WHO doctor awarded for helping the mothers and babies of Gaza
 WHO obstetrician and gynaecologist Dr Nashwa Skaik, who leads the pioneering Early Essential Newborn Care project which assists with 75 per cent of all births in Gaza, has been awarded WHO Director-General’s Award of Excellence for her work. Credit: WHO22 December 2019, Gaza – “Families and in particular, mothers and infants, are the essence of any society and they should never be neglected. I am immensely honoured and grateful for this recognition, which is a true reflection of the global and regional efforts to improve mother and newborn health in all settings. This reward is a huge boost to myself and the team in our office,” Dr Nashwa Skaik, WHO’s obstetrician and gynaecologist in Gaza, reflects after receiving the WHO Director-General’s Award of Excellence for her work managing a pioneering maternal and newborn health care project in the Gaza Strip to prevent and treat the key causes of newborn mortality and diseases.
WHO obstetrician and gynaecologist Dr Nashwa Skaik, who leads the pioneering Early Essential Newborn Care project which assists with 75 per cent of all births in Gaza, has been awarded WHO Director-General’s Award of Excellence for her work. Credit: WHO22 December 2019, Gaza – “Families and in particular, mothers and infants, are the essence of any society and they should never be neglected. I am immensely honoured and grateful for this recognition, which is a true reflection of the global and regional efforts to improve mother and newborn health in all settings. This reward is a huge boost to myself and the team in our office,” Dr Nashwa Skaik, WHO’s obstetrician and gynaecologist in Gaza, reflects after receiving the WHO Director-General’s Award of Excellence for her work managing a pioneering maternal and newborn health care project in the Gaza Strip to prevent and treat the key causes of newborn mortality and diseases.
In Palestine, babies aged less than one month old account for 50 per cent of deaths in children under five. Half of these deaths in babies occur in the first day of life, mainly from complications related to prematurity, birth asphyxia and infection.
Based on international evidence, Dr Nashwa and colleagues at WHO, rolled out the Early Essential Newborn Care project in 2017 with the Ministry of Health in Gaza to ensure that quality essential care is provided during critical moments around birth, in addition to care for premature, low-birthweight and sick babies.
 The project has strengthened the Ministry of Health’s system from the bottom up, by coaching local clinical staff with a package of simple and cost-effective evidence-based interventions during childbirth and immediately after, and focusing on the elimination of harmful and outdated practices in the first 24 hours of life. This includes reshaping policy and guidelines, managing supplies and staff, and providing health information.
The project has strengthened the Ministry of Health’s system from the bottom up, by coaching local clinical staff with a package of simple and cost-effective evidence-based interventions during childbirth and immediately after, and focusing on the elimination of harmful and outdated practices in the first 24 hours of life. This includes reshaping policy and guidelines, managing supplies and staff, and providing health information.
The project now covers 75 per cent of all births in Gaza in maternity and neonatal units in four targeted hospitals and widespread adoption has resulted in significant improvements since 2017 in key areas including the following.
Early and exclusive breastfeeding: take up improved from 21% to 52.5% from 2017 to 2019. These practices, where infants receive breastmilk within one hour of birth and where they only receive breastmilk without additional food or drink, are known to lower newborn deaths by 22%. Breastfeeding protects the baby from common childhood illnesses such as diarrhoea and pneumonia and may also have longer-term health benefits, such as reducing the risk of overweight and obesity in childhood and adolescence.
Babies receiving sustained skin-to-skin contact: this increased from 0% to 35% from 2017 to 2019. This practice, where a baby is laid directly on their mother’s bare chest shortly after birth, is essential for preventing temperature loss and diseases that lead to infection and death. Among infants who received this care, there is a reduction in newborn admission to intensive care due to respiratory problems by 5% in Gaza. In addition, it helps parents bond with their babies and supports better physical and developmental outcomes for the baby.
Dr Skaik said she treasures the opportunities she gets at WHO:
“They are like no other place. I enjoy my everyday work with the team and the space I am given to be more creative and innovative. We try our best to deliver high quality and unique care to all mothers and babies in Gaza, which ensures that they thrive and survive despite the difficult circumstances.”
The WHO team congratulates Dr Skaik and her colleagues for their dedication and achievements in improving the lives of mothers and babies in Gaza.
Patient and health worker shot with live ammunition during Gaza’s Great March of Return
 Sabreen is a 28-year-old first responder and team leader of the Nabed Al-Hayat team, working east of Rafah in the south of the Gaza Strip. Sabreen established the independent team on 6 April 2018, soon after the beginning of Gaza’s Great March of Return. Her team of 13 at the start of demonstrations included Abdullah al-Qutati, who was shot and killed on 10 August while working to provide help to those injured. Today, the team comprises 12 first responders, though different team members have had to take leaves of absence from volunteering due to injuries sustained while working to deliver healthcare. The team works closely with the Ministry of Health field medical point.
Sabreen is a 28-year-old first responder and team leader of the Nabed Al-Hayat team, working east of Rafah in the south of the Gaza Strip. Sabreen established the independent team on 6 April 2018, soon after the beginning of Gaza’s Great March of Return. Her team of 13 at the start of demonstrations included Abdullah al-Qutati, who was shot and killed on 10 August while working to provide help to those injured. Today, the team comprises 12 first responders, though different team members have had to take leaves of absence from volunteering due to injuries sustained while working to deliver healthcare. The team works closely with the Ministry of Health field medical point.
On 27 September 2019, Sabreen was treating a child who had suffered gas inhalation close to the Gaza fence. While receiving care, the child was shot with live ammunition in his back, which penetrated into his abdomen. Sabreen remembers, “At first, I collapsed with grief and started crying. Then I straight away resumed providing first aid to him [the child] until he was transferred to the medical point. We were about 100 meters from the fence… He was under my care and I couldn›t believe they would shoot a child while a paramedic was treating him. After that, a journalist standing near me had a call from the Israeli side to convey a message to me that I should leave the place and that they would shoot warning bullets to our side. While leaving, they shot about ten bullets around me.” The child, 13 years old, was transferred to the European Gaza Hospital and admitted to the intensive care unit after surgery.
Approximately 20 minutes after the child was shot, at around 6:10pm, Sabreen saw four injured persons close to the fence in need of assistance. She went forward to help and had begun to treat one of the persons when she was shot with live ammunition. The bullet went through her right forearm, severing a nerve in her hand, and into her abdomen. She had heavy bleeding from her liver and was rushed to hospital. At hospital, Sabreen was taken straight to the operating theatre to stop the bleeding. After the surgery, the doctors told her family that the bullet had lodged next to her spine and that intervening to remove it would risk additional health problems. Sabreen stayed at the hospital for four days under observation before she was discharged.
Since her injury, Sabreen has become dependent on her husband and mother to move around. She can only stand with difficulty and needs to walk slowly, requiring help for most of her daily tasks. She suffers numbness in both her legs and has also lost some movements and feeling in her right hand.
Sabreen says, “It’s not my first injury. I was shot in my head with live ammunition a few months ago which affected my sight… I feel I am targeted as a paramedic and in Gaza we have never been truly protected. In spite of all the risks, I choose to be a first responder at the fence. I believe it is our responsibility to treat those who need our help and our skills.”
Sabreen is married with a 7-year-old daughter who is at primary school. “After my injury, I haven’t been able to properly care for my daughter. Now my husband or my mother have to care for her. Sometimes my daughter has had to miss school when her father is at work. Really, it is so hard for me as a mother to be unable to care for my daughter as I want to. I never felt as disabled as when I was unable to help her.”
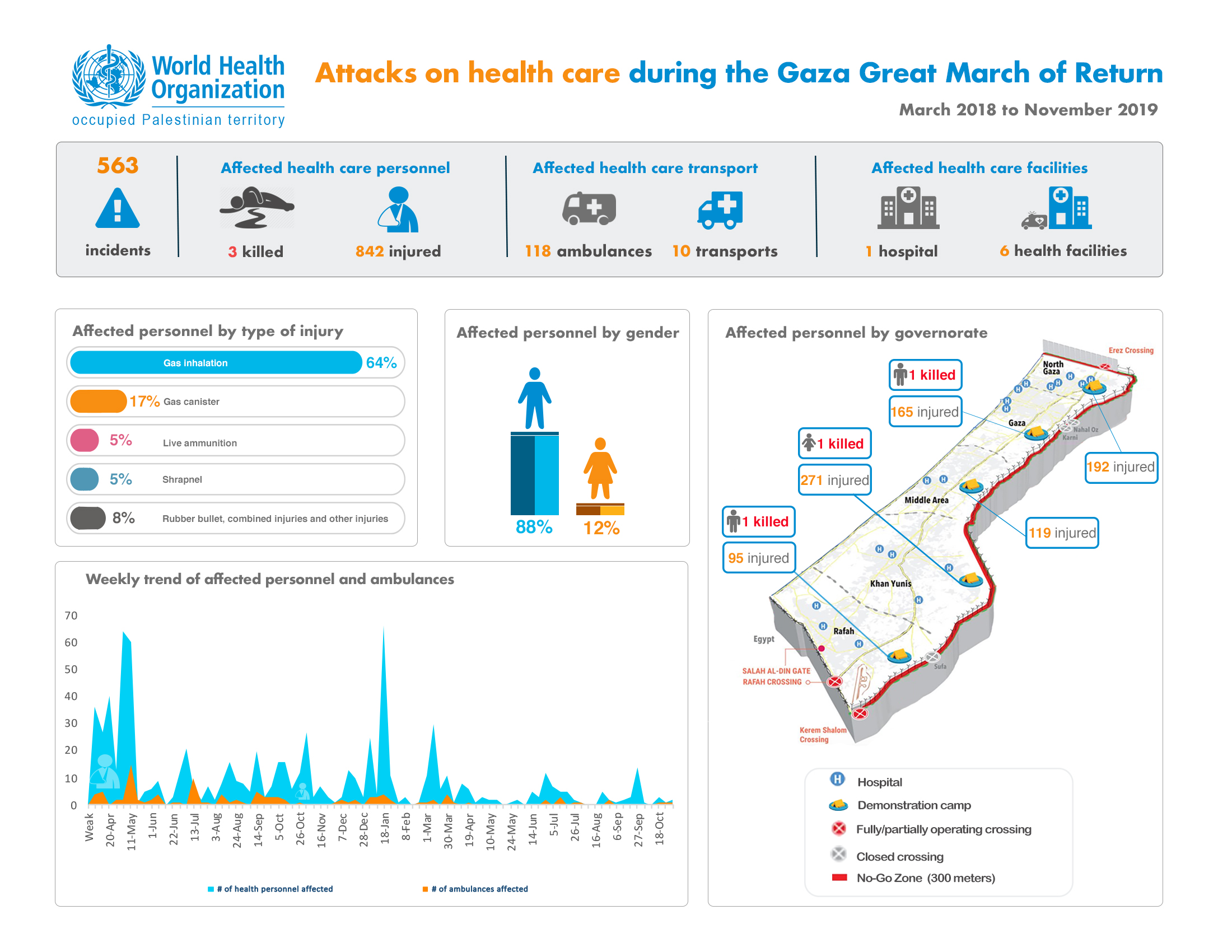
Sabreen sustained the 44th and 45th live ammunition injuries among health workers in the Gaza Strip since the start of the Great March of Return. From 30 March 2018 to 30 September 2019, three health workers have been killed and 832 injured in 550 recorded incidents against health staff and facilities in the Gaza Strip.
WHO launches report on the Right to Health 2018, October 2019
 October 2019, Ramallah – WHO today released its report, “Right to Health in the occupied Palestinian territory: 2018”. The report examines obstacles to achieving the highest attainable standard of health for Palestinians living under occupation, including barriers to adequate health care provision, access to health care, determinants of health beyond health care and health attacks.
October 2019, Ramallah – WHO today released its report, “Right to Health in the occupied Palestinian territory: 2018”. The report examines obstacles to achieving the highest attainable standard of health for Palestinians living under occupation, including barriers to adequate health care provision, access to health care, determinants of health beyond health care and health attacks.
The launch event was held in Ramallah, with opening remarks from Dr Gerald Rockenschaub, Head of WHO office in the occupied Palestinian territory, Mr James Heenan, Head of the Office of the High Commissioner of Human Rights in the occupied Palestinian territory, Mr Jamie McGoldrick, Humanitarian Coordinator for the Occupied Palestinian Territory, and Dr Mai Alkaila, Minister of Health for Palestine.
Dr Rockenschaub commented on the findings of the report: “Palestinians in the West Bank and Gaza Strip continue to face major barriers to the realization of the right to health. Sustainability of quality health care services is challenged by chronic occupation and fragmentation; restrictions on movement have a profound impact on access to health care, including for some of the most vulnerable Palestinian patients. A study completed by WHO this year demonstrates that cancer patients initially denied or delayed permits to access chemotherapy and/or radiotherapy outside Gaza from 2015 to 2017 were 1.5 times less likely to survive in the following six months or more, compared to those initially approved permits. The findings highlight the urgent need for reform to remove access barriers to protect patients from harm.”
Palestinians living under Israeli occupation in the West Bank and Gaza Strip are exposed to high levels of violence. In 2018, 299 Palestinians were killed and 31,723 injured in occupation-related violence, of which the vast majority (87% of deaths and 81% of injuries) occurred in the Gaza Strip in the context of the Great March of Return, which began on 30 March 2018. The public health consequences of violence are severe. Over a half of conflict-affected children may be affected by post-traumatic stress disorder, while the long-term consequences of injuries, with more than 6,000 live ammunition injuries in Gaza alone over the year, put strain on an already overburdened health system. Health staff, too, work at considerable personal risk. In 2018, there were an unprecedented 432 attacks against health care in the West Bank and Gaza Strip. In Gaza alone, three health workers were killed and 570 injured, 41 with live ammunition, while providing care to those injured in Gaza’s Great March of Return.
Zeiad, a first responder with the Palestinian Red Crescent Society (PRCS), was injured with live ammunition at one of the peak times of the demonstrations when there was a huge volume of injuries overwhelming the public hospitals in Gaza. He was taken in a critical condition to the PRCS hospital for emergency surgery. Zeiad stated, “When I remember the events of that day, it makes me very sad. Even us health workers – carrying out our humanitarian work and clearly marked with our PRCS vests – were targeted with live ammunition.”
Mr McGoldrick discussed the humanitarian situation for Palestinians: “The dire humanitarian situation – particularly in the Gaza Strip and for West Bank communities in Area C, East Jerusalem and H2 area of Hebron – has profound implications for people’s health. WHO’s report highlights the health implications of impediments to inadequate access to water and sanitation, high rates poverty, unemployment and food insecurity and insecure housing, demolitions and displacement.”
He expressed concern about ongoing high levels of exposure to violence, including for health workers: “No patient should have to worry about being prevented from accessing essential and lifesaving treatments, whether access to health facilities requiring Israeli-issued permits or access to essential medicines within Palestinian health facilities. No health worker should have to go to work with the fear of being shot at and killed. WHO’s report underlines the immediate need for our collective efforts to strengthen the protection of health care.”
The full report can be found here: Right to health 2018
WHO supports primary health care targeting vulnerable communities in the West Bank
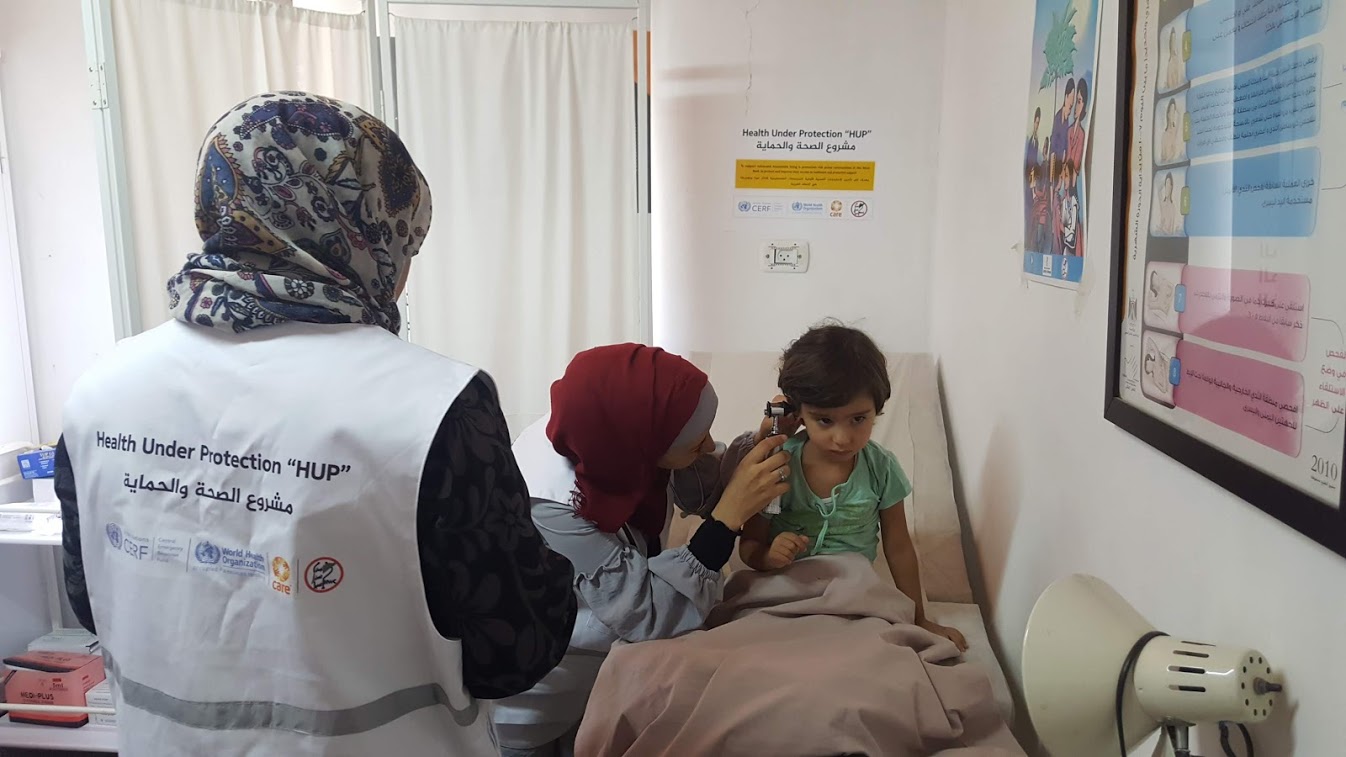 A child gets medical check up at the mobile clinic in Kherbet Zakhariya. Credit: WHO06 September 2019 - The World Health Organization (WHO) supports health partners to deliver primary healthcare services to over 12,000 people in the West Bank through mobile clinics. With funding from the UN Central Emergency Response Fund, two mobile clinics, run by CARE international and Health Work Committee, are providing basic life-saving services and laboratory tests, women’s healthcare, mental health and psychosocial support, family planning services and health education. WHO also supported procurement of medical supplies to help the mobile clinics to work more efficiently and ensure people can access essential medicines needed for treatment and prevention.
A child gets medical check up at the mobile clinic in Kherbet Zakhariya. Credit: WHO06 September 2019 - The World Health Organization (WHO) supports health partners to deliver primary healthcare services to over 12,000 people in the West Bank through mobile clinics. With funding from the UN Central Emergency Response Fund, two mobile clinics, run by CARE international and Health Work Committee, are providing basic life-saving services and laboratory tests, women’s healthcare, mental health and psychosocial support, family planning services and health education. WHO also supported procurement of medical supplies to help the mobile clinics to work more efficiently and ensure people can access essential medicines needed for treatment and prevention.
The mobile clinics reach 19 vulnerable communities in the West Bank. For most of them, this is the only source of receiving much needed health care. A few months ago, residents of Kherbet Zakhariya community were cut off from access to even essential health services and medical supplies. Now, a mobile team visits the village three times a week, one of which is dedicated to women’s health.
“It is critical for everyone in our community to have access to health services. We spent over a year and a half without any mobile clinic coming,” says Mohammad Sa’ed, a community leader of Kherbet Zakhariya. He benefits from the mobile clinics visits himself: “I was not visiting any hospital for check-ups when services were unavailable in our village. When the clinic started operating, they discovered I have high blood pressure and prediabetes. Now I come to the mobile clinics for regular check-ups and to receive prescribed medicines and better nutrition advice - this keeps me in better health.”
Abir Sa’ed brought her 4-year old daughter for a follow-up visit: “Last week my daughter had an ear infection, we came to the clinic for consultation. A doctor provided her with medicine, and she is feeling much better now. Before the clinic started visiting us, we used to go to Beit Fajjar or Bethlehem, which was hard because the transportation is not easy to find. Now, the situation is much better, and we can receive health care quickly.”
People from the community receive text messages about the mobile clinic visit, but often passing of information through word of mouth is more effective. “When we come to the community, people start spreading the message that the mobile clinic arrived,” says Dr Ghandi Al Tamimi, a doctor with one of the mobile clinics. “There are people who live too far or have certain health conditions and cannot come. I call them “the marginalized of the marginalized”. We do home visits for them.”
Each mobile clinic provides around 10-15 consultations a day. Dr Al Tamimi says chronic diseases are the most common among populations they visit.
The mobile clinics also offer women psychosocial support alongside health services to respond to the needs of women affected by gender-based violence and provide information on violence prevention. “In my work, I focus on women, young girls and children who have experienced either physical and/or sexual violence,” says Raihana Mesyef, a psychosocial worker with a mobile clinic. “We have both community meetings, where I provide an overview of violence, its different forms and types and answer most common questions, and one-on-one meetings where a woman can talk about her experience and I can provide advice on how to deal with it.”
Currently, 162,663 people in the West Bank have limited access to primary health care. An estimated 138,000 people in Area C* receive primary health care services through mobile clinics supported by the Ministry of Health and Health Cluster partners, but uncertainties of funding cast doubt over the sustainability of these services. WHO will continue to work with the Ministry of Health and partners to support the provision of essential primary health care services to the most vulnerable communities.
*Over 60% of the West Bank is considered Area C, where Israel retains near exclusive control, including over law enforcement, planning and construction.








