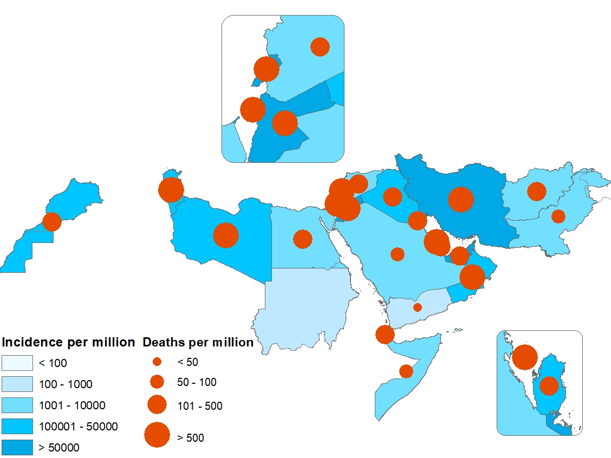
In 2022, 7 countries of the Eastern Mediterranean Region reported cholera outbreaks: Islamic Republic of Iran (confirmed cases: 367; deaths: 7), Iraq (suspected cases: 11 097; deaths: 24), Lebanon (suspected cases: 5422; deaths: 23), Pakistan (confirmed cases: 1002; deaths: 43), Somalia (suspected cases: 15 653; deaths: 88), Syria (suspected cases: 70 220; deaths: 102) and Yemen (suspected cases: 21 178; deaths: 21).
The recent cholera outbreaks in Lebanon and Syria are alarming as these 2 countries are not cholera-endemic and last experienced cholera outbreaks 29 years and 20 years ago respectively.
The cholera outbreaks in the Region in 2022 disproportionately affected children aged under 5 years, who accounted for more than half of suspected cholera cases in Afghanistan (55%) and in Somalia (65%). In addition, about 26% and 24% of suspected cholera cases in Lebanon and Yemen respectively were children aged under 5 years.
Islamic Republic of Iran
A cholera outbreak was reported from the Islamic Republic of Iran in July. By the end of October 2022, the country had reported 367 laboratory-confirmed cholera cases, including 7 cholera-associated deaths (case fatality ratio [CFR]: 1.91%). All these cases have been confirmed by culture as Vibrio cholerae biotype El Tor, serotype Ogawa.
Cases were mostly male (67%), aged 20–60 years (79%) and generally living in urban areas (81%). Most (97.06%) of the confirmed cases were Iranian citizens and only 2.2% were Afghan refugees living in the Islamic Republic of Iran. About 80% of cholera cases were imported (78% from Iraq), and 20% had a history of contact with Iranian passengers to Iraq. About two thirds (69%) of patients were hospitalized, while the rest were treated in an outpatient setting.
WHO supported the scaling up of the cholera response through a multidisciplinary approach that included strengthening surveillance and diagnostics; improving case management; strengthening water, sanitation and hygiene (WASH) systems through multisectoral mechanisms, infection prevention and control (IPC) measures, and guidance on water quality monitoring; and providing support to increase risk perception and knowledge among communities about the disease, its symptoms, associated risks, prevention and health-seeking behaviour.
Iraq
Cholera is endemic in Iraq with frequent upsurges in cases. The last large outbreak occurred in 2015, in which 4965 suspected cholera cases and 2 associated deaths (case fatality ratio [CFR]: 0.04%) were reported. Of the total suspected cases, 2868 were laboratory-confirmed cases, including the 2 cholera-associated deaths, from across 17 of Iraq’s 18 governorates.
Historically, cholera season starts in August or early September; however, in 2022, the cholera outbreak started earlier, and the first cases were reported on 19 June 2022. In 2022, Iraq reported 11 097 suspected cholera cases, including 3705 laboratory-confirmed cases and 24 cholera-associated deaths (CFR: 0.22%). Most of the confirmed cases (91.4%) were reported from 7 directorates of health, with the highest number of cases reported from Baghdad-Resafa (6041 cases), followed by Kirkuk (1676), Babylon (842) and Wassit (705).
 Fig. 4. Epidemiological curve of suspected cholera cases, Iraq, June–December 2022
Fig. 4. Epidemiological curve of suspected cholera cases, Iraq, June–December 2022
 Fig. 5. Geographical distribution of suspected cholera cases and CFR by governorate, Iraq, June–December 2022
Fig. 5. Geographical distribution of suspected cholera cases and CFR by governorate, Iraq, June–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported Iraq’s Ministry of Health in implementing a comprehensive and multisectoral response plan, including surveillance; case management; water, sanitation and hygiene (WASH); logistics; and risk communication and community engagement (RCCE). WHO enhanced coordination among the relevant stakeholders for cholera prevention and response. WHO built the capacity of both the surveillance team and laboratory staff and provided them with updated technical guidelines as well as the required diagnostic kits.
WHO also supported the health authorities to monitor water quality in Iraq. In 2022, WHO trained 40 health workers on water quality monitoring. WHO also dispatched medicines and medical supplies to Sulaymaniyah governorate to support the regional health department in its response to the sudden cholera outbreak in the governorate. The package comprised medicines and medical supplies, including enough infusion sets, antibiotics and Ringer’s lactate solution to cover the needs of about 5000 people.
The WASH Cluster and sector response in Iraq primarily targeted 10 governorates, namely Duhok, Erbil and Sulaymaniyah in the Kurdistan region of Iraq, and Anbar, Baghdad, Basra, Diyala, Kirkuk, Ninewa and Salah al-Din in the federal region of Iraq. The WASH partners worked in these areas to meet the needs of internally displaced people in camps, returnees, and refugees in the affected governates. The response aimed to provide the WASH services needed by the affected populations and prevent and control cholera.
Lebanon
In 2022, Lebanon experienced its first cholera outbreak in almost 3 decades. The fragile health system – already affected by the economic and political crisis – was not ready to cope with such an outbreak. Responding to the cholera outbreak was therefore a more challenging task for the health ministry and its partners than for other cholera-endemic countries.
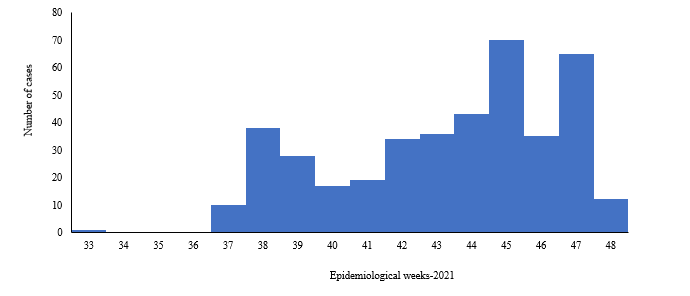
On 6 October 2022, the International Health Regulations national focal point notified WHO of 2 culture-confirmed cholera cases reported from the Akkar and North governorates. The outbreak started in week 42 of 2022 and cases showed an increasing trend until week 45, when the highest number of cases was reported. Cases showed a decreasing trend from week 46 to week 51, but the number of cases rose again in the last week of 2022.
From October to the end of December 2022, a total of 5422 suspected cholera cases, including 661 laboratory-confirmed cholera cases and 23 cholera-associated deaths (case fatality ratio [CFR]: 0.42%), were reported. Of the total cases, 29% were aged under 5 years, almost 53% were female, 29% were Syrian and only 19% of cases were admitted to hospital. At the national level, 20 of the 26 districts in Lebanon registered laboratory-confirmed cholera cases. Although the cumulative attack rate continued to be highest in the Akkar and North governorates, sporadic surges were reported in both the Baalbek-Hermel and Beqaa governorates.
 Fig. 6. Epidemiological curve of suspected cholera cases in Lebanon, October–December 2022
Fig. 6. Epidemiological curve of suspected cholera cases in Lebanon, October–December 2022
 Fig. 7. Geographical distribution of suspected cholera cases by governorate, Lebanon, October–December 2022
Fig. 7. Geographical distribution of suspected cholera cases by governorate, Lebanon, October–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
Joint efforts and coordinated responses by WHO, Lebanon’s Ministry of Public Health, and partners to this outbreak proved effective, with the number of cholera cases significantly reduced through joint interventions and on-time response. WHO worked closely with the Joint National Health Sector Working Group to improve coordination and enhance response.
WHO supported surveillance and laboratories in terms of capacity-building, updating and provision of surveillance and case management guidelines, and provision of sample transport media and rapid diagnostic tests (RDTs). Laboratory directors and technicians were trained in bacteriological analysis.
Cholera treatment centres (CTCs), cholera treatment units (CTUs) and oral rehydration points (ORPs) were also set up, with the support of WHO, in cholera-affected areas.
To raise public awareness of the prevention, control and treatment of cholera, WHO worked closely with communities and partners by producing and distribution of information, education and communication materials such as child-friendly videos, brochures and leaflets.
WHO also supported an oral cholera vaccine (OCV) campaign. The first phase of the door-to-door OCV campaign, which was completed on 4 December 2022, saw 525 630 people receive a single dose. The target was to reach 600 000 people, giving an 87% coverage rate. The second phase of the OCV campaign, targeting high-risk areas, started on 17 December and over 80 000 people received a single dose of OCV. The Ministry of Public Health and partners intensified efforts to increase coverage and vaccine uptake, despite increased vaccine hesitancy and refusals. WHO continued to engage partners and advocate for joint efforts to sustain the cholera preparedness and response activities in Lebanon.
 Fig. 8. Number of OCV doses administered, Lebanon, November–December 2022
Fig. 8. Number of OCV doses administered, Lebanon, November–December 2022
Pakistan
Although cholera is endemic in Pakistan, the last officially declared outbreak occurred following floods in 2010, with 168 confirmed cases reported. Since then, cholera cases have been reported in 5 of the last 11 years.
The 2022 cholera outbreak was first reported in Sindh province following laboratory confirmation of the first case on 15 January 2022. On 29 April 2022, Sindh’s Director-General for Health declared the cholera outbreak in Karachi. Cholera then started to spread, affecting more provinces. On 14 June 2022, Pakistan was hit by a devastating flood that affected more than 33 million people and displaced 500 000 people.
From January to December 2022, a total of 27 766 samples were tested, with 1002 laboratory-confirmed cholera cases. Pakistan also reported 43 cholera-associated deaths in 2022: 40 deaths in Balochistan and 3 in Khyber Pakhtunkhwa.
 Fig. 9. Number of cholera samples tested and laboratory-confirmed cases by week, Pakistan, January–December 2022
Fig. 9. Number of cholera samples tested and laboratory-confirmed cases by week, Pakistan, January–December 2022
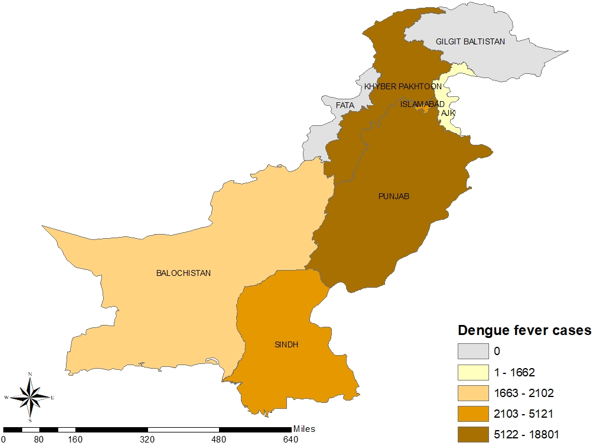
 Fig. 10. Geographical distribution of suspected cholera cases by province, Pakistan, January–December 2022
Fig. 10. Geographical distribution of suspected cholera cases by province, Pakistan, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO supported the federal and provincial ministries of health in all response pillars: leadership and coordination, surveillance system, laboratory confirmation, case management, risk communication and community engagement (RCCE), water, sanitation and hygiene (WASH) and oral cholera vaccine (OCV). Examples of the support provided by WHO in Pakistan include the establishment of 813 surveillance sentinel sites for early detection of acute diarrhoeal cases; expansion of the number of technical laboratories for diagnosis of cholera from 6 to 38 laboratories; provision of Cary-Blair and sample transport media to outbreak-affected districts; development of a laboratory strategy; recruitment of human resources; and capacity-building of health workers.
With WHO support, an OCV campaign was also carried out in 4 provinces – Balochistan, Khyber Pakhtunkhwa, Punjab and Sindh –with more than 2.8 million people receiving a single dose of OCV (average coverage of 96%).
Table 1. Number of people who received OCV, Pakistan, 2022
|
Province
|
No. targeted
|
No. vaccinated
|
Coverage (%)
|
|
Balochistan
|
754 784
|
675 916
|
89.6
|
|
Khyber Pakhtunkhwa
|
383 531
|
415 984
|
108.5
|
|
Punjab
|
1 196 939
|
1 144 058
|
95.6
|
|
Sindh
|
590 878
|
571 823
|
96.8
|
|
Total
|
2 926 132
|
2 807 781
|
96.0
|
Somalia
Somalia is considered one of the countries most affected by natural and human-made disasters. These emergencies have significantly undermined the health and well-being of millions of people in the country. According to WHO, more than 7.8 million people in 74 districts were affected by severe drought in 2022, with more than 1 million displaced from their homes. In addition, more than 4.3 million people faced severe food insecurity and over 6.4 million people lacked access to safe drinking water in 2022.
Further, the past 30 years of prolonged conflict, and the COVID-19 emergency, on top of political instability, climate change impacts, mass population displacement, poor water and sanitation infrastructure, and low awareness among the general population of prevention and control of infectious disease outbreaks, have created an environment conducive to the spread of infectious diseases, including cholera.
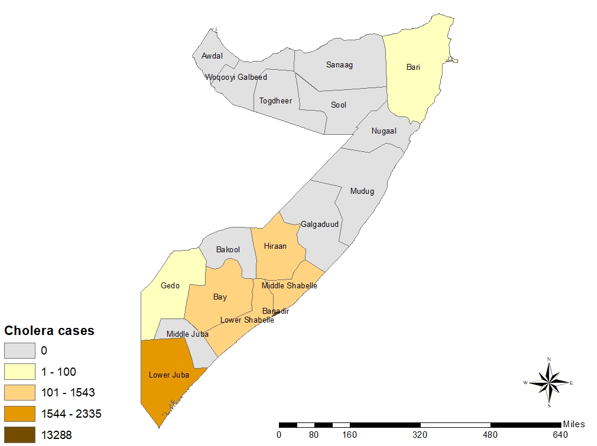
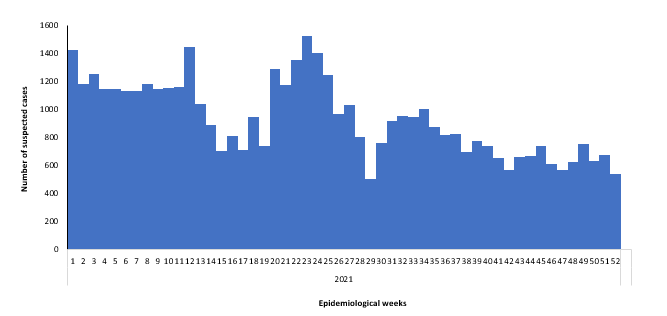
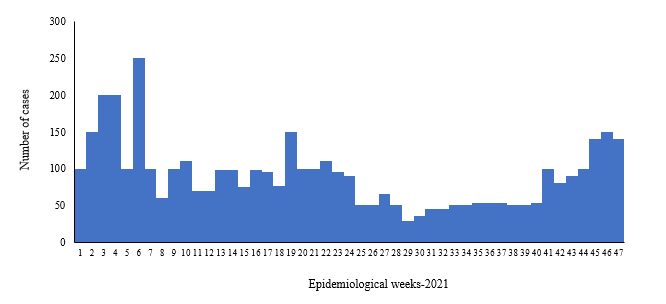
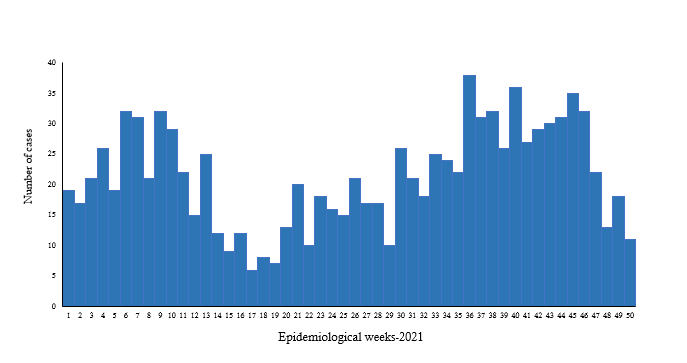
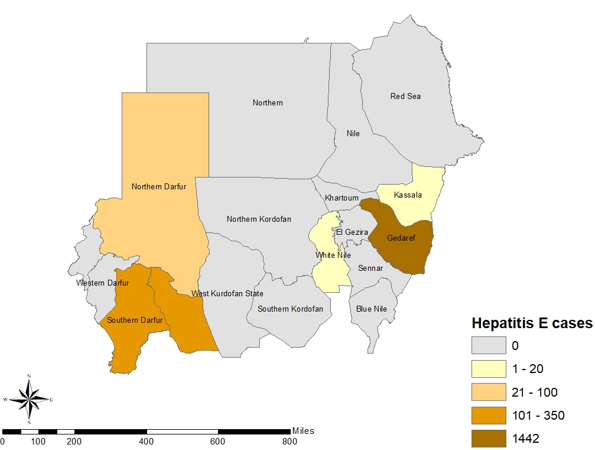
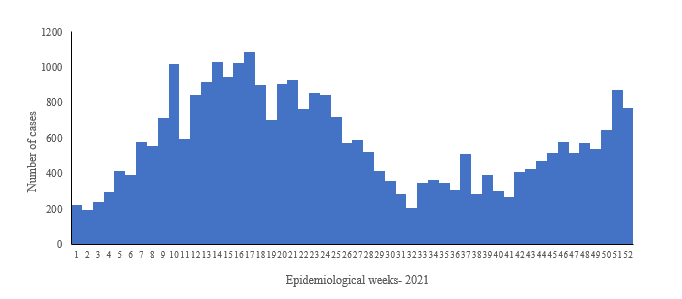
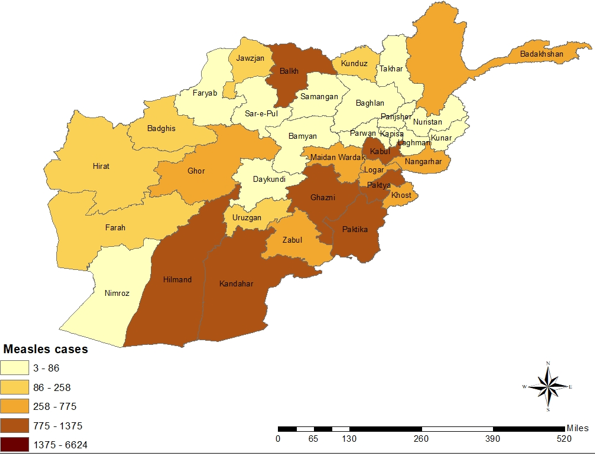
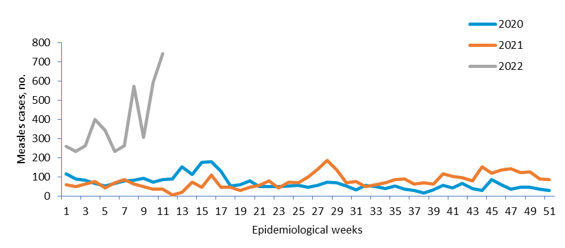
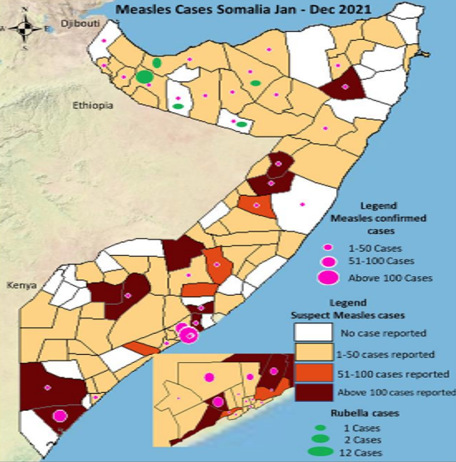
In 2022, a total of 15 653 suspected cholera cases, including 88 cholera-associated deaths (case fatality ratio [CFR]: 0.56%), were reported from 25 drought-affected districts. The number of suspected cases increased significantly from week 13 of 2022, with cases peaking in week 17. The number of suspected cases showed a decreasing trend from week 19 to week 30 of 2022, before switching back to an increasing trend for weeks 36 to 49 of 2022.
In total, 2200 samples were tested in 2022 at the National Public Health Laboratory in Mogadishu, of which 279 were positive for Vibrio cholerae O1 serotype Ogawa . Of the confirmed cases , 64% were children aged under 5 years and 48% were women. The highest incidences of confirmed cholera cases were reported in Daynile, Dharkenley, Kahda and Kismayo districts, while most of the deaths were reported from Daynile, Hawle Wadag, Kahda and Wanlaweyn districts.
 Fig. 11. Epidemiological curve of suspected cholera cases and CFR, Somalia, January–December 2022
Fig. 11. Epidemiological curve of suspected cholera cases and CFR, Somalia, January–December 2022
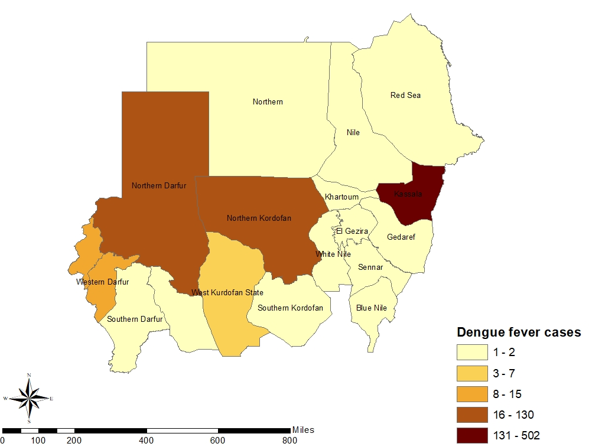
 Fig. 12. Geographical distribution of suspected cholera cases and CFR by district, Somalia, January–December 2022
Fig. 12. Geographical distribution of suspected cholera cases and CFR by district, Somalia, January–December 2022
WHO, in close coordination with partners, supported Somalia’s Ministry of Health (MOH) and health system in all response pillars, including leadership and coordination, surveillance system, laboratory confirmation, case management, risk communication and community engagement (RCCE), water, sanitation and hygiene (WASH), and oral cholera vaccine (OCV) administration.
WHO conducted regular meetings and worked on improving coordination and response within the federal health authorities in Banaadir and the southern states . Following a WHO cholera risk assessment, the country was graded as very high risk. WHO also built the capacity of the surveillance and laboratory teams and provided them with updated guidelines, laboratory kits, sample transportation media and sample culture facilities. Samples were continually collected and sent to the National Public Health Laboratory in Mogadishu for culture and sensitivity studies as per the testing strategy. WHO also trained health workers in Somalia on cholera case management and provided case management, case investigation, and hygiene kits.
WHO worked closely with partners and the MOH to improve the WASH situation both in health facilities and in communities. In close coordination with the United Nations Children’s Fund (UNICEF) and MOH, WHO jointly worked on the provision of safe and clean drinking water to the country’s drought-affected districts. WHO technical experts supported the Health Cluster partners and MOH by providing health sensitization sessions targeting internally displaced people.
WHO also supported implementation of an oral cholera vaccine (OCV) campaign, during which 888 092 people aged 1 year and over received 2 doses of OCV, with 95% coverage in 9 districts (Table 2).
Table 2. Number of OCV doses administered by district, Somalia, 2022
|
District
|
No. targeted
|
No. vaccinated
|
Coverage (%)
|
|
Marka
|
66 988
|
62 622
|
93
|
|
Afgoi
|
97 196
|
93 371
|
96
|
|
Baidoa
|
187 386
|
182 507
|
97
|
|
Dharkenley
|
62 406
|
59 604
|
96
|
|
Daynile
|
79 716
|
73 993
|
93
|
|
Hodan
|
175 031
|
164 262
|
94
|
|
Jowhar
|
57 578
|
56 512
|
98
|
|
Madina
|
144 140
|
135 534
|
94
|
|
Wanlaweyn
|
64 070
|
59 687
|
93
|
|
Total
|
934 511
|
888 092
|
95
|
Syria
Basic infrastructure in Syria has been undermined by prolonged conflict, mass displacement, economic crisis, and political unrest. After almost 2 decades since the last confirmed case of locally transmitted cholera, the country experienced a cholera outbreak in 2022. This was alarming for other typically cholera-free countries in the Eastern Mediterranean Region, especially those countries neighbouring Syria. Previously, the last confirmed cholera case had been an imported case, reported in 2015 in Aleppo governorate, with no further local transmission documented.
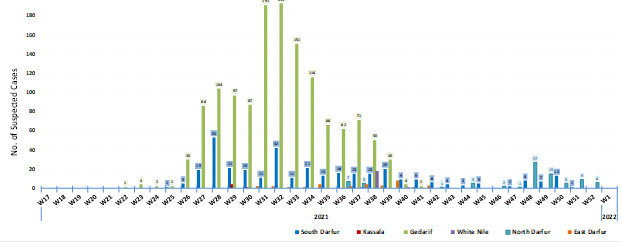
The first case of the 2022 outbreak was detected on 22 August in Aleppo and confirmed on 25 August. On 10 September 2022, the Syrian Ministry of Health declared a cholera outbreak when 15 laboratory-confirmed cholera cases were reported from Aleppo governorate, including a single cholera-associated death. After that, cholera spread to all 14 governorates of Syria. From 25 August to 31 December 2022, a total of 70 220 suspected cholera cases were reported, with 102 associated deaths (case fatality ratio [CFR]: 0.15%), from the 14 governorates.
In 2022, a total of 4352 samples were tested using rapid diagnostic tests (RDTs), of which 1886 samples were positive for Vibrio cholerae. A total of 3336 stool samples were tested by culture and polymerase chain reaction (PCR) methods, of which 868 tested positive for V. cholerae, with a positivity rate of 26%. WHO supported antibiotics susceptibility in the country, where tests showed resistance for ampicillin, furazolidone, and nalidixic acid, and sensitivity for ciprofloxacin, azithromycin and trimethoprim/sulfamethoxazole.
The governorates most affected by the outbreak were Deir Al Zour (20 560 cases; 29.28% of the total cases), Edleb (17 784 cases; 25.33%), Raqua (14 372 cases; 20.47%) and Aleppo (14 064 cases; 20.03%). Additionally, 5037 suspected cases and 7 associated deaths were reported from camps for internally displaced people in northern Syria. Regarding age distribution, 44.58% of the suspected cases were aged under 5 years. Males accounted for 52% of all cases and females for 48%. Laboratory confirmation was carried out in 7 designated laboratories, including the Central Public Health Laboratory.
 Fig. 13. Epidemiological curve of suspected cholera cases, Syria, August–December 2022
Fig. 13. Epidemiological curve of suspected cholera cases, Syria, August–December 2022
 Fig. 14. Geographical distribution of suspected cholera cases and CFR by governorate, Syria, December 2022
Fig. 14. Geographical distribution of suspected cholera cases and CFR by governorate, Syria, December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO provided both technical and financial support to the health system of Syria in all outbreak response pillars: leadership and coordination; surveillance system; laboratory confirmation; case management; risk communication and community engagement (RCCE); water, sanitation and hygiene (WASH); and oral cholera vaccine (OCV). WHO trained health workers in various disciplines, including surveillance, laboratory confirmation, and case management, and provided them with technical guidelines and case management protocols.
To enhance active case finding and diagnose cholera on time, WHO supported Syria to establish a sample management system, including sample transportation, by ensuring the provision of sample transport media (Cary-Blair) and rapid diagnostic tests (RDTs) to health facilities in the country. WHO supported the establishment of cholera treatment centres (CTCs) and cholera treatment units (CTUs) and oral rehydration points (ORPs) across the affected areas, and provided them with the needed cholera kits, intravenous infusions and oral rehydration solution. WHO also worked closely with the WASH Cluster partners to provide safe drinking water and improve sanitation and hygiene for the prevention and control of cholera outbreaks.
Moreover, WHO supported Syria to receive 2 million doses of oral cholera vaccine (OCV) to implement a vaccination campaign (single-dose strategy) targeting 2 million people aged 1 year and over through 63 fixed facilities and 685 mobile teams. The campaign was implemented through fixed points as well as a door-to-door approach. About 1772 health workers were trained and deployed to deliver vaccination for this campaign, in addition to 36 supply officers and 97 supervisors from different levels will participate in the campaign. By end December 2022, more than 1 944 807 people aged 1 year and over (98% of the targeted population) were vaccinated against cholera in Syria.
In addition, on 29 December 2022, the International Coordinating Group (ICG) on Vaccine Provision approved 1 702 383 doses of OCV to conduct a reactive vaccination campaign (single-dose strategy) in northwest Syria targeting 3 subdistricts (A’zaz, Dana and Maaret Tamsrin).
Table 3. Number of people who received OCV, Syria, 2022
|
Governorate
|
No. targeted
|
No. vaccinated
|
Coverage (%)
|
|
Hasakeh
|
395 423
|
399 948
|
101
|
|
Deir Ezzor
|
750 000
|
763 601
|
102
|
|
Raqqa
|
497 746
|
431 258
|
87
|
|
Aleppo
|
350 000
|
350 000
|
100
|
|
Total
|
1 993 169
|
1 944 807
|
98
|
Yemen
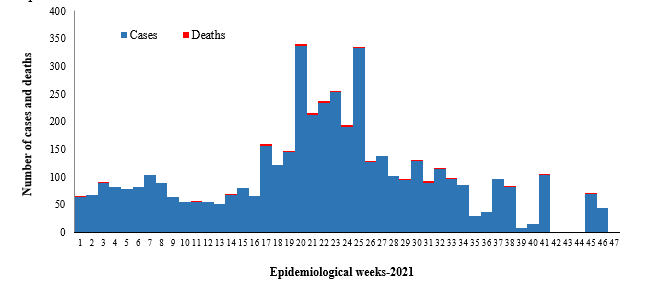
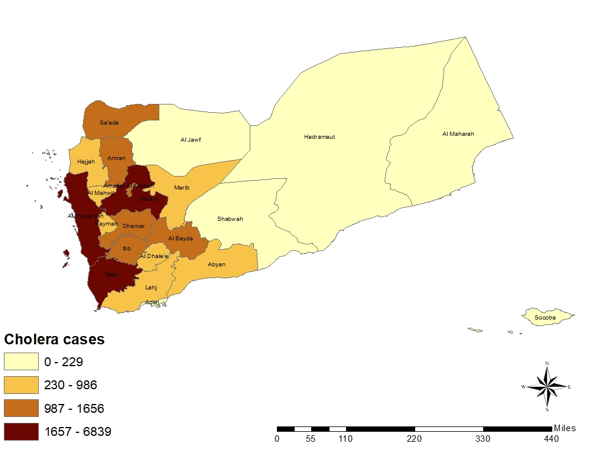
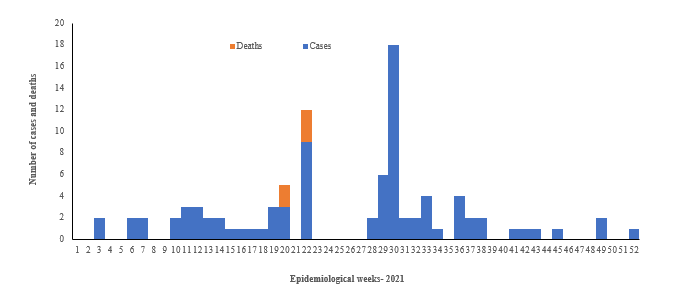
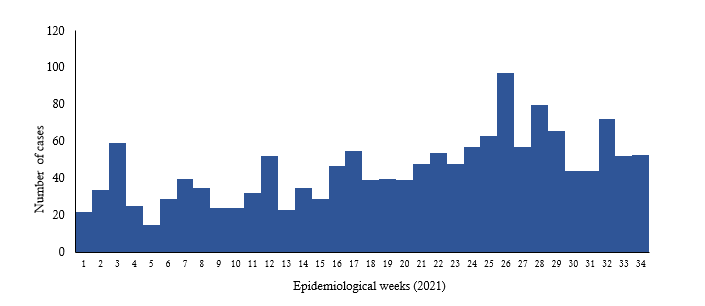
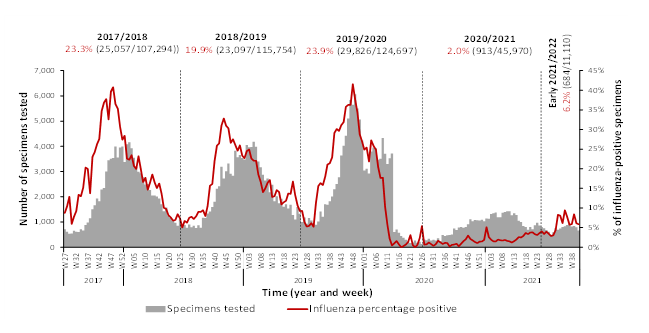
The cholera outbreak first reported in Yemen in October 2016 continued to affect the entire country in 2021 and 2022. A total of 21 178 suspected cholera cases, including 21 associated deaths (case fatality ratio [CFR]: 0.10%), were reported from Yemen in 2022. A total of 2282 rapid diagnostic tests (RDTs) were conducted, of which 657 were positive. The highest numbers of cases were reported in weeks 1 and 2 of 2022. After this period, the outbreak showed a decreasing trend overall, with few fluctuations in weeks 8, 20, 34 and 42 of 2022. The lowest number of cases was reported in week 51 of 2022.
WHO has supported health authorities in Yemen to prevent, control and manage the outbreak since cholera erupted in the country in 2016. WHO set up 28 public health emergency operations centres as part of the long-lasting response to the cholera outbreak in Yemen. WHO also provides cholera management kits to the existing cholera treatment centres (CTCs) or cholera treatment units (CTUs) in health facilities in Yemen.
 Fig. 15. Epidemiological curve of suspected cholera cases, Yemen, January–December 2022
Fig. 15. Epidemiological curve of suspected cholera cases, Yemen, January–December 2022
 Geographical distribution of suspected cholera cases and CFR by governorate, Yemen, January–December 2022
Geographical distribution of suspected cholera cases and CFR by governorate, Yemen, January–December 2022
The boundaries and names shown, and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
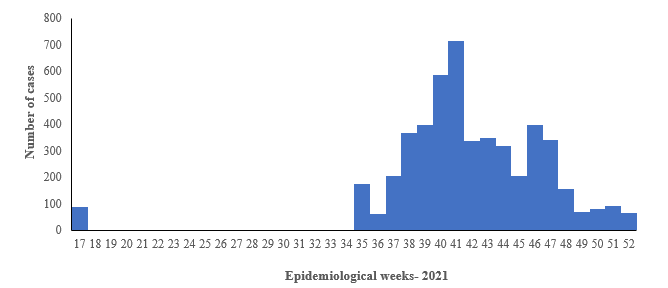
 Fig. 2. Epidemiological curve of AWD cases, Afghanistan, May–December 2022
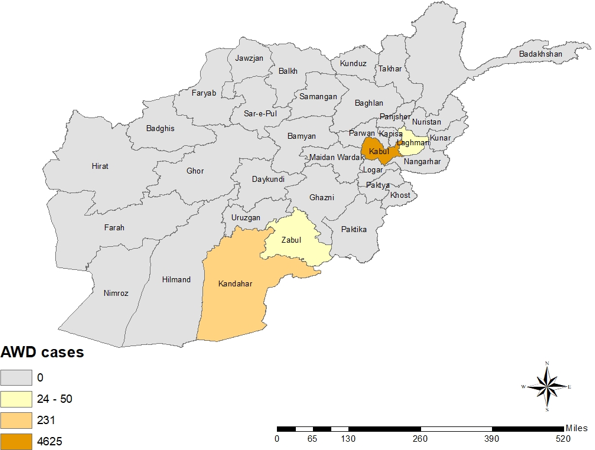
Fig. 2. Epidemiological curve of AWD cases, Afghanistan, May–December 2022 Fig. 3. Geographical distribution of AWD cases and deaths by province, Afghanistan, May–December 2022.
Fig. 3. Geographical distribution of AWD cases and deaths by province, Afghanistan, May–December 2022.