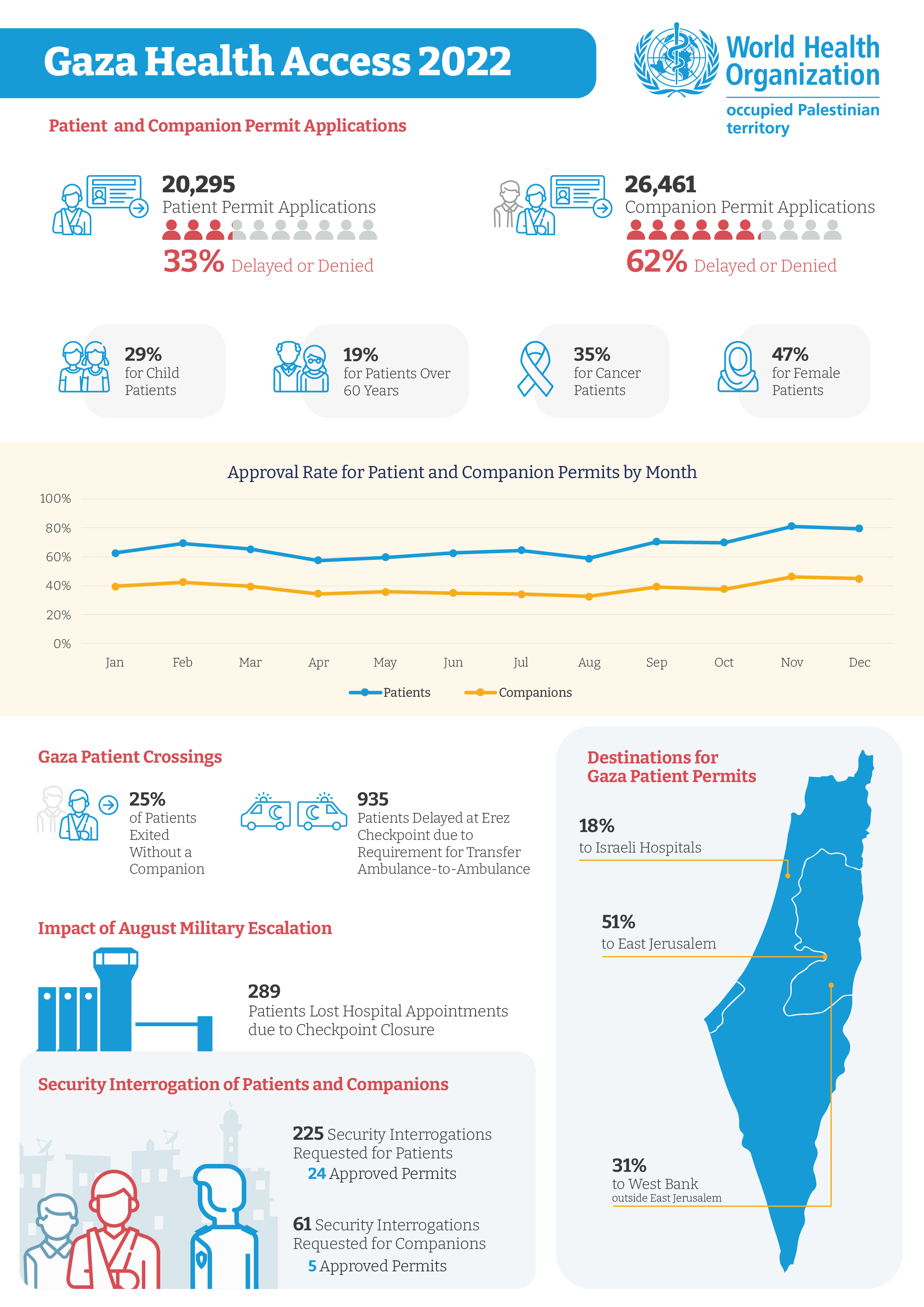
Gaza Health Access 2022
Throughout the year, WHO continued to document the impact of barriers to health access on the Palestinian people in Gaza.
Below are four of the cases documented during 2022:
|
January Saleem, a 16-year-old child with leukaemia, dies after barriers to hospital admission Saleem An-Nawati was 16 years old from Gaza and had acute leukaemia diagnosed in late 2021. He was initially referred for an appointment at An-Najah University Hospital in Nablus in the West Bank on 28 November 2021, but he received no definitive response to his permit application in time for his appointment. Saleem was delayed a permit to reach treatment on two further occasions, for appointments at An-Najah Hospital on 6 and 19 December ..read more |
 |
|
March Gaza child dies following repeated permit delays by Israel Fatma Al-Masri was a 19-month-old girl from Khan Younis in the Gaza Strip. She died on 25 March 2022 after she was delayed access to lifesaving cardiac surgery for nearly three months. Fatma was born with a congenital heart condition known as an atrial septal defect. She needed curative surgery at Makassed Hospital in East Jerusalem and was required by Israel to obtain a permit to reach her hospital appointment. Her family applied three times for permits to reach hospital appointments on 28 December 2021, 13 February 2022, and 5 April 2022... read more |
 |
|
May 5-year-old Ahlam repeatedly delayed access to a critical operation for her hearing Ahlam is a 5-year-old girl born in Beit-Lahia in the north of the Gaza Strip. Since she was six months old, Ahlam’s family noticed she was not as responsive as other children her age and suspected that a problem with her hearing. They took her to two charitable organizations in the Gaza Strip, Atfaluna and Hamad Hospital in Gaza City, who examined her hearing and diagnosed Ahlam with partial hearing loss.. read more |
 |
|
July Ahmed, a patient with cancer, delayed critical follow up for four months Ahmed is 39 years old and from the Gaza Strip. He was diagnosed with cancer in his right parotid gland in 2013, receiving surgery and treatment in Egypt. In 2016, doctors found a recurrence of his cancer and he had further surgery in 2017 at Assuta Hospital in Tel Aviv. There, Ahmed received medicines, radiotherapy and chemotherapy to increase the chances of being successfully treated and since then has needed regular follow up, including medical imaging (PET scans) not available in the Gaza Strip... read more |
 |
Scaling-up Mental Health Services in Palestine
 Nurse Ibrahim checks on a patient in the ICU, European Gaza Hospital
Nurse Ibrahim checks on a patient in the ICU, European Gaza Hospital
“Seeing someone so young attempt to take their own life is heart-breaking. Though we work in a tough environment, witnessing such suffering never gets easy. Sadly, this is not our first such case,” says Ibrahim, ICU Nurse at the European Gaza Hospital.
Recently, he has been caring for a 19-year-old male who was admitted to the ICU after attempting suicide.
Ibrahim and other health workers treating the patient understand that recovery will be long and hard. Medicines are only one part of the treatment and will need to be complemented with extensive mental health support to help him recover and reintegrate into his life.
“These incidents don’t just happen because someone had one bad day. There is always a deeper reason. Something is eating them from the inside. It’s usually a sign of mental health challenges the individual might be facing,” says Ibrahim.
Over the last few days, he’s built a special bond with the patient, and his empathy and understanding have helped him feel comfortable and express his feelings. This has been instrumental in identifying the mental health challenges the patient is facing, which are at the root of his problems.
“He’s been suffering from severe depression and anxiety for some time. Unfortunately, he suffered in silence and alone. When it got too much to bear, he tried to take his own life. His worries stem from sheer economic desperation and hopelessness. He’s not been able to find a job and support his family,” says Ibrahim.
Besides giving him the daily dose of medicines and injections, Ibrahim is also bringing him hope. He is playing a crucial role in the patient’s mental healing by providing initial psychological support and offering a safe space to talk and process the ordeal he has experienced. The patient will be referred to a specialist for further support once he is ready to be discharged.
Ibrahim is one of 300 health workers from Gaza and the West Bank trained by WHO on the Mental Health Gap Action Programme (mhGAP) Intervention Guide (2.0), with support from The Big Heart Foundation.
WHO’s mHGAP rollout includes integrating mental health care into primary and secondary health services by training non-specialist health workers to identify, support, and treat mental health conditions. This approach addresses multiple barriers to accessing mental health services in Palestine, such as lack of trained staff, limited facilities, poor quality of services, affordability, under-resourcing, stigma, and discrimination.
Addressing the Gap
Strengthening the skills of non-specialist health workers contributes to reducing the treatment gap and scaling-up up mental health services by making them more accessible as people can access services closer to home more easily. This also eliminates the potentially prohibitive costs of seeking specialist care in distant locations, making it a feasible, affordable, and cost–effective solution, especially for low- and middle-income countries. Additionally, it allows for treatment in a familiar environment, where people can maintain support networks, employment, education, and other activities while receiving care, which facilitates recovery.
For most common conditions, integrated care by primary and secondary care staff trained in mental health can be preferable to specialist care because it helps to reduce stigma and discrimination.
For Ibrahim, the training has helped him improve the quality of health care delivery to patients.
“Since receiving the training, I am much more aware that physical and mental health problems can often be treated simultaneously. This is a new way of working for me and is helping me understand and treat my patients better. After all the mind and body are very closely linked, one can’t do well without the other, says Ibrahim.
Extending support to care givers
The benefits of the training have gone beyond just helping patients for Abdullah, a Paediatric Nurse at the Emergency Department of the European Gaza Hospital. A few months ago, he received a child suffering from gastroenteritis. While treating his young patient, Abdullah was alarmed by the stress the child’s mother was exhibiting.
“All mothers get extremely stressed when it comes to their child’s health. I told her that her son would be fine and required routine treatment, but she kept sobbing uncontrollably. This was not normal at all”, he recounts.
 Nurse Abdullah treats a patient at the Emergency Ward of the European Gaza Hospital
Nurse Abdullah treats a patient at the Emergency Ward of the European Gaza Hospital
He immediately recognized that she is likely suffering from underlying mental health issues and knew he had to help her. After treating the child, he conducted a mental health screening, and it quickly became evident why her child’s sickness was stressing her so much.
“She had recently lost her older child due to ill health and was still suffering from trauma,” says Abdullah.
He provided initial psychological support and recommended that she seek help and speak to her family, so her condition does not worsen.
While the need for mental health services in Palestine remains high, health workers trained on mHGAP will be vital in bridging the gap and supporting many people who could have gone undiagnosed. Plans to cascade and make the mHGAP training accessible to more health workers are being developed by WHO as part of the overall efforts to advance universal health coverage.
21-year-old Musaab repeatedly denied access to cancer care
Musaab is 21 years old and in his third year of study at university in Nablus, in the north of the West Bank.
In the summer of 2022, Musaab was diagnosed with a cancer called a synovial sarcoma in his left ankle. To confirm his diagnosis and to guide the best approach to his treatment, he was referred to Makassed Hospital in East Jerusalem for bone biopsy in June 2022, for an appointment on 6 July. Because Musaab has a West Bank identity card, he was required by Israel to obtain a permit to access East Jerusalem. He applied three times for a permit for his initial hospital appointment and was denied each time. The family were told that Musaab and his companions (different family members for each application) had been denied on security grounds. He eventually received the bone biopsy at Istishari Hospital in Ramallah, which meant he didn’t require a permit for his appointment.
Musaab was in Israeli prison from July 2020 to January 2021. It was during his detention that he started to feel pain in his left ankle. “He was given paracetamol, which didn’t help,” his father said. “He has been suffering a lot. He told me sometimes he felt as if his bone was being crushed.”
After his diagnosis, doctors considered to refer Musaab to Augusta Victoria Hospital, the major Palestinian cancer centre, in East Jerusalem. However, because he had been denied a permit to East Jerusalem previously, the doctors instead referred him to An-Najah University Hospital in Nablus, which meant he didn’t require an Israeli permit to reach care. Musaab received the chemotherapy he needed before he would undergo an operation. By November 2022, he was ready for surgery and his family applied for permits for him to reach Assuta Hospital in Tel Aviv. They wanted a private surgical consultation, to see the extent to which it would be possible to salvage Musaab’s leg. His three applications for a permit to reach two different appointments at the hospital were again denied.
Musaab’s father spoke with a doctor at Makassed Hospital to get advice on how to proceed. “He told me that repeatedly delaying surgery might cause bone erosion requiring leg amputation, God forbid.” The family had lost hope of obtaining a permit to access East Jerusalem, so Musaab’s father went to the Services Purchase Unit (SPU) of the Ministry of Health in Ramallah to request a change of destination to Jordan.
“Musaab and I travelled [to the Jordan border, the King Hussein Bridge] on 12 December. At the Bridge, we were asked to sit and wait. We waited about an hour, then an Israeli officer came out and asked us to go back to the West Bank. He said that we were both denied for security reasons. We refused to leave, and I requested to see the Mukhabarat [intelligence] officer. I insisted, telling them that my son has cancer and that he has the right to access health care. I asked them to let him go. After waiting another four hours, they decided to allow Musaab to cross to Jordan, but they made me return.” Although he crossed, Musaab missed his appointment at King Hussein Cancer Center in Amman, which had been for 12:30pm that day. The next available appointment was a week later.
“My son needs me beside him during these difficult times. We should see the doctor together so we can discuss the different options to help Musaab decide about the surgery.” Musaab’s father appealed through nongovernmental organizations Physicians for Human Rights Israel and Hamoked, as well as through a private lawyer, to get approval to travel to Jordan. He said, “This is so inhumane. How can this happen in any place in the world? Why are they blocking me from accompanying my son? I just want to hold his hand when he goes for surgery.”
Musaab is currently undergoing medical assessment in preparation for surgery. His mother crossed to Jordan on 20 December. His father is still hoping to join him1
Making health care services faster and easier for patients
10 January 2023 – Khetam, a mother of 2, has only brought one of her daughters to the primary health centre, though both are sick and in need of medical attention.
Her younger daughter has a very high fever and weakness. Khetam has had to prioritize her treatment today.
 Khetam and her daughter at the Jabaliya Health Centre, Gaza Strip
Khetam and her daughter at the Jabaliya Health Centre, Gaza Strip
“If I brought my other daughter too, we would have had to spend more time waiting to see the doctors, doing the paperwork, and running from one department to the other. If I forgot any of their medical notes, x-rays, or prescriptions, I’d have to spend even more effort going back and forth in trying to arrange these documents to get the treatment and medicines,” Khetam says.
 Patients queue outside the doctor's office, Jabaliya Health Centre, Gaza Strip
Patients queue outside the doctor's office, Jabaliya Health Centre, Gaza Strip
In the past, she has sometimes waited hours to get the administrative paperwork done only to then be met with long queues outside the doctor’s office, which often end in bitter disagreements between patients over who’s turn it is.
For many like Khetam, this makes seeking health care for even the simplest of issues quite daunting, time-consuming and tiring.
A pleasant surprise
Today, Khetam’s visit to the health centre has been unlike in the past. She had blocked a few hours from her day but is pleasantly surprised at how quickly she has been able to see the doctor and get the medicines for her daughter.
“I didn’t have to spend ages getting the paperwork done, I didn’t have to wait a long time to see the doctor and now I’m on the way to the pharmacy without having to carry any files or prescriptions. The doctor has already sent it to them online. If I knew the system had changed and is so much quicker, I would have brought my other daughter for treatment too,” she says.
Change is under way at the Jabalia, Deir Al-Balah, and Sheikh Redwan primary health care centres in the Gaza Strip, which cover a catchment population comprising 180 000 people. With support from the Big Heart Foundation, WHO has facilitated expansion of the electronic health information system at these 3 centres. The system has already been introduced at 24 primary health care centres by the Gaza Ministry of Health, and other health partners.
 Dr Abdelkarim looks at a patient's history on the new electronic health information system, Jabaliya Health Centre, Gaza
Dr Abdelkarim looks at a patient's history on the new electronic health information system, Jabaliya Health Centre, Gaza
Change is being felt by everyone
The new paperless system has drastically streamlined patient information management and improved data flow between all departments, allowing seamless connectivity. Everything from the moment patients enter the health centre until they leave is now being managed through a unified system. This includes administrative paperwork for registering patients to receive treatment.
 Riyad, who is suffering from an infection caused by stones in the urinary tract has come to the health centre for a check-up. His visit has gone smoothly.
Riyad, who is suffering from an infection caused by stones in the urinary tract has come to the health centre for a check-up. His visit has gone smoothly.
“I came in, was given my number and saw the doctor without having to wait. Now, I’m on my way to the laboratory to get some tests. The doctor has already sent the test request to the laboratory, and I do not need to carry any papers there,” says Riyad.
By eliminating the need for patients to carry files and allowing better management of patient flow, thus limiting crowding, the new system is ensuring delivery of faster, hassle-free, and better quality health care services.
Improvements are also being felt by health workers.
“I used to have to do volumes of paperwork for each patient, but the system has really simplified my work and made data recording more accurate and reliable. It’s very easy to pull up someone’s medical history even if they lose previous reports,” says Dr Hesham, Family Doctor, Jabaliya Health Centre.
 Dr Hesham shows the volume of paperwork he had to fill prior to the new electronic information system being introduced
Dr Hesham shows the volume of paperwork he had to fill prior to the new electronic information system being introduced
Physicians can now record patient history, display test results, write prescriptions, order tests, receive clinical reminders, and print instructions, through one platform. The real-time, patient-centred records can then be made available instantly to other departments as needed, without the need for extensive paperwork, limiting human error.
 Since August 2022, approximately 119 health workers across the 3 primary health care centres have been trained in using the electronic health information system
Since August 2022, approximately 119 health workers across the 3 primary health care centres have been trained in using the electronic health information system