School-aged children receive essential medicines to tackle schistosomiasis and soil-transmitted helminth infections. WHOSomalia/Khurram Sajjad.29 May 2022 – Neglected tropical diseases affect people who lack regular access to adequate sanitation, basic health infrastructure and health services. These diseases can lead to significant morbidity, mortality, stigma and discrimination in communities.
School-aged children receive essential medicines to tackle schistosomiasis and soil-transmitted helminth infections. WHOSomalia/Khurram Sajjad.29 May 2022 – Neglected tropical diseases affect people who lack regular access to adequate sanitation, basic health infrastructure and health services. These diseases can lead to significant morbidity, mortality, stigma and discrimination in communities.
Prevalence of neglected tropical diseases
Of the 20 neglected tropical diseases listed by WHO as endemic in tropical countries, schistosomiasis and soil-transmitted helminth infections, along with leprosy and visceral leishmaniasis, are common in Somalia. About 5 to 6 million people in the country live in the areas that are highly endemic for these diseases.
Between 2016 and 2017, WHO and the Ministry of Health and Human Services of Somalia conducted a mapping exercise to determine where neglected tropical diseases affect people. They found unexpected cases of intestinal schistosomiasis due to Schistosoma mansoni, or snails, in the South West state and in Banadir. Hookworms are known to be common in these locations too.
Communities living in South West Somalia, across the middle and lower valleys of the Shabelle and Juba rivers, reportedly suffer the most from these diseases. Additionally, internally displaced persons are also among the most affected, due to their living conditions.
Reducing spread of infections
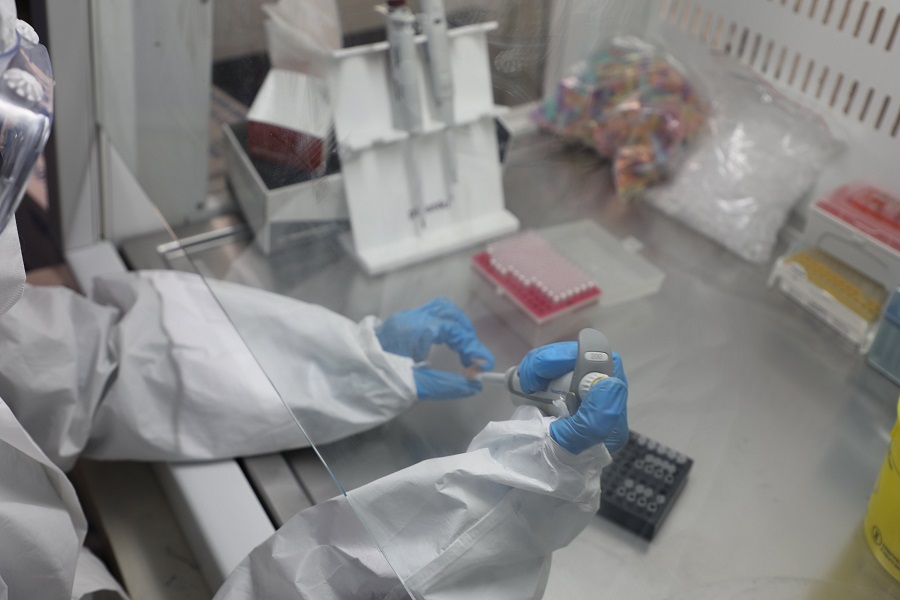
To reduce prevalence of these diseases, the World Health Organization (WHO) has been providing support to the Federal Government of Somalia to conduct mass drug administration campaigns since 2017.
On 7 May 2022, the country embarked on an 18-day effort to provide essential medicines, namely praziquantel and metronidazole, to around 2.48 million school-aged children (aged between 5 and 14 years) and adults in 39 districts. Health care workers have been visiting schools and madrasas to reach children and using community-based initiatives to target adults. These efforts will reduce the reservoir of infection and interrupt disease spread.
The last campaign, conducted in 2020, administered these essential medicines to around 2.6 million school-aged children and over 300 000 adults in 41 districts. It covered around 91% of a targeted 3.18 million people.
 WHO is supporting the Government to conduct the fourth mass drug administration campaign in Somalia since 2017. WHOSomalia/Khurram Sajjad.In addition to offering medicines to control and eradicate schistosomiasis and soil-transmitted helminth infections, WHO has supported the federal and state governments to increase public awareness about them. They have reached out to the most vulnerable groups, including internally displaced persons. These interventions have been possible with support from the END Fund and Expanded Special Project for Elimination of Neglected Tropical Diseases (ESPEN).
WHO is supporting the Government to conduct the fourth mass drug administration campaign in Somalia since 2017. WHOSomalia/Khurram Sajjad.In addition to offering medicines to control and eradicate schistosomiasis and soil-transmitted helminth infections, WHO has supported the federal and state governments to increase public awareness about them. They have reached out to the most vulnerable groups, including internally displaced persons. These interventions have been possible with support from the END Fund and Expanded Special Project for Elimination of Neglected Tropical Diseases (ESPEN).
“These interventions of WHO are in line with the new WHO road map for neglected tropical diseases "Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030," which sets global targets and milestones to prevent, control, eliminate or eradicate 20 neglected tropical diseases and disease groups, now prioritized by WHO, and attain the SDGs,” said Dr Mamunur Rahman Malik, WHO Representative for Somalia.
“We also believe that whatever we do and whatever strategy we undertake to eliminate the risk of neglected tropical diseases from Somalia, our efforts should contribute to building a strong foundation for the primary health care system in such a fragile health system setting. Creating demand for eliminating this disease from school-aged children and making sure that the health system delivers such public good in real-time are all part of our work in this country, aiming to build resilience,” commented Dr Mamunur Rahman Malik, on the eve of the launch of the mass drug administration campaign for schistosomiasis and soil-transmitted helminthiasis.
In line with the national action plan for Somalia, WHO and its partners, such as the ESPEN and END Fund, intend to support national health authorities to conduct mass drug administration campaigns with increased national coverage for schistosomiasis, including more than 75% of treatment coverage for school-aged children, to eliminate the disease as a public health problem by 2025. The campaigns will also treat soil-transmitted helminthiasis, including deworming coverage for at least 75% of eligible school-aged children and pre-school children by 2026.
Both schistosomiasis and soil-transmitted helminth infections are spread due to a lack of hygiene, when people do not have access to water and sanitation facilities, or do not wash their hands often, particularly before meals or after excretion.
For additional information, please visit:
ESPEN: ESPEN | Expanded Special Project for Elimination Neglected Tropical Diseases (who.int)
The END Fund: Home - The END Fund