Page 29 - WHO-HSD Brochure - Flipping Book Version 7
P. 29
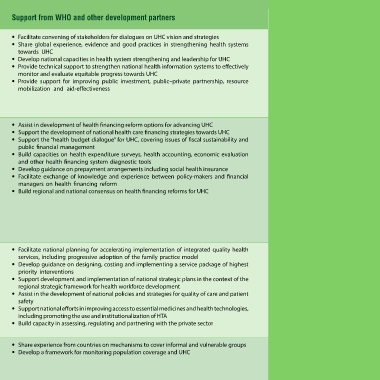
Strategic Actions for countries Support from WHO and other development partners
Framework for action on advancing universal health coverage (UHC)
component
Developing a vision • Formulate a vision to transform the national health system towards UHC • Facilitate convening of stakeholders for dialogues on UHC vision and strategies
and strategy for • Establish a multisectoral mechanism for UHC at the highest level • Share global experience, evidence and good practices in strengthening health systems
universal health • Institutionalize a mechanism for public involvement in the development and promotion of a towards UHC
coverage UHC vision and strategy, e.g. through public representative assemblies and civil society. • Develop national capacities in health system strengthening and leadership for UHC
• Undertake an evidence-informed health system review for UHC to assess the status of and gaps • Provide technical support to strengthen national health information systems to effectively
in financial protection, service and population coverage monitor and evaluate equitable progress towards UHC
• Develop a roadmap for health system strengthening to achieve UHC with short, medium and • Provide support for improving public investment, public–private partnership, resource
long-term goals mobilization and aid-effectiveness
• Strengthen reliable monitoring and evaluation system to track, evaluate and report UHC progress
in the Eastern Mediterranean Region
• Enhance public investment and public–private partnership for UHC
• Promote implementation research for UHC
Improving health • Develop and implement an evidence-informed health financing strategy for UHC • Assist in development of health financing reform options for advancing UHC
financing system • Analyse health expenditure patterns and health financing arrangements using household • Support the development of national health care financing strategies towards UHC
performance and surveys, health accounts and other diagnostic tools to identify gaps and underlying causes • Support the “health budget dialogue” for UHC, covering issues of fiscal sustainability and
enhancing financial • Track the incidence of catastrophic health expenditures and impoverishment, differentiated public financial management
risk protection along socioeconomic and demographic dimensions • Build capacities on health expenditure surveys, health accounting, economic evaluation
• Engage with national finance authorities to promote predictable public financing for health and and other health financing system diagnostic tools
ensure alignment with health sector requirements for UHC • Develop guidance on prepayment arrangements including social health insurance
• Explore creative revenue raising mechanisms for health • Facilitate exchange of knowledge and experience between policy-makers and financial
• Establish/expand prepayment arrangements, e.g. social health insurance and general government managers on health financing reform
revenue arrangements, to limit out-of-pocket payments • Build regional and national consensus on health financing reforms for UHC
• Reduce fragmentation in pooling arrangements across different schemes to avoid negative
consequences for equity and efficiency
• Move from passive to strategic purchasing arrangements (by linking decisions on resource
allocation to information on providers’ performance and health needs)
• Unify national information systems for provider payment
• Identify sources of health sector inefficiencies and ensure value for money
Expanding the • Improve quality, safety and continuity of care by expanding person-centred integrated health • Facilitate national planning for accelerating implementation of integrated quality health
coverage of needed service delivery services, including progressive adoption of the family practice model
health services • Design and implement a service package of highest priority evidence-informed person- and • Develop guidance on designing, costing and implementing a service package of highest
population-based interventions priority interventions
• Improve health workforce availability, accessibility, quality and performance to meet current and • Support development and implementation of national strategic plans in the context of the
future health service requirements regional strategic framework for health workforce development
• Ensure reliable access to, and regulation, quality, safety and affordability of essential medicines • Assist in the development of national policies and strategies for quality of care and patient
and health technologies, as part of the services package, appropriately employing health safety
technology assessment (HTA) • Support national efforts in improving access to essential medicines and health technologies,
• Integrate emergency health care in service delivery to enhance health system resilience including promoting the use and institutionalization of HTA
• Strengthen engagement with and regulation of for-profit and not-for-profit private sector for • Build capacity in assessing, regulating and partnering with the private sector
service provision in support of UHC
Ensuring expansion • Prioritize expansion of service coverage and financial protection for vulnerable and informal • Share experience from countries on mechanisms to cover informal and vulnerable groups
and monitoring of groups as part of the Sustainable Development Goals • Develop a framework for monitoring population coverage and UHC
population coverage • Collect data, disaggregated by socioeconomic and demographic factors, to monitor equity in
progress towards UHC