R. Kishk,1 H. Aboul Atta,1 M. Ragheb,2 M. Kamel,1 L. Metwally 1 and N. Nemr 2
تحديد الأنماط الجينية لذرية فيروس التهاب الكبد البائي الخفي لدى المصريين المصابين بالتهاب الكبد الوبائي سي المزمن
رانيا محمد كشك، حسن نصر الإسلام أبو العطا، مصطفى محمد راغب، محمود كامل منصور، لبنى أحمد متولي، نادر نمر
الخلاصة: إن العدوى بفيروس التهاب الكبد المزمن "سي" المصحوبة بفيروس التهاب الكبد البائي الخفي، يرافقها زيادة في خطر الإصابة بالتهاب الكبد، وتليف الكبد، وسرطانة الخلايا الكبدية. وتهدف هذه الدراسة إلى تحديد معدل انتشار العدوى بفيروس التهاب الكبد البائي الخفي بين المرضى المصريين المصابين بالتهاب الكبد الوبائي "سي"، وتحديد الأنماط الجينية، والطفرات الجينية السطحية لفيروس التهاب الكبد البائي "سي"، وتأثير العدوى المشتركة على الاستجابة المبكرة للمعالجة. وقد أدرج في الدراسة 162 مريضاً مصاباً بفيروس التهاب الكبد "سي" المزمن من مستشفى الإسماعيلية للحميات بمصر، ممن كانوا سلبيين لمستضد فيروس التهاب الكبد البائي، وتم إجراء تقييم سريري مع اختبارات بيولوجية كيميائية وهيستولوجية وفيروسية لجميع المرضى. وتم اكتشاف دنا فيروس التهاب الكبد البائي في مصول ثلاثة مرضى من بين 40 مريضاً إيجابياً للضد اللبي لفيروس التهاب الكبد البائي. وقد استجاب هؤلاء الثلاثة للمعالجة التوليفية في الأسبوع الثاني عشر للمعالجة. وتوقف واحد فقط منهم عن المعالجة في الأسبوع 24. ولم يكتشف سوى النمط الجيني D لفيروس التهاب الكبد البائي لدى هؤلاء المرضى مع غياب أي طفرة محددة في هذه المستفرَدات.
ABSTRACT Chronic hepatitis C virus (HCV) infection combined with occult hepatitis B virus (HBV) infection has been associated with increased risk of hepatitis, cirrhosis and hepatocellular carcinoma. This study aimed to determine the prevalence of occult HBV infection among Egyptian chronic HCV patients, the genotype and occurrence of surface gene mutations of HBV and the impact of co-infection on early response to treatment. The study enrolled 162 chronic HCV patients from Ismailia Fever Hospital, Egypt, who were HBV surface antigen-negative. All patients were given clinical assessment and biochemical, histological and virological examinations. HBV-DNA was detectable in sera from 3 patients out of the 40 patients who were positive for hepatitis B core antibody. These 3 patients were responsive to combination therapy at treatment week 12; only 1 of them had discontinued therapy by week 24. HBV genotype D was the only detectable genotype in those patients, with absence of “a” determinant mutations among those isolates.
Caractérisation du génotype des souches du virus de l’hépatite B occulte chez des patients égyptiens atteints d’hépatite C chronique
RÉSUMÉ L’infection chronique par le virus de l’hépatite C associée à une infection occulte par le virus de l’hépatite B a été associée à un risque accru d’autres hépatites, de cirrhose et de carcinome hépatocellulaire. La présente étude visait à déterminer la prévalence des infections occultes par le virus de l’hépatite B chez des patients égyptiens atteints d’une hépatite C chronique, le génotype et la survenue des mutations génétiques du virus de l’hépatite B et l’impact d’une coïnfection par le virus de l’hépatite B sur la réponse précoce du patient au traitement. L’étude a recruté 162 patients atteints d’une hépatite C chronique dans l'établissement Fever Hospital d'Ismaïlia (Égypte), ayant des résultats négatifs pour l’antigène de surface du virus de l’hépatite B. Tous les patients ont été soumis à un examen clinique ainsi qu'à des analyses biochimiques, histologiques et virologiques. L’ADN du virus de l’hépatite B a été dépisté dans le sérum de trois patients sur 40 dont les résultats étaient positifs pour l’anticorps nucléocapsidique de l’hépatite B. Ces trois patients ont répondu au traitement combiné à la Semaine 12 du traitement ; seul un patient a interrompu le traitement à la Semaine 24. Le génotype D du virus de l’hépatite B était le seul détectable chez ces patients, et aucune mutation du déterminant « a » n’a été observée dans les isolats.
1Department of Microbiology; 2Department of Endemic and Infectious Diseases, Faculty of Medicine, Suez Canal University, Ismailia, Egypt (Correspondence to M. Kamel:
Received: 23/07/12; accepted: 14/10/12
EMHJ, 2014, 20(2): 130-138
Introduction
Occult hepatitis B virus (HBV) infection can be defined as a particular form of HBV infection where patients are negative for hepatitis B surface antigen (HBsAg) while at the same time being positive for HBV DNA in the liver tissue (and in some cases also in the serum). This clinical entity was suspected as far back as the 1970s, when there were reports of transmission of HBV infection through blood transfusion from donors with serology suggestive of past HBV infection and clearance of HBsAg [1,2].
Occult HBV infection seems to be related to the host’s immune response and probably the effect of co-infection with other agents [1]. Studies have shown that occult HBV infection is more prevalent in populations co-infected with hepatitis C virus (HCV) or human immunodeficiency virus (HIV). A prevalence of occult HBV infection of 33% was noted in an Italian study of a group of individuals co-infected with HCV, whereas the rates were 70% to 95% in Japanese studies [3]. In Egypt El Sherif et al. found that chronic HCV patients negative for HBsAg and positive for antibodies to hepatitis B virus core antigen (anti-HBc) had more severe liver disease compared with patients negative for HBsAg and hepatitis B core antibody (HBcAb). Although HBV-DNA in the serum was detected in 22.5% of anti-HBc-positive chronic HCV patients, it was not detected in any of anti-HBc-negative chronic HCV patients [4].
Several possible mechanisms have been hypothesized for the pathogenesis of occult HBV infection and the condition is probably multifactorial [5,6]. Although the negativity of HBsAg among individuals with occult HBV infection remains controversial, some studies have reported that it could be due to viral genome variability, which results in suppressed S protein expression or viral replication; other studies have reported that it could be due to surface gene mutants (S mutants) in a variety of patient groups with variable rates of occurrence [3].
Due to the apparent increase in prevalence of S mutants and limited data regarding these mutations in patients with occult HBV infection this study aimed to elucidate the prevalence of occult HBV infection among Egyptian patients with chronic HCV and to determine the genotype and occurrence of surface gene mutations of HBV among those patients. The impact of HBV co-infection on the patient’s early response to treatment was also investigated.
Methods
Study design and population
This study was conducted on 162 patients with chronic HCV infection treated with pegylated interferon and ribavirin (PEG-IFN/RBV) in Ismailia Fever Hospital. The study was approved by the ethics committee of Suez Canal University. The diagnosis of HCV was done by detection of serum anti-HCV antibody and confirmed by detection of serum HCV RNA. All the study population was subjected to the clinical assessment, biochemical assessment and pathological examination of liver biopsy.
Laboratory tests
Serological markers
Serological status was investigated by the 3rd-generation enzyme immunoassay method using commercially available kits for anti-HCV (BioTina GmbH), HBsAg (Diasorin) and anti-HBcAg total (CTK Biotech).
Determination of HBV DNA load by real-time PCR
The HBV/DNA was extracted from 200 µL of serum samples negative for HBsAg using the QIAamp DNA Minikit (Qiagen Inc.), and re-suspended in 100 µL of a storage buffer provided by the kit manufacturer. The extracted samples were tested for the presence of HBV DNA using a real-time polymerase chain reaction (PCR) system (Applied Biosystems 7500) to determine the viral load by using the following oligonucleotides:
primer F: SF2: 5′-CTTCATCCTGCTGCTATGCCT-3′
primer R: SR2: 5′-AAAGCCCAGGATGATGGGAT-3′
probe: SP2: FAM-ATGTTGCCCGTTTGTCCTCTAATTCCAG-TAMRA
The 25 µL reaction mixture volume contained 0.5 µL of each primer (10 pmol/µL) and the probe (SP2, 10 pmol/µL), 6 µL water (PCR-grade), 5 µL of DNA template and 12.5 µL of the TaqMan universal PCR master mix (Applied Biosystems). To allow quantification of HBV genotype Aa clones were used as external standards.
Cycling conditions were 10 min. at 95 °C, 95 °C for 15 s, and 60 °C for 1 min. for 45 cycles. Fluorescence acquisition was taken once per cycle using FAM™ as a reporter dye and TAMRA™ as a quencher dye.
Nested PCR amplification of S gene
The S gene of the HBV genome (681 bp) was amplified using the following primers. For the first PCR (nucleotide positions 18–989):
forward primer (IS1): 5′-AAGCTCTGCTAGATCCCAGAGT-3′
reverse primer (HS4R): 5′-CATACTTTCCAATCAATAGG-3′
The 25 µL reaction mixture volume contained 1 µL of each primer (10 pmol), 13.25 µL water (PCR-grade), 5 µL of DNA template, 0.25 µL of the Taq polymerase, 2 µL DNTPs and 2.5 µL buffer. Cycling conditions were 7 min. at 96 °C, 96 °C for 45 s, 55 °C for 45 s and 72 °C for 1 min. for 45 cycles.
For the second PCR (nucleotide positions 414–989):
forward primer (SB1): 5′-TGCTGCTATGCCTCATCTTC-3′
reverse primer (HS4R): 5′-CATACTTTCCAATCAATAGG-3′
The 25 µL reaction mixture volume contained 1 µL of each primer, 17.3 µL water (PCR-grade), 1 µL of DNA template, 0.25 µL of the Taq polymerase, 2 µL DNTPs and 2.5 µL buffer. Cycling conditions were 7 min. at 96 °C, 96 °C for 45 s, and 55 °C for 45 s and 72 °C for 45 s for 45 cycles.
Sequencing of the amplified products
The amplified products were sequenced using ABI PRISM® 3100 and BigDye™ DNA automated sequencer (Perkin–Elmer Applied Biosystems) according to the manufacturer’s protocol. The sequences were aligned together with the ClusalW software programme [7].
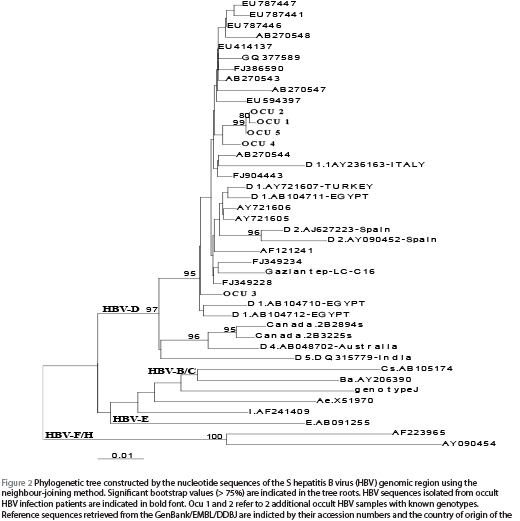
The phylogenetic tree was constructed using the neighbour-joining method with Tamura-Nei’s distance correction model using the online hepatitis virus database (http://s2as02.genes.nig.ac.jp/) [8]. The bootstrap values were determined on 1000 database re-sampling tests. The sequences of other HBV isolates used for the construction of the phylogenetic tree were retrieved from the National Institutes of Health GenBank® European Molecular Biology Laboratory (EMBL) and DNA DataBank of Japan (DDBJ) sequence databases and were indicated in their accession numbers. The new nucleotide sequences data that were reported in this manuscript will appear in the GenBank/EMBL/DDBJ sequence database with accession numbers.
Statistical analysis
Statistical analysis was performed with the Fisher exact probability test and the independent t-test for the continuous variables using the SPSS, version 16 software package. P-values (2-tailed) < 0.05 were considered to be statistically significant.
Results
Baseline data
This study was conducted on 162 patients with chronic HCV infection in Ismailia Fever Hospital. Their ages ranged between 19 and 59 years [mean 41.9 (standard deviation 10) years] and most patients were aged > 30 years (83.4%). Nearly two-thirds were male (62.3%). The mean HCV RNA level in sera was 791 717 (SD 3 083 970) IU/mL. At a cut-off of ≤ 800 000 IU/mL, 83.2% of patients showed low viraemia.
Prevalence of exposure to HBV
The study revealed that previous exposure to HBV infection was high (24.7%) in Egyptian patients with chronic HCV. The prevalence of HBcAb positivity showed a highly statistically significant increase with age of patients, being 3.7% in patients aged ≤ 30 years, 14.7% in those > 30–45 years and 40.3% in patients > 45 years (P = 0.001), with no significant association with sex or residence. Among HBcAb-positive patients, further testing for HBV DNA before initiating antiviral therapy revealed 3 patients with occult HBV (7.5%). HBV DNA loads were 5700, 7200 and 138 000 IU/mL respectively in the 3 people. All were males, from rural areas and aged 26, 49 and 58 years respectively (mean 44.3 years). None of the 3 showed cirrhosis, but 2 patients had mild fibrosis, 1 of them with non-cirrhotic fibrosis, with a mean stage of 2.
The demographic and histological data of patients with chronic HCV infection according to the presence or absence of occult HBV infection are shown in Tables 1 and 2. There were no significant differences between the 2 groups in age, sex or area of residence, or by hepatitis activity index or fibrosis scores.
Regarding liver enzymes, in dual-infected patients 2 patients had alanine transaminase (ALT) level above the upper limit of detection (48 and 64 U/L respectively) and 1 patient had aspartate aminotransferase (AST) above the upper limit of detection (56 U/L). All the 3 patients had alpha-fetoprotein (AFP) < 10 ng/mL. Furthermore, histopathology revealed low grades of activity in all: A1 in 2 patients and A2 in 1 patient, with a mean activity of 4.3.
When we classified patients according to exposure to HBV as well as presence of occult HBV DNA in sera, the median HCV RNA load was highest in patients with occult HBV infection followed by HCV patients previously exposed to HBV (positive to anti-HBc with no detectable DNA) and lowest in patients not exposed to HBV (400 000, 252 000 and 101 500 IU/mL respectively) (P = 0.053).
Discontinuation and response to therapy
Up to week 12, 10 patients (6.2%) had discontinued therapy due to either side-effects, such as anaemia and thrombocytopenia, or to unexplained reasons. By intention-to-treat analysis, the majority of patients 134 (82.7%) exhibited early virological response (EVR) and 18 (11.1%) were non-responders. Although the EVR response rate was similar in HBcAb-positive and -negative patients (82.5% and 82.8% respectively), the former group showed a slightly lower non-responder rate. This difference, however, was not statistically significant (Fisher exact test, P = 0.34).
At week 24, another 10 patients (7.5%) had discontinued therapy, 115 (85.8%) showed no viraemia (responders) and 9 (6.7%) had viraemia (non-responders). Among the HBcAb-positive patients, 75.0% were responders to combination therapy, while only 5.0% were non-responders. On the other hand, 69.7% of HBcAb-negative patients were responders to therapy and only 5.7% were non-responders, with no statistical difference between the 2 groups (Fisher exact test, P = 0.58).
Therefore, overall at week 24, 20 patients (12.3%) had discontinued therapy, 115 (71%) were responders and 27 (16.7%) were non-responders, with no significant difference between the groups (Table 3), although HBcAb-positive patients showed higher responder rates and lower rates of discontinuation compared with HBcAb-negative patients.
In the 3 dual-infected patients, all patients had low HCV RNA level of viraemia (≤ 800 000 IU/mL); their viral loads were 5610, 75 000 and 260 000 IU/mL (mean 113 536 IU/mL). All 3 patients were responders to PEG-IFN/RBV therapy at week 12 but only 1 of them discontinued therapy at week 24 (Table 4).
Molecular analysis
Nested PCR
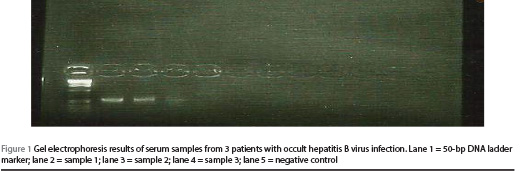
Figure 1 shows the gel electrophoresis results for the 3 samples from patients with occult HBV.
Molecular evolutionary analysis of samples from patients with occult HBV
Partial HBV genome sequence of the S region was done for all 3 samples from patients with occult HBV by the nucleotide sequences of the S HBV genomic region [nt (485–976) = aa (109–224)]. Sequencing results were used for phylogenetic analysis and genotyping. Neighbour-joining analysis determined that all the examined HBV genomes retrieved from chronic HCV patients negative for HBsAg were of genotype D. Reference sequences were retrieved from the GenBank/EMBL/DDBJ (Figure 2).
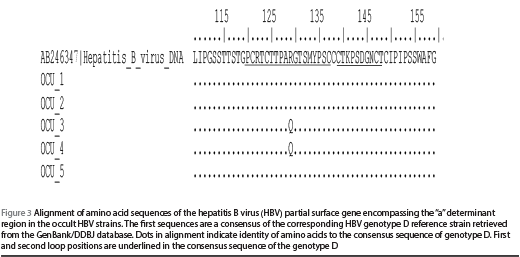
Mutations in the “a” determinant region
The available nucleotide sequences spanning the S gene of HBV isolates from the 3 occult hepatitis B infection samples were translated into amino acids and aligned in correspondence to the reference sequence. There was no amino acid mutation in the “a” determinant region of the S gene of HBV genome isolated from occult HBV infection strains (Figure 3).
Discussion
Occult HBV infection is defined as detectable HBV DNA in peripheral blood or liver by sensitive nucleic acid detection methods in patients without detectable HBsAg. Although the mechanism and clinical implications have not been elucidated clearly, occult HBV infection has its own risk of disease transmission and may contribute to acute exacerbation and development of HBV-associated diseases such as hepatitis, cirrhosis and hepatocellular carcinoma [1].
This study included 162 patients with chronic HCV; nearly two-thirds of our patients were males (62.3%) and the majority of them (83.4%) were > 30 years old. This pattern of age and sex agrees with another study from Egypt reported by Emara et al. [9]. On other hand, the mean age of our patients was higher than that reported in a similar series in Germany and the United States of America [10,11]. The difference in age could be related to the presence of an active surveillance system that could discover infected individuals at an earlier age. In Egypt, there is currently no ongoing surveillance for chronic HBV and HCV.
The prevalence of occult HBV infection is quite variable depending on the level of endemic disease in different parts of the world, the different assays employed in routine serological or nucleic acid test screening and the different populations studied [1]. In this study, occult HBV infection was found in 3 out of 40 anti-HBc positive HCV patients. All were males, from rural areas, had low level of viraemia (≤ 800 000 IU/mL) and their liver histopathology showed non-cirrhotic fibrosis and minimal activity. In addition, all were EVR, i.e. responders to combined PEG-IFN/RBV at week 12, and had normal AFP levels. Although most of these differences were not statistically significant, occult HBV infection was associated with higher median of stages of fibrosis and grades of activity, lower viraemia and good response to antiviral therapy.
Previous studies have pointed out to the role of occult HBV infection in accelerating the evolution of cirrhosis in patients with chronic hepatitis. However, given the data available in our study we were unable to reach any conclusions to this end, and this can probably be attributed to the lower number of patients with occult HBV infection (only 3 cases), the young age of 1 of the 3 patients of occult HBV infection (26 years) and lastly because HBV DNA was not tested in the sera of anti-HBc-negative chronic HCV patients in this study.
The prevalence of occult HBV infection (7.5%) was similar to a French series of chronic HCV cases that were not related to anti-HBc [12]. In a recent study in Sharqiya governorate of Egypt, the prevalence of occult HBV infection was 3.9% in patients with chronic HCV, 11.1% in anti-HBc positive cases and 2.9% in anti-HBc negative cases [9]. Occult HBV infection was also found in 16% of patients with HCV-related chronic liver disease including liver cirrhosis and chronic hepatitis; all were anti-HBc-positive [4].
In this study, the HBV load was < 104 IU/mL in 2 patients (5700 and 7200) and high (138 000) in 1 patient. In the 3 cases with occult HBV infection in our study, 2 had HBV DNA and HCV RNA load < 104 IU/mL (5700 and 7500 respectively for the first patient; 7200 and 5600 respectively for the second patient). In both cases their baseline AST levels were normal and 1 showed mildly elevated ALT. The third patient had viral loads exceeding 105 IU/mL for HCV RNA (260 000) and HBV DNA (138 000), with elevation of both ALT (64 IU/L) and AST (56 IU/L).
In our study, the mean ALT and AST levels were slightly higher in patients with dual HBV and HCV but with no statistically significant difference between the groups. Fukuda et al. also reported higher serum ALT levels in occult HBV infected patients, although their study failed to demonstrate a significant correlation [13]. But Fujiwara et al. reported fluctuations of HBV DNA load in serial assays and that occult HBV infection was not detected continuously [14]. In some of their patients, HBV DNA appeared after elevation of ALT, reflecting the enzyme release from the liver. The authors added that more sensitive quantitative assays might reveal precisely the manner in which the viral load changes [14]. In the present study, the outcomes of therapy after 24 weeks showed no association with anti-HBc status. In anti-HBc-positive patients, a slightly higher responder rate (75.0%) and similar discontinuation rate (12.5%) were found compared with anti-HBc negative patients (69.7% and 12.3% respectively); however this difference was not statistically significant. Similar findings were reported by Emara et al., i.e. a responder rate of 55.6% and 43.8% in anti-HBc-positive and -negative patients respectively, with no significant difference [11]. In this study, all patients with occult HBV infection showed EVR (at week 12), however, by week 24, 1 discontinued therapy and 2 were responders. However, the small number of cases with occult HBV infection limits the conclusions that can be drawn from the data. No significant association has been reported between response and occult HBV infection status in patients with chronic HCV treated with PEG-IFN/RBV [15].
In contrast, low response rates were recorded in chronic HCV patients with occult HBV infection under standard interferon monotherapy [16]. In a retrospective analysis of 140 patients treated for chronic HCV by PEG-IFN/RBV there was no association between HBV markers (HBV DNA, anti-HBc, and anti-HBs antibodies) and disease severity or response to treatment [17].
The impact of occult HBV co-infection on anti-HCV therapy response also remains controversial. Indeed, some studies with combination therapy failed to find any difference, but they only treated a small number of patients with occult HBV infection and, therefore, their data cannot be considered conclusive and would need to be confirmed by larger studies [15]. On the opposite, Marcellin reported that the rate of sustained virological response to IFN/RBV combination was significantly higher in HCV mono-infected than among co-infected patients [18]. The authors concluded that occult HBV infection may play a key role in the poor response of chronic HCV to combined IFN-α and RBV therapy irrespective of HCV genotype.
In our study, there was no amino acid mutation in the “a” determinant region of the S gene of HBV genome isolated from occult HBV infection strains. Interestingly, Khattab et al. found, mutations in the “a” determinant of the S gene, including the G145R mutation, in all their 4 co-infected patients, which may have explained the lack of detection of serum HBsAg by conventional serology assays [12]. This is consistent with data showing that these mutations may affect the binding of anti-HBs monoclonal antibodies to the “a” determinant of the surface protein [19]. Moreover, quantification of HBV DNA by a real-time PCR assay also showed relatively low levels of circulating virus, which may have contributed to the lack of detection of HBsAg in serum. The fact that HBV DNA was detectable with 2 different PCR methods at several time points argues for the specificity of the PCR amplified DNA sequences.
It is worth mentioning that all the HBV DNA levels mentioned in this study were determined before initiating PEG-IFN/RBV therapy.
Our study had some limitations. First—although both viruses are endemic in Egypt— the number of cases of occult HBV infection in chronic HCV patients in our study was small. This could probably be attributed to testing serum samples rather than liver biopsy specimens; additional cases of occult HBV infection could have been detected in liver specimens. Secondly, it is now known that up to 20% of individuals with occult HBV are negative for all markers of past HBV infection aside from HBV DNA, so some cases of occult HBV could have been missed in our study as we only screened anti-HBc positive patients for HBV DNA. Nevertheless, it is known that the HBV DNA detection rate is highest in subjects who are anti-HBc-positive and these individuals are more likely to be infectious. Finally, we need to complete the whole S gene sequencing to determine the presence of any mutation in the pre-S1 or pre-S2 regions.
In conclusion, occult HBV infection was uncommon in chronic HCV patients in this study. The clinicopathological features and the virological response rate after combined PEG-IFN/RBV therapy might be similar between patients with HCV mono-infection and those with dual occult HBV/HCV infection. The serum HBV DNA levels in occult HBV and HCV dual infection were low and the patients responded to combined PEG-IFN/RBV therapy. It is concluded that exposure to HBV or occult HBV infection in patients with chronic HCV does not affect the outcome of therapy at weeks 12 and 24. Phylogenetic analysis revealed that all the occult HBV cases were genotype D with no detectable mutations in the S region of the S gene.
Acknowledgements
We would like to acknowledge Dr Abeer ElKady for her contribution in the molecular sequencing of sera of patients with occult HBV infection in the laboratory of Nagoya City University Graduate School of Medical Sciences, Kawasumi, Mizuho, Nagoya, Japan.
Funding: None.
Competing interests: None declared.
References
- Fang Y et al. Prevalence of occult hepatitis B infection among hepatopathology patients and healthy people in China. Journal of Infection, 2009, 58:383–388.
- Allain J. Occult hepatitis B virus infection: implications in transfusion. Vox Sanguinis, 2008, 86:83–91.
- Torbenson M, Thomas M. Occult hepatitis B. Lancet Infectious Diseases, 2002, 2:479–486.
- El-Sherif A et al. Antibody to hepatitis B core antigen as a screening test for occult hepatitis B virus infection in Egyptian chronic HCV patients. Journal of Gastroenterology, 2009, 44:359–364.
- Said ZN. An overview of occult hepatitis B virus infection. World Journal of Gastroenterology, 2011, 17(15):1927–1938.
- Ozaslan E, Purnak T. Controversies about occult hepatitis B virus infection. World Journal of Gastroenterology, 2009, 15:4986–4987.
- Thompson JD, Julie D, Desmond G. CLUSTAL W: improving the sensitivity of progressive multiple sequence alignment through sequence weighting, position-specific gap penalties and weight matrix choice. Nucleic Acids Research, 1994, 22:4673–4680.
- Shin-IT et al. Development and public release of a comprehensive hepatitis virus database. Hepatology Research, 2008, 38:234–243.
- Emara M et al. Occult hepatitis B virus infection in Egyptian chronic HCV patients: prevalence, impact on PEG-IFN/RBV therapy. Virology Journal, 2010, 17(7):324.
- Niederau C, Fischer C, Kautz A. [Socio-economical aspects, quality of life and state of knowledge in hepatitis B patients. Socio-economical aspects in hepatitis B.] Soziookonomische Charakteristika, Lebensqualitat und Wissensstand bei Patienten mit Hepatitis-B-Virusinfektion in Deutschland. Soziookonomische Aspekte bei Hepatitis B. Zeitschrift fur Gastroenterologie, 2007, 45(5):355–368.
- Malone D, Tran T, Poordad F. Cost-efficacy analysis of PEG-IFNα- 2b/RBV compared with PEG-IFNα-2a/RBV for the treatment of chronic hepatitis C. Journal of Managed Care Pharmacy, 2005, 11:687–694.
- Khattab E et al. Analysis of HCV co-infection with occult hepatitis B virus in patients undergoing IFN therapy. Journal of Clinical Virology, 2005, 33:150–157.
- Fukuda R et al. Co-infection by serologically silent hepatitis B virus may contribute to poor interferon response in patients with chronic HCV by down-regulation of type-I interferon receptor gene expression in the liver. Journal of Medical Virology, 2001, 63:220–227.
- Fujiwara K et al. Lack of association between occult hepatitis B virus DNA viral load and aminotransferase levels in patients with hepatitis C virus related chronic liver disease. Journal of Gastroenterology and Hepatology, 2004, 19:1343–1347.
- Fabris P et al. Occult hepatitis B virus infection does not affect liver histology or response to therapy with interferon alpha and ribavirin in intravenous drug users with chronic hepatitis C. Journal of Clinical Virology, 2004, 9:160–166.
- De Maria N et al. The impact of previous HBV infection on the course of chronic HCV. American Journal of Gastroenterology, 2000, 95:3529–3536.
- Levast M et al. Prevalence and Impact of occult hepatitis B virus infection in chronic HCV patients treated with pegylated interferon and ribavirin. Journal of Medical Virology, 2010, 82:747–754.
- Marcellin P. Hepatitis B and hepatitis C in 2009. Liver International, 2009, 29(s1):1–8
- Cooreman M et al. Characterization of the reactivity pattern of murine monoclonal antibodies against wild-type hepatitis B surface antigen to G145R and other naturally occurring “a” loop escape mutations. Hepatology, 2009, 30:1287–1292.








