessibility and quality of care at the centre of its national agenda. From the start, patient safety has been recognized as a key part of this reform, acknowledging that safe services translate into healthier lives and stronger trust between patients and the health system.
In 2025, the Ministry of Health and Population, with support from the WHO Egypt country office, launched the Patient Safety Friendly Hospitals Initiative (PSFHI) to make hospitals safer for everyone.
To implement the PSFHI, the Ministry and WHO Egypt adopted a comprehensive, step-by-step approach based on the following elements:
- Planning with purpose
WHO and the Ministry co-developed a customized assessment tool to evaluate hospitals rigorously and fairly.
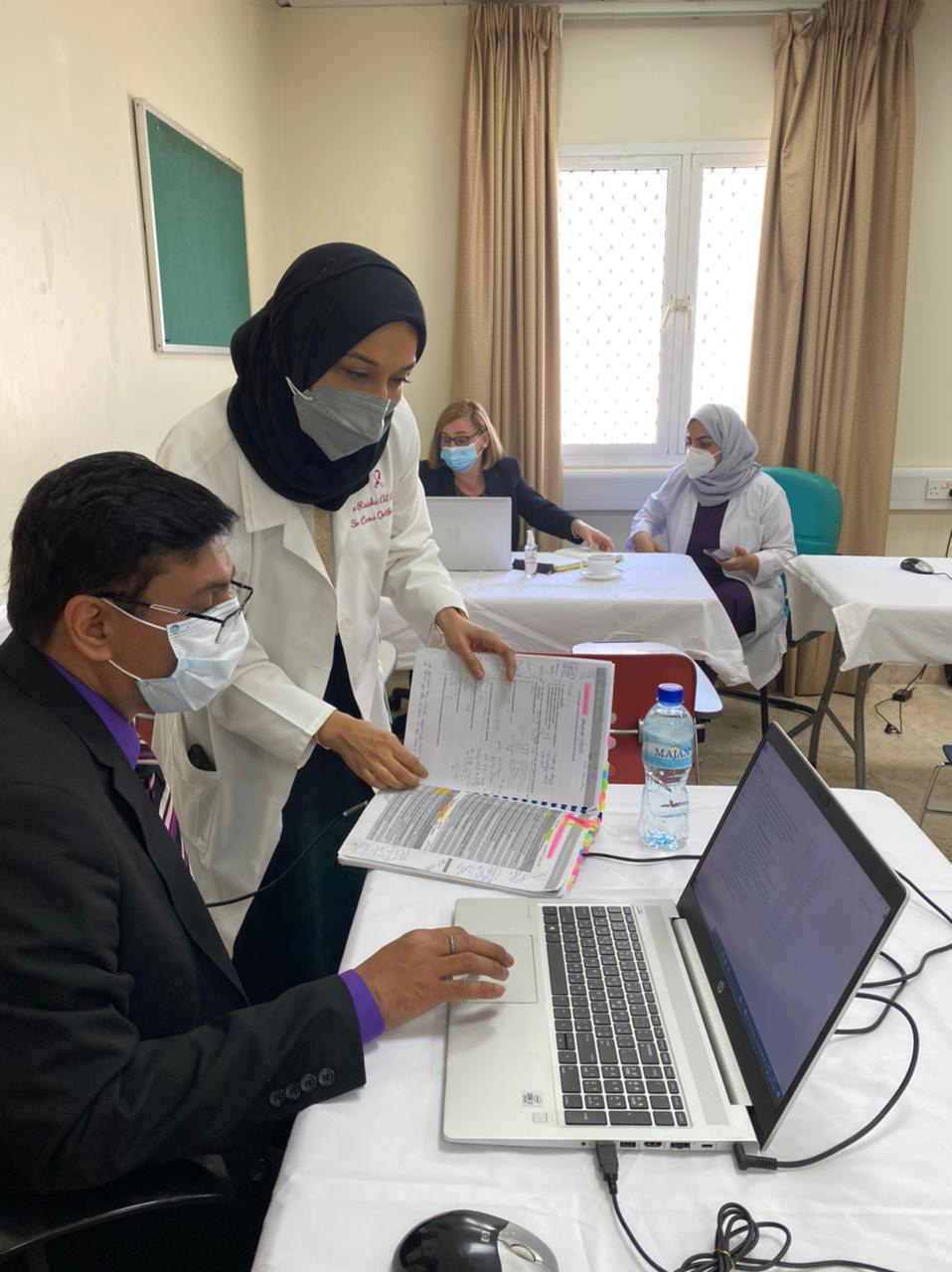
- Empowering teams
Workshops and on-site sessions helped hospital leaders and staff understand the “why” and “how” of patient safety.
- Choosing champions
Three hospitals were selected for their readiness and potential to become regional models. Together with WHO, they identified gaps and built action plans.
- Taking action
From fire safety upgrades to clinical guideline committees, hospitals implemented changes that made a real difference. With WHO’s technical support, hospitals implemented the agreed action plans and:
introduced structured regular patient safety walk-rounds by hospital staff, identifying risks before they become harms;
adopted the WHO Safe Childbirth Checklist;
integrated dedicated safety budgets into hospital planning;
established guideline development committees.
These actions enabled the three hospitals to reach Level 2 recognition, demonstrating measurable progress in embedding patient safety within their institutions.
- Building for the future
A national training programme was undertaken to certify assessors who will lead future evaluations – ensuring the initiative grows and thrives.
In late 2025, Egypt will launch Phase 2, expanding the PSFHI to more hospitals. This time, Egyptian assessors will lead the way, with WHO providing guidance. It’s a model of sustainability, ownership and national pride.
Egypt’s success shows that embedding patient safety into health care reform builds trust and better outcomes. By combining structured assessments, targeted improvements and sustainable national capacity, Egypt is ensuring that universal health coverage is not just about increasing access to health services – it is also about safe, effective and dignified care for all.
Another key focus of the PSFHI has been building resilience. The initiative is not only about improving routine essential services, but also about making sure hospitals can keep delivering them during emergencies, without compromising patient safety standards. This has become especially important as Egypt continues to receive large numbers of displaced people from crisis-affected neighboring countries. By strengthening emergency preparedness and response, hospitals are becoming more resilient and better equipped to protect patients, even in times of crisis.
“When I walk into the hospital now, I feel safer – not just for myself, but for my family and community.” – A patient at one of Egypt’s newly recognized PSFHI hospitals
A key enabler of this progress has been Egypt’s strong commitment to patient safety. In particular, the establishment of the General Administration for Patient Safety at the Ministry of Health and Population provided the leadership and coordination, in collaboration with WHO, that made the project possible.
With every step, Egypt is proving that universal health coverage isn’t just a policy – it’s a promise. And through the PSFHI, that promise is being kept.
Islamic Republic of Iran
Advancing neonatal care in Iran: kangaroo mother care and developmental support transform outcomes for preterm infants

September 2025 – In a significant stride towards safer, more compassionate neonatal care, the Islamic Republic of Iran has successfully scaled up the implementation of kangaroo mother care (KMC) and developmental care packages in neonatal intensive care units (NICUs). These efforts to integrate patient safety and neurodevelopmental support into routine practice are transforming outcomes for preterm and critically ill newborns across the country.
As neonatal survival rates improve, the focus has shifted towards reducing long-term complications, particularly neurodevelopmental disorders. Recognizing the vulnerability of preterm infants to medical errors, infections and stress, the Ministry of Health and Medical Education (MoHME) has prioritized evidence-based interventions that combine safety with developmental care.
KMC – an approach centred on skin-to-skin contact between mother and infant – has been progressively adopted since 2000. In 2013, the Islamic Republic of Iran joined the Newborn Individualized Developmental Care and Assessment Programme Federation International (NFI), further embedding developmental care principles into NICU protocols. Interventions emphasize parental involvement, individualized care and a nurturing environment as key to improving both short- and long-term outcomes.
The MoHME has played a pivotal role in institutionalizing KMC as part of its National Neonatal Health Programme, embedding safety principles such as infection prevention, thermal protection and safe infant positioning into national guidelines. Standardized training for NICU staff, robust monitoring frameworks and infrastructure upgrades have ensured consistent, high-quality implementation, with strategic pilot sites leading the way.
Vali Asr Hospital in Tehran pioneered intermittent KMC and introduced a comprehensive developmental care package, including environmental modifications, sensory stimulation and post-discharge follow-up. The outcomes highlight that integrating developmental care with patient safety principles is essential for high-quality, family-centred neonatal care. The World Health Organization (WHO) recommends further institutional support to sustain and enhance these programmes across all relevant units.
Alzahra Hospital in Tabriz became the first in the Islamic Republic of Iran to implement a continuous KMC model, allowing mothers to remain with their infants 24/7 in a dedicated ward adjacent to the NICU. The KMC model at Alzahra Hospital is a flagship example of how infrastructure, policy and compassionate care can converge to transform neonatal outcomes. It is aligned with WHO's Nurturing Care Framework and has influenced national guideline revisions for sustainable, equitable and family-inclusive neonatal health services.
 The initiative has continued for more than 2 decades. While baseline data on morbidity prior to implementation is limited, internal reports and published studies indicate marked improvements in clinical outcomes, including reduced infections, improved weight gain, enhanced breastfeeding success and better maternal mental health. Post-discharge support, such as developmental assessments and early intervention therapies, further strengthens long-term outcomes.
The initiative has continued for more than 2 decades. While baseline data on morbidity prior to implementation is limited, internal reports and published studies indicate marked improvements in clinical outcomes, including reduced infections, improved weight gain, enhanced breastfeeding success and better maternal mental health. Post-discharge support, such as developmental assessments and early intervention therapies, further strengthens long-term outcomes.
“More than 2 decades of clinical and research experience has shown that engaging parents in the care of newborns, especially in high-risk cases, not only improves infant survival and development but also strengthens family resilience. Family-integrated care enhances communication, reduces medical errors and builds trust between caregivers and families. From a patient safety perspective, it is a transformative approach. Scaling up such evidence-based, inclusive models must be a global priority to ensure safer, more effective neonatal and child health care,” said Dr Mamak Shariat, Full Professor, Maternal, Fetal and Neonatal Research Centre, Tehran University of Medical Sciences
Despite its success, the programme faces challenges related to human resources, father engagement and environmental optimization. Staff turnover rates necessitate ongoing training and orientation. Father engagement remains limited due to lack of awareness, highlighting the need for inclusive education, and environmental optimization is needed to reduce stress and support effective caregiving.
MoHME is addressing these gaps through innovative approaches including continuous capacity-building, infrastructure improvements and family-centred education.
WHO has supported the contextual adaptation of KMC protocols to align with the Iranian health system and safety standards. The United Nations Children’s Fund (UNICEF) Iran has contributed to infrastructure development, parental education and global knowledge exchange through the KMC network.
This robust national and international collaboration has laid the foundation for the sustainable scale up of both intermittent and continuous KMC and catalysed broader reforms in family-integrated neonatal care, with patient safety as a central pillar of service delivery and policy development.
“The adoption of kangaroo mother care across Iran reflects our commitment to delivering high-impact, low-cost innovations that enhance patient safety and strengthen health system resilience,” said the Director General of Hospital Management and Clinical Excellence Centre at MoHME Dr Alireza Askari. “By embedding KMC into national protocols and investing in continuous capacity-building, we are ensuring that even the smallest and most vulnerable newborns receive safe, high-quality and equitable care, regardless of where they are born.”
A model for the Region
Iran’s experience demonstrates that even in resource-constrained settings, safe, family-integrated neonatal care is achievable and scalable. The integration of KMC and developmental care into national policy and practice offers a replicable model for other countries seeking to improve neonatal outcomes while prioritizing patient safety.
Oman
Oman’s safe delivery practices
Safe delivery practices are essential for the health and well-being of mothers and newborns. The Sultanate of Oman, where 98% of deliveries occur in hospitals or certified clinics, has made significant strides in improving maternal and child health by providing accessible care before and during pregnancy and after delivery. Emphasis is placed on regular antenatal check-ups, proper nutrition and early identification of high-risk pregnancies.
The Ministry of Health oversees the availability of equipment, medication and health care provider training focused on addressing common neonatal challenges such as asphyxia, sepsis, prematurity, hypothermia and congenital disorders.
Guidelines for managing newborn problems levels 1 and 2
 In 2007, a neonatal care package was developed. The Ministry of Health revised management guidelines for high-risk newborns and established a training system for health care providers at the primary care level. In 2008, national guidelines on managing newborn problems were rolled out. Adapted to the Omani context from World Health Organization (WHO) guidelines and issued for 2 levels – the first for primary health care facilities equipped for delivery, the second for higher levels of care – the emphasis is on early identification and intervention for problems such as asphyxia, sepsis, prematurity, hypothermia and congenital disorders.
In 2007, a neonatal care package was developed. The Ministry of Health revised management guidelines for high-risk newborns and established a training system for health care providers at the primary care level. In 2008, national guidelines on managing newborn problems were rolled out. Adapted to the Omani context from World Health Organization (WHO) guidelines and issued for 2 levels – the first for primary health care facilities equipped for delivery, the second for higher levels of care – the emphasis is on early identification and intervention for problems such as asphyxia, sepsis, prematurity, hypothermia and congenital disorders.
Infection remains a concern. Sepsis caused by gram-negative bacteria is a major cause of mortality among premature newborns. Rigorous infection control measures, timely diagnosis and appropriate use of antibiotics are essential to combat the problem.
In collaboration with WHO, Oman is taking a lead on the Global Strategy for Infection Prevention and Control. It has implemented a neonatologist-led antimicrobial stewardship programme which has reduced antibiotic use in newborn wards by nearly 65% without negatively impacting mortality rates or the detection of sepsis. To further strengthen health outcomes, Oman supports universal newborn hearing screening protocols and neonatal screening programmes for conditions like congenital hypothyroidism, and protocols are in place for prematurity-related care and safe transport. These initiatives are coordinated by the National Centre for Women and Child Health.
While these practices provide a solid foundation for newborn care, it remains essential to ensure that the mother has a safe delivery, especially in obstetric emergencies. To meet this need, Oman has introduced PROMPT training programmes.
PROMPT in Oman
The PROMPT training programme is an internationally recognized, evidence-based training developed by the PROMPT Foundation in the United Kingdom. Its implementation, based on National Maternal Morbidity and Mortality Committee recommendations, is a central plank of Oman’s strategy to reduce maternal and neonatal complications.
The programme’s objectives are to improve clinical outcomes for mothers and babies by enhancing team responses to obstetric emergencies, strengthening multi-professional teamwork and communication during high-risk obstetric situations, standardizing emergency obstetric care across health care institutions and building institutional capacity by empowering master trainers to cascade the training as part of ongoing staff development.
The training comprises a mix of interactive lectures, skills stations and simulation-based scenarios covering topics such as postpartum haemorrhage management, shoulder dystocia, eclampsia and maternal collapse, cord prolapse, sepsis and early warning signs, team communication and leadership in emergencies, newborn resuscitation and decision-making and risk management in obstetrics.
Incorporated into the national antenatal care policy, the programme will be mandatory in government and private health care institutions providing maternity services.
The first phase of PROMPT training, involving 14 hospitals, was conducted in 2024. The programme has now been adopted as the national standard for obstetric emergency training in Oman. Upon completion of the training, teams are expected to cascade the programme within their respective institutions, contributing to long-term sustainability and quality improvement in maternity care.
The next set of trainings in Oman, hosted by the Ministry of Health, will include Sultan Qaboos University Medical City, the Medical City for Military and Security Services and private hospitals alongside Ministry facilities.
A team has already been identified to oversee PROMPT training in the different hospitals. The team will go on to play a central role as Oman, working in tandem with the PROMPT Foundation in the UK, becomes a regional PROMPT training hub.
Safe transport of ill children
Transferring patients safely between health care facilities is a core function of health care delivery. In 2011, Oman established a safe transport training course, a collaboration between the Ministry of Health’s Department of Woman and Child Health and the Newborn and Paediatric Emergency Transfer Service (NETS-UK) in the United Kingdom.
In 2013, a follow-up training of trainers was conducted to build local capacity and ensure the initiative’s sustainability. National guidelines for the safe transportation of clinically ill children were developed and widely disseminated. First issued in 2013, the guidelines were updated in 2021 to reflect the latest evidence-based practices.
Combined, these efforts illustrate Oman’s unwavering commitment to reduce maternal and infant mortality rates and ensure a safe delivery for every mother and child.
Sudan
Teleconsultations in Sudan bridge gaps in maternal and child health

September 2025, Port Sudan, Sudan – Faced with severe health system disruptions caused by conflict, Sudan has taken a step towards safeguarding maternal and child health through innovative telemedicine solutions. With support from the World Health Organization (WHO), 2 remote consultation platforms – a toll-free call centre and a WhatsApp-based service – are helping vulnerable populations, including those in remote regions and refugee communities, access care.
Sudan’s maternal, newborn and child health indicators are among the worst in the Region. Neonatal mortality stands at 25 per 1000 live births and under-5 mortality at 50 per 1000 live births. Preterm complications, birth asphyxia, neonatal sepsis and respiratory infections are leading causes of death. In conflict-affected areas like Darfur and Kordofan geographic isolation, shortages of skilled personnel and fragmented referral systems result in life-threatening delays in care.
To address these urgent gaps, WHO launched two telemedicine initiatives in late 2024.
The Toll-Free Call Centre (1700) provides 24/7 access to clinical guidance via basic mobile phones, enabling timely intervention for high-risk pregnancies and childhood illnesses.
An encrypted WhatsApp platform allows caregivers to share visual documentation of symptoms, enabling paediatric specialists to remotely assess and guide treatment, reducing diagnostic errors.
By offering zero-cost services, the platforms help advance health equity and allow even the most marginalized populations – including refugees – to access care.
“The ability to visually verify critical symptoms via WhatsApp has the potential to dramatically reduce diagnostic errors, especially in hard-to-reach areas,” says Maternal and Reproductive Health Officer at WHO Sudan Dr Hiba Hussein. “This initiative shows that innovation can thrive even in challenging settings, helping to ensure no mother or child is left behind.”
Since being launched, the platforms have reached 3489 mothers and children, providing urgent guidance and preventing delays in identifying life-threatening emergencies such as severe dehydration and respiratory distress. Initiative outcomes include reduced diagnostic errors through specialist-guided assessments, real-time routing to operational health facilities using dynamic maps and the creation of secure digital records for disease surveillance and outbreak tracking.
The initiative has contributed to broader health system improvements by enhancing service delivery and round the clock clinical support in remote areas and conflict zones, and to workforce capacity-building through training opportunities for frontline providers in emergency care.
In addition, surveillance has been enhanced by securing data that supports outbreak response, and equity advancement – aligned with WHO’s “leave no one behind” mandate – through free access for conflict-affected and displaced populations.
Overcoming challenges, sustainability and expansion
Connectivity and funding issues were among the challenges facing the project. Connectivity issues were mitigated by combining digital platforms with a toll-free service, ensuring access in low-network regions. Health worker capacity gaps were addressed through training on emergency triage and updated maternal and child health protocols.
WHO is advocating for the integration of digital health into Sudan’s national health strategies and for dedicated domestic funding to ensure long-term sustainability. Plans for expansion include virtual mentoring for frontline providers, scaling up the Call Centre to offer specialized care and strengthening referral coordination through digital mapping.
The initiatives are implemented by WHO Sudan, which provides technical guidance and monitoring frameworks, in collaboration with the Sudan Family Planning Association (SFPA), Sudan Medical Specialization Board and Shabaka (Network).
Syria
Empowering communities, saving lives: Syria's caring for newborns and mothers at home programme
 A WHO-supported mobile health team from Al Bir checks the blood pressure of a woman during a home visit in rural Hama. Mobile clinics provide essential health services to families who would otherwise struggle to access care. Photo credit: WHO
A WHO-supported mobile health team from Al Bir checks the blood pressure of a woman during a home visit in rural Hama. Mobile clinics provide essential health services to families who would otherwise struggle to access care. Photo credit: WHO
Born in the sixth month of pregnancy – in a region where access to neonatal care is limited – and weighing just 900 grams, *Lena’s survival was far from certain. But thanks to medical guidance and care protocols provided by the dedicated volunteers of the Syrian Arab Republic’s home-based newborn and maternal care programme, and the tireless commitment of her parents, Lena began to thrive.
That Lena is now a healthy 2-year-old testifies to the strength of family and the lifesaving impact of homebased care. Supported by the team, who provided advice and close follow up, Lena’s parents followed best practices – frequent breastfeeding, skin-to-skin warming, avoidance of supplements and formula. It was a collective effort, rooted in community-based care.
Lena’s family is one of many that have benefitted from the caring for newborns and mothers at home programme. Launched in 2017, the programme reaches around 20 000 families annually in underserved rural areas.
Linked to the healthy village programme, the initiative involves volunteer health workers providing essential care to pregnant women and newborns. Despite funding constraints, it has steadily expanded.
 Children sit beside their mother as she receives care from a WHO-supported Al Bir mobile team in rural Hama. The teams deliver primary health services directly to people’s homes, ensuring no one is left behind. Photo credit: WHO As part of the programme, community health workers conduct home visits during the antenatal period and the first weeks after birth. The programme supports families in adopting best practices for maternal and newborn care at home and promotes care seeking from specialist health professionals when necessary.
Children sit beside their mother as she receives care from a WHO-supported Al Bir mobile team in rural Hama. The teams deliver primary health services directly to people’s homes, ensuring no one is left behind. Photo credit: WHO As part of the programme, community health workers conduct home visits during the antenatal period and the first weeks after birth. The programme supports families in adopting best practices for maternal and newborn care at home and promotes care seeking from specialist health professionals when necessary.
Initiated with support from the World Health Organization (WHO) Regional Office for the Eastern Mediterranean and the WHO Office in Syria, the programme adapted regional modules to local Syrian contexts. It is currently being Implemented in 11 governorates, where a total of 885 volunteers cover 216 healthy villages.
In 2024, 19 180 home visits were made, with 58 newborns and 69 mothers referred to specialized care.
The programme's success is largely due to the dedication of its volunteers who receive 5 days of basic health care training. Capacity-building started in 2018 with a series of training of trainers (TOT) conducted in collaboration with the Regional Office.
Despite the successes, the programme covers just 5% of prenatal, delivery and newborn care needs. Funding remains a significant hurdle to the programme’s sustainability and expansion. Resources are limited, despite occasional contributions from organizations like OCHA, and there are obstacles in reaching areas such as the West North region.
The future
The goal is to build on the programme’s successes and expand its reach. With a renewed focus on quality and training, the programme aims to engage volunteers with higher education – currently volunteers are mostly from preparatory and high school backgrounds – and enhance capacity-building opportunities, including a shift to computerized data collection.
As the programme moves forward, it is poised to make an even greater impact. With a focus on quality, training and capacity-building, the caring for newborns and mothers at home programme will continue to empower communities and save lives.
* Not a real name.








