Influenza pandemic occurs when a new influenza virus emerges and spreads around the world, and most people do not have immunity. Viruses that have caused past pandemics typically originated from animal influenza viruses.
Some aspects of influenza pandemics can appear similar to seasonal influenza while other characteristics may be quite different. For example, both seasonal and pandemic influenza can cause infections in all age groups, and most cases will result in self-limited illness in which the person recovers fully without treatment. However, typical seasonal influenza causes most of its deaths among the elderly while other severe cases occur most commonly in people with a variety of medical conditions.
For both seasonal and pandemic influenza, the total number of people who get severely ill can vary. However, the impact or severity tends to be higher in pandemics in part because of the much larger number of people in the population who lack pre-existing immunity to the new virus. When a large portion of the population is infected, even if the proportion of those infected that go on to develop severe disease is small, the total number of severe cases can be quite large.
COVID-19 and influenza
Many of the influenza symptoms are similar to those that are present for COVID-19. For example, symptoms such as fever, headache, muscle ache, sneezing and coughing. For COVID-19, additionally, there are specific symptoms such as anosmia, which is a lack of smell or taste of food. Many people, especially young people, have experienced these additional and specific symptoms for COVID-19.
 The presence of these symptoms, whether they are for influenza or for COVID-19, varies in people depending on their level of immunity. It is important to note that the prevention measures, such as washing hands, wearing masks, and maintaining physical distancing are very effective for both diseases. Both seasonal influenza and COVID-19 are preventable through following these measures.
The presence of these symptoms, whether they are for influenza or for COVID-19, varies in people depending on their level of immunity. It is important to note that the prevention measures, such as washing hands, wearing masks, and maintaining physical distancing are very effective for both diseases. Both seasonal influenza and COVID-19 are preventable through following these measures.
Vaccination is effective for preventing seasonal influenza, in particular, preventing severe disease outcomes in older adults, people with serious health conditions and pregnant women. Infants may be protected by passively acquired immunity from their mother for the first 6–9 months of age. COVID-19 vaccines provide strong protection against serious illness, hospitalization and death from COVID-19. There is also some evidence that being vaccinated will make it less likely that you will pass the virus on to others, which means your decision to get the vaccine also protects those around you.
The viruses
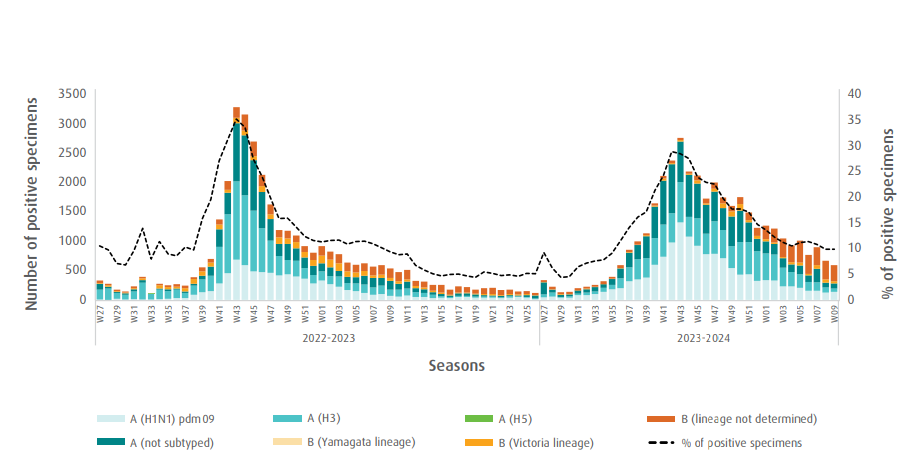
Influenza virus is a respiratory virus that is part of the Orthomyxoviridae family. There are 4 types of seasonal influenza viruses, types A, B, C and D. Influenza A and B viruses circulate and cause seasonal epidemics of disease. They can be further broken down into subtypes depending on the combination of the proteins on their surface (e.g. influenza A) or different lineages (e.g. influenza B). Infection with influenza viruses causes influenza disease.
COVID-19 is an infectious disease caused by a respiratory virus called the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-CoV-2 is part of the coronavirus family and can be further classified into variants and subvariants.
Signs and symptoms
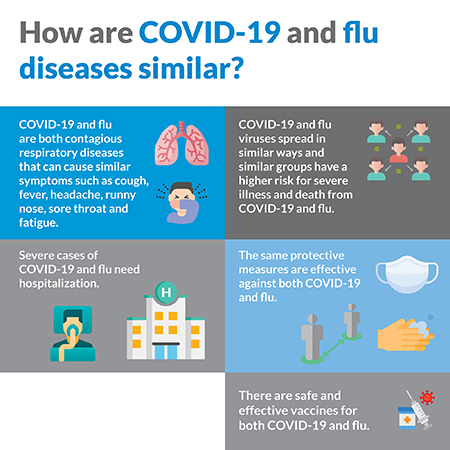 Both COVID-19 and influenza disease share similar symptoms, including cough, runny nose, sore throat, fever, headache and fatigue. People infected with either virus can have varying levels of illness; some having no symptoms, mild symptoms or severe disease. People with mild symptoms of both COVID-19 and influenza can usually be cared for safely at home. Both diseases can be fatal, with certain people at higher risk for severe disease and death.
Both COVID-19 and influenza disease share similar symptoms, including cough, runny nose, sore throat, fever, headache and fatigue. People infected with either virus can have varying levels of illness; some having no symptoms, mild symptoms or severe disease. People with mild symptoms of both COVID-19 and influenza can usually be cared for safely at home. Both diseases can be fatal, with certain people at higher risk for severe disease and death.
You cannot tell the difference between flu and COVID-19 from symptoms. Testing for the virus is the only way you can know which virus you have or reveal if someone has both influenza and COVID-19 at the same time.
Prevention
Both COVID-19 and influenza can spread from person to person, mainly in those who are in close contact with each other. Both are spread primarily by large and small particles containing virus when people with either virus cough, sneeze or talk. It is also possible to get infected by touching another person or a surface that has virus on it and then subsequently touching their own mouth, nose or eyes. Therefore, personal protective measures like:
- Regular hand washing with proper drying of the hands
- Good respiratory hygiene – Cough or sneeze into a bent elbow or tissue and throw the tissue into a closed bin
- Early self-isolation of those feeling unwell, feverish and having other symptoms of influenza
- Avoiding close contact with sick people
- Avoiding touching your eyes, nose or mouth
Can help to protect you and others from infection. Other protective measures to protect from infection also include:

- Maintain at least a 1-metre distance from others and wear a well-fitted mask
- Avoid crowded and poorly ventilated places and settings;
- Open windows or doors to keep rooms well ventilated;
In addition to these measures there are safe and effective vaccines for both COVID-19 and influenza. Vaccination is an important part of preventing severe disease and death for both COVID-19 and influenza. The vaccines for COVID-19 and influenza are not cross-protective. Influenza vaccines are different to COVID-19 vaccines so you must get both to protect yourself from each disease.
Treatment
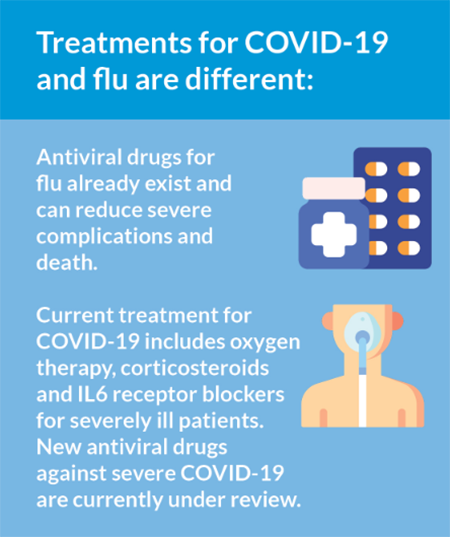 Different treatments are available for both influenza and COVID-19, but both in the initial stages are treated by addressing symptoms such as fever. Both viruses can cause severe disease, leading to hospitalization where more supportive treatment is needed such as a ventilator. For some patients, medications may help lessen the symptoms, severity and shorten the duration of COVID-19 or influenza illness.
Different treatments are available for both influenza and COVID-19, but both in the initial stages are treated by addressing symptoms such as fever. Both viruses can cause severe disease, leading to hospitalization where more supportive treatment is needed such as a ventilator. For some patients, medications may help lessen the symptoms, severity and shorten the duration of COVID-19 or influenza illness.
For influenza, there are oral antiviral medications available that can be used to supplement symptomatic treatment. Patients that are known to be in a group at high risk for developing severe or complicated illness should be treated with antivirals in addition to symptomatic treatment as soon as possible. Patients with severe or progressive clinical illness associated with suspected or confirmed influenza virus infection (i.e. clinical syndromes of pneumonia, sepsis or exacerbation of chronic underling diseases) should be treated with antiviral drug as soon as possible.
For COVID-19 those with milder illness, resting at home and taking medicine to reduce fever or other symptoms is usually enough. However more severe cases that require hospitalization may be treated with both novel treatments (e.g. monoclonal antibody therapy) and provided with supportive care. Optimal supportive care includes oxygen for severely ill patients and those who are at risk for severe disease and more advanced respiratory support such as ventilation for patients who are critically ill. Dexamethasone is a corticosteroid that can help reduce the length of time on a ventilator and save lives of patients with severe and critical illness. Results from the WHO’s Solidarity Trial indicated that remdesivir, hydroxychloroquine, lopinavir/ritonavir and interferon regimens appear to have little or no effect on 28-day mortality or the in-hospital course of COVID-19 among hospitalized patients. Hydroxychloroquine has not been shown to offer any benefit for treatment of COVID-19. WHO does not recommend self-medication with any medicines, including antibiotics, as a prevention or cure for COVID-19. WHO is coordinating efforts to develop treatments for COVID-19 and will continue to provide new information as it becomes available.
Influenza updates
All weekly updates
- 2024
- Influenza update, epidemiological week 9, 2024
- Influenza update, epidemiological week 8, 2024
- Influenza update, epidemiological week 7, 2024
- Influenza update, epidemiological week 6, 2024
- Influenza update, epidemiological week 5, 2024
- Influenza update, epidemiological week 4, 2024
- Influenza update, epidemiological week 3, 2024
- Influenza update, epidemiological week 2, 2024
- Influenza update, epidemiological week 1, 2024
- 2023
- Influenza update, epidemiological week 36, 2023
- Influenza update, epidemiological week 35, 2023
- Influenza update, epidemiological weel 34, 2023
- Influenza update, epidemiological week 33, 2023
- Influenza update, epidemiological week 31, 2023
- Influenza update, epidemiological week 30, 2023
- Influenza update, epidemiological week 29, 2023
- Influenza update, epidemiological week 28, 2023
- Influenza update, epidemiological week 27, 2023
- Influenza update, epidemiological week 13, 2023
- Influenza update, epidemiological week 12, 2023
- Influenza update, epidemiological week 11, 2023
- Influenza update, epidemiological week 10, 2023
- Influenza update, epidemiological week 9, 2023
- Influenza update, epidemiological week 8, 2023
- Influenza update, epidemiological week 7, 2023
- Influenza update, epidemiological week 6, 2023
- Influenza update, epidemiological week 5, 2023
- Influenza update, epidemiological week 4, 2023
- Influenza update, epidemiological week 3, 2023
- Influenza update, epidemiological week 2, 2023
- Influenza update, epidemiological week 1, 2023
- 2022
- Influenza update, epidemiological week 52, 2022
- Influenza update, epidemiological week 51, 2022
- Influenza update, epidemiological week 50, 2022
- Influenza update, epidemiological week 49, 2022
- Influenza update, epidemiological week 48, 2022
- Influenza update, epidemiological week 47, 2022
- Influenza update, epidemiological week 46, 2022
- Influenza update, epidemiological week 45, 2022
- Influenza update, epidemiological week 44, 2022
- Influenza update, epidemiological week 43, 2022
- Influenza update, epidemiological week 42, 2022
- Influenza update, epidemiological week 41, 2022
- Influenza update, epidemiological week 40, 2022
- Influenza update, epidemiological week 39, 2022
- Influenza update, epidemiological week 38, 2022
- Influenza update, epidemiological week 37, 2022
- Influenza update, epidemiological week 36, 2022
- Influenza update, epidemiological week 35, 2022
- Influenza update, epidemiological week 34, 2022
- Influenza update, epidemiological week 33, 2022
- Influenza update, epidemiological week 32, 2022
- Influenza update, epidemiological week 31, 2022
- Influenza update, epidemiological week 30, 2022
- Influenza update, epidemiological week 29, 2022
- Influenza update, epidemiological week 28, 2022
- Influenza update, epidemiological week 27, 2022
- Influenza update, epidemiological week 26, 2022
- Influenza update, epidemiological week 25, 2022
- Influenza update, epidemiological week 24, 2022
- Influenza update, epidemiological week 23, 2022
- Influenza update, epidemiological week 22, 2022
- Influenza update, epidemiological week 21, 2022
- Influenza update, epidemiological week 20, 2022
- Influenza update, epidemiological week 19, 2022
- Influenza update, epidemiological week 18, 2022
- Influenza update, epidemiological week 17, 2022
- Influenza update, epidemiological week 16, 2022
- Influenza update, epidemiological week 15, 2022
- Influenza update, epidemiological week 14, 2022
- Influenza update, epidemiological week 13, 2022
- Influenza update, epidemiological week 12, 2022
- Influenza update, epidemiological week 11, 2022
- Influenza update, epidemiological week 10, 2022
- Influenza update, epidemiological week 09, 2022
- Influenza update, epidemiological week 08, 2022
- Influenza update, epidemiological week 07, 2022
- Influenza update, epidemiological week 06, 2022
- Influenza update, epidemiological week 05, 2022
- Influenza update, epidemiological week 04, 2022
- Influenza update, epidemiological week 03, 2022
- Influenza update, epidemiological week 02, 2022
- Influenza update, epidemiological week 01, 2022
- 2021
- Influenza update, epidemiological week 52, 2021
- Influenza update, epidemiological week 51, 2021
- Influenza update, epidemiological week 50, 2021
- Influenza update, epidemiological week 49, 2021
- Influenza update, epidemiological week 48, 2021
- Influenza update, epidemiological week 47, 2021
- Influenza update, epidemiological week 46, 2021
- Influenza update, epidemiological week 45, 2021
- Influenza update, epidemiological week 44, 2021
- Influenza update, epidemiological week 43, 2021
- Influenza update, epidemiological week 42, 2021
- Influenza update, epidemiological week 41, 2021
- Influenza update, epidemiological week 40, 2021
- Influenza update, epidemiological week 39, 2021
- Influenza update, epidemiological week 38, 2021
- Influenza update, epidemiological week 37, 2021
- Influenza update, epidemiological week 36, 2021
- Influenza update, epidemiological week 35, 2021
- Influenza update, epidemiological week 34, 2021
- Influenza update, epidemiological week 33, 2021
- Influenza update, epidemiological week 32, 2021
- Influenza update, epidemiological week 31, 2021
- Influenza update, epidemiological week 30, 2021
- Influenza update, epidemiological week 29, 2021
- Influenza update, epidemiological week 28, 2021
- Influenza update, epidemiological week 27, 2021
- Influenza update, epidemiological week 26, 2021
- Influenza update, epidemiological week 25, 2021
- Influenza update, epidemiological week 24, 2021
- Influenza update, epidemiological week 23, 2021
- Influenza update, epidemiological week 22, 2021
- Influenza update, epidemiological week 21, 2021
- Influenza update, epidemiological week 20, 2021
- Influenza update, epidemiological week 19, 2021
- Influenza update, epidemiological week 18, 2021
- Influenza update, epidemiological week 17, 2021
- Influenza update, epidemiological week 16, 2021
- Influenza update, epidemiological week 15, 2021
- Influenza update, epidemiological week 14, 2021
- Influenza update, epidemiological week 13, 2021
- Influenza update, epidemiological week 12, 2021
- Influenza update, epidemiological week 11, 2021
- Influenza update, epidemiological week 10, 2021
- Influenza update, epidemiological week 09, 2021
- Influenza update, epidemiological week 08, 2021
- Influenza update, epidemiological week 07, 2021
- Influenza update, epidemiological week 06, 2021
- Influenza update, epidemiological week 05, 2021
- Influenza update, epidemiological week 04, 2021
- Influenza update, epidemiological week 03, 2021
- Influenza update, epidemiological week 02, 2021
- Influenza update, epidemiological week 01, 2021
- 2020
- Influenza update, epidemiological week 11, 2020
- Influenza update, epidemiological week 10, 2020
- Influenza update, epidemiological week 09, 2020
- Influenza update, epidemiological week 08, 2020
- Influenza update, epidemiological week 07, 2020
- Influenza update, epidemiological week 06, 2020
- Influenza update, epidemiological week 05, 2020
- Influenza update, epidemiological week 04, 2020
- Influenza update, epidemiological week 03, 2020
- Influenza update, epidemiological week 02, 2020
- Influenza update, epidemiological week 01, 2020
- 2019
- Influenza update, epidemiological week 52, 2019
- Influenza update, epidemiological week 51, 2019
- Influenza update, epidemiological week 50, 2019
- Influenza update, epidemiological week 49, 2019
- Influenza update, epidemiological week 48, 2019
- Influenza update, epidemiological week 47, 2019
- Influenza update, epidemiological week 46, 2019
- Influenza update, epidemiological week 45, 2019
- Influenza update, epidemiological week 44, 2019
- Influenza update, epidemiological week 43, 2019
- Influenza update, epidemiological week 42, 2019
- Influenza update, epidemiological week 41, 2019
- Influenza update, epidemiological week 40, 2019
- Influenza update, epidemiological week 39, 2019
- Influenza update, epidemiological week 38, 2019
- Influenza update, epidemiological week 37, 2019
- Influenza update, epidemiological week 36, 2019
- Influenza update, epidemiological week 35, 2019
- Influenza update, epidemiological week 34, 2019
- Influenza update, epidemiological week 33, 2019
- Influenza update, epidemiological week 32, 2019
- Influenza update, epidemiological week 31, 2019
- Influenza update, epidemiological week 30, 2019
- Influenza update, epidemiological week 29, 2019
- Influenza update, epidemiological week 28, 2019
- Influenza update, epidemiological week 27, 2019
- Influenza update, epidemiological week 26, 2019
- Influenza update, epidemiological week 25, 2019
- Influenza update, epidemiological week 24, 2019
- Influenza update, epidemiological week 23, 2019
- Influenza update, epidemiological week 22, 2019
- Influenza update, epidemiological week 21, 2019
- Influenza update, epidemiological week 20, 2019
- Influenza update, epidemiological week 19, 2019
- Influenza update, epidemiological week 18, 2019
- Influenza update, epidemiological week 17, 2019
- Influenza update, epidemiological week 16, 2019
- Influenza update, epidemiological week 15, 2019
- Influenza update, epidemiological week 14, 2019
- Influenza update, epidemiological week 13, 2019
- Influenza update, epidemiological week 12, 2019
- Influenza update, epidemiological week 11, 2019
- Influenza update, epidemiological week 10, 2019
- Influenza update, epidemiological week 09, 2019
- Influenza update, epidemiological week 08, 2019
- Influenza update, epidemiological week 07, 2019
- Influenza update, epidemiological week 06, 2019
- Influenza update, epidemiological week 05, 2019
- Influenza update, epidemiological week 04, 2019
- Influenza update, epidemiological week 03, 2019
- Influenza update, epidemiological week 02, 2019
- Influenza update, epidemiological week 01, 2019
- 2018
- Influenza update, epidemiological week 52, 2018
- Influenza update, epidemiological week 51, 2018
- Influenza update, epidemiological week 50, 2018
- Influenza update, epidemiological week 49, 2018
- Influenza update, epidemiological week 48, 2018
- Influenza update, epidemiological week 47, 2018
- Influenza update, epidemiological week 46, 2018
- Influenza update, epidemiological week 45, 2018
- Influenza update, epidemiological week 44, 2018
- Influenza update, epidemiological week 43, 2018
- Influenza update, epidemiological week 42, 2018
- Influenza update, epidemiological week 41, 2018
- Influenza update, epidemiological week 40, 2018
- Influenza update, epidemiological week 39, 2018
- Influenza update, epidemiological week 38, 2018
- Influenza update, epidemiological week 37, 2018
- Influenza update, epidemiological week 36, 2018
- Influenza update, epidemiological week 35, 2018
- Influenza update, epidemiological week 34, 2018
- Influenza update, epidemiological week 33, 2018
- Influenza update, epidemiological week 32, 2018
- Influenza update, epidemiological week 31, 2018
- Influenza update, epidemiological week 30, 2018
- Influenza update, epidemiological week 29, 2018
- Influenza update, epidemiological week 28, 2018
- Influenza update, epidemiological week 27, 2018
- Influenza update, epidemiological week 26, 2018
- Influenza update, epidemiological week 25, 2018
- Influenza update, epidemiological week 24, 2018
- Influenza update, epidemiological week 23, 2018
- Influenza update, epidemiological week 22, 2018
- Influenza update, epidemiological week 21, 2018
- Influenza update, epidemiological week 20, 2018
- Influenza update, epidemiological week 19, 2018
- Influenza update, epidemiological week 18, 2018
- Influenza update, epidemiological week 17, 2018
- Influenza update, epidemiological week 16, 2018
- Influenza update, epidemiological week 15, 2018
- Influenza update, epidemiological week 14, 2018
- Influenza update, epidemiological week 13, 2018
- Influenza update, epidemiological week 12, 2018
- Influenza update, epidemiological week 11, 2018
- Influenza update, epidemiological week 10, 2018
- Influenza update, epidemiological week 09, 2018
- Influenza update, epidemiological week 08, 2018
- Influenza update, epidemiological week 07, 2018
- Influenza update, epidemiological week 06, 2018
- Influenza update, epidemiological week 05, 2018
- Influenza update, epidemiological week 04, 2018
Influenza monthly update, February 2024
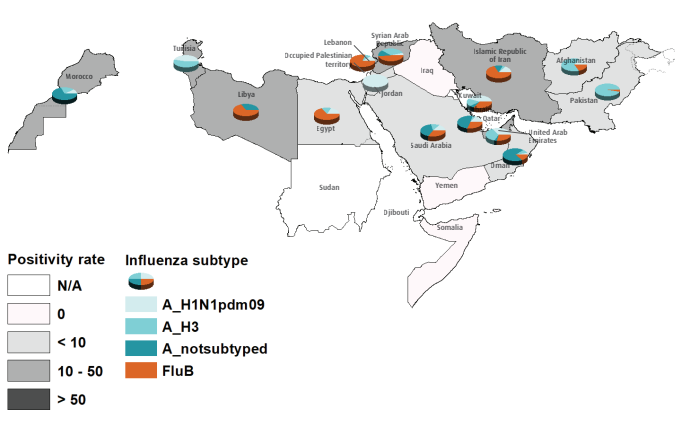
In February 2024, 19 out of 21 Member States with existing influenza surveillance systems in the WHO Eastern Mediterranean Region (EMR) reported influenza data to FluNet and/or EMFLU (Afghanistan, Bahrain, Egypt, the Islamic Republic of Iran, Iraq, Jordan, Lebanon, Libya, Morocco, the occupied Palestinian territory, Oman, Pakistan, Qatar, Saudi Arabia, Somalia, the Syrian Arab Republic, Tunisia, the United Arab Emirates, and Yemen)
All monthly updates
- 2024
- Influenza monthly update, Febreuary 2024
- Influenza monthly update, January 2024
- 2023
- Influenza monthly update, November 2023
- Influenza monthly update, October 2023
- Influenza monthly update, September 2023
- Influenza monthly update, August 2023
- Influenza monthly update, July 2023
- Influenza monthly update, June 2023
- Influenza monthly update, May 2023
- Influenza monthly update, April 2023
- Influenza monthly update, March 2023
- Influenza monthly update, February 2023
- Influenza monthly update, January 2023
- 2022
- Influenza monthly update, December 2022
- Influenza monthly update, November 2022
- Influenza monthly update, October 2022
- Influenza monthly update, September 2022
- Influenza monthly update, August 2022
- Influenza monthly update, July 2022
- Influenza monthly update, June 2022
- Influenza monthly update, May 2022
- Influenza monthly update, April 2022
- Influenza monthly update, March 2022
- Influenza monthly update, February 2022
- Influenza monthly update, January 2022
- 2021
- Influenza monthly update, December 2021
- Influenza monthly update, November 2021
- Influenza monthly update, October 2021
- Influenza monthly update, September 2021
- Influenza monthly update, August 2021
- Influenza monthly update, July 2021
- Influenza monthly update, June 2021
- Influenza monthly update, May 2021
- Influenza monthly update, April 2021
- Influenza monthly update, March 2021
- Influenza monthly update, February 2021
- Influenza monthly update, January 2021