1. Background and situation analysis
Zika virus disease is caused by a RNA flavivirus transmitted to humans by the Aedes mosquito, the same type of mosquito that transmits dengue, chikungunya and yellow fever. Only 20% of people with Zika virus infection show symptoms, which include mild fever, skin rash and conjunctivitis. These symptoms normally last for 2–7 days. Currently, there is no vaccine to prevent the disease or any specific anti-viral treatment available.
In December 2013, authorities in French Polynesia reported an increased incidence of rare neurological disorders. Among these reports, 42 cases were diagnosed as Guillain-Barré syndrome. A preceding viral infection was reported in 88% of these cases and retrospective analysis demonstrated that all 42 cases had serological tests suggesting prior dengue and Zika virus infections. In July 2015, authorities in the State of Bahía, Brazil, reported an increase in the number of patients with neurological syndromes, of whom 42 were confirmed as Guillain-Barré cases. Of these 42 confirmed cases, 26 had reported symptoms consistent with Zika virus infection.
In October 2015, Brazilian health authorities reported an unusual increase in the number of cases of microcephaly in Pernambuco State, northeast Brazil. In the following 3 months, over 4000 suspected cases of microcephaly were reported. Likewise, in November 2015, the French Polynesian authorities reported an unusual increase in the number of central nervous system malformations in fetuses and neonates from March 2014 to May 2015. 18 cases with different severe neurological malformations were reported which significantly exceeded the background incidence.
In both Brazil and French Polynesia, this reported increase in the number of neurological disorders and congenital malformations occurred within the context of arbovirus circulation, and both countries were experiencing a Zika outbreak for the first time. Prior to 2007, Zika virus infection had not been documented outside Asia or Africa. As of April 2016, over 60 countries in the Americas, the Pacific Islands, South-east Asia and Africa have reported local transmission of Zika virus disease.
The current Zika virus outbreaks, and associated microcephaly and neurological disorders, have caused increasing alarm in countries across the world. Brazil announced a national public health emergency in November 2015. Some countries in Latin America have advised women to postpone pregnancies until this potentially severe health risk is better understood. The Centers for Disease Control and Prevention, Atlanta, and the European Centre for Disease Control and Prevention,Stockholm, and other national public health agencies have also issued travel warnings, which include recommendations that pregnant women consider postponing travel to any area with ongoing Zika virus transmission. On 1 February 2016, WHO announced that the recent cluster of neurological disorders and neonatal malformations reported in the Americas region constitute a Public Health Emergency of International Concern (PHEIC) and called for a global response to the spread of Zika virus disease.
1.1 Situation in the Eastern Mediterranean Region and risk analysis
As of May 2016, no countries of the Region have reported importation of Zika virus disease or autochthonous transmission. However, there is currently no specific surveillance for Zika or available laboratory testing. Of the 22 countries in the Region, the following 8 have reported dengue outbreaks in recent years and/or have the presence of competent Aedes mosquitoes: Djibouti, Egypt, Oman, Pakistan, Saudi Arabia, Somalia, Sudan and Yemen.
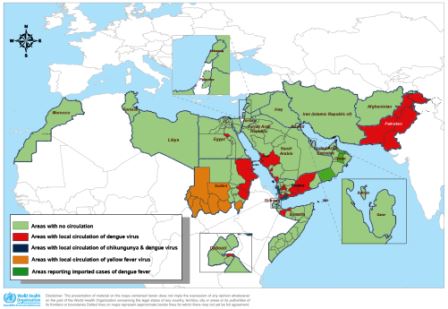
Fig. 1. Areas with circulation of dengue, chikungunya and yellow fever virus, 1959–2015
Zika virus infection further compounds the challenges as the majority of infected people do not display any symptoms and the population has no immunity to this new virus.
2. Current gaps in preparedness and response capacities for Zika
Based on the findings of the WHO Region-wide assessment of Ebola preparedness in 2015 and recent country experiences in responding to major outbreaks of emerging infectious diseases, including Middle East respiratory syndrome coronavirus (MERS-CoV), influenza and viral haemorrhagic fever, the following gaps, which may affect preparedness and response capacities for Zika, have been identified:
- Gaps in public health leadership capacities, as well as in planning and coordination of preparedness for public health emergencies
- Inadequate capacity at the points of entry (PoE) for surveillance and response to public health threats
- Inadequate disease surveillance systems and response capacities in general
- Weak vector surveillance and vector control programmes
- Limited capacity and skills to perform risk communication and to promote community engagement
- Insufficient regional epidemiological knowledge on Zika infections, and large knowledge gaps in vector entomology
- Weak diagnostic capacity for detection of emerging pathogens
3. Preparedness plan for Zika
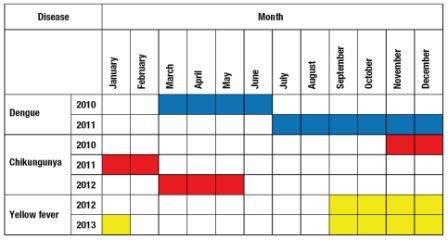
In the event that Zika virus were to occur in the Region as a result of local transmission or importation, the preparedness plan must address the need for significant improvements in preparedness and response capacities before the possible transmission season, which for arboviral diseases occurs from October to December in most countries.
Table 1. Seasonality of arboviral diseases in the Eastern Mediterranean Region
3.1 Goal
The overall goal of this preparedness plan is to support countries to enhance surveillance and response for Zika virus infection in order to promptly detect any imported cases; rapidly contain local transmission; and mitigate adverse health impacts in the countries in the Region.
3.2 Objectives and priority activities
The following priority actions have been identified for countries, noting that as of May 2016 the Region has not yet reported any case of Zika virus infection.
Improve leadership and coordination for enhanced preparedness and response capacities
- Strengthen regional public health leadership, incident management systems, multisectoral coordination and information sharing mechanisms for Zika virus infection in the Region.
- Support countries to use an all-hazard approach to develop and implement contingency plans for epidemic and pandemic preparedness and response plans, and to adapt these for possible Zika infections.
Enhance capacities required under the IHR (2005) at international Points of Entry (PoE)
- Build regional capacity for surveillance, early detection and response to public health events at international points of entry.
- Strengthen effective coordination and collaboration among stakeholders of points of entry, and improve their awareness of the risks of importation/exportation of Zika vectors.
Support regional risk assessments and the development of effective surveillance systems
- Establish national Zika infection risk profiles.
- Establish effective surveillance systems for Zika virus infection and associated congenital birth defects and neurological complications.
- Develop regional capacity on risk assessment, surveillance and epidemiological investigation around suspected or confirmed Zika cases.
Reinforce entomological surveillance and vector control
- Provide guidance and support on entomological surveillance and integrated vector management to reduce the risk of exposure to Zika.
- Establish geographic distribution of competent vectors regionally and at country level.
- Strengthen specific medical entomology research, knowledge and skills at country level through training activities.
Improve access to quality diagnostics testing and rapid turnaround of results
- Establish Zika virus diagnostic services in the Region.
- Coordinate and build capacity for collection, storage and transportation of samples; and establish a process for shipment of specimens to reference laboratories.
- Build capacity to perform routine diagnostic testing.
Improve risk communication and community engagement
- Establish Zika virus risk communication protocols for countries and key communications products for various target groups.
- Establish engagement with communities on Zika virus infection and vector control activities.
- Support Zika awareness-raising activities for mass gatherings.
Address regional knowledge gaps through operational research
- Promote entomological research on competent Aedes.
- Refine epidemiological knowledge of possible early Zika circulation in the Region.
- Support operational research on Zika and related arboviral infections, and their vectors, in order to narrow the knowledge gap.
Preparedness plan for Zika in the Eastern Mediterranean Region [flyer]
3.3 Operationalization of the plan
An incident management system has been established in the Regional Office to support overall planning and implementation of the plan. The WHO Department of Communicable Disease Prevention and Control and the pandemic and epidemic disease programme will coordinate the operationalization of the plan in close consultation and collaboration with other technical programmes. Each collaborating technical programme has a designated staff member responsible for a function in the incident management system.
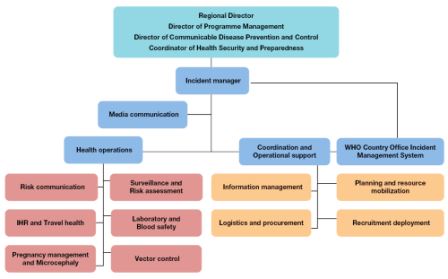
Fig. 2. Structure of regional incident management system for Zika virus
The plan will require ensuring close and transparent communication, conducting of technical missions, organizing meetings, workshops and training, and ensuring close interaction and follow-up with countries of the Region, WHO headquarters, other United Nations agencies and international health partners of WHO.
4. Monitoring and evaluation
The implementation of a Zika preparedness plan will be monitored and evaluated regularly by the WHO Regional Office through a combination of process/output metrics and operational response performance indicators corresponding to each of the major objectives.
Country activities in implementation of Zika preparedness plan
 Preparedness plan for Zika in the Eastern Mediterranean Region [flyer]
Preparedness plan for Zika in the Eastern Mediterranean Region [flyer]




