I. Amirlak,1 M. Ezimokhai,2 A. Dawodu,3 K.P. Dawson,1 J. Kochiyil,1 L. Thomas2 and A.M. Abdulle 4
الوضع الحالي للمغذيات الزهيدة المقدار لدى الأمهات وأطفالهن الرضّع، وتأثيره على الوزن عند الولادة في الإمارات العربية المتحدة
إرادج أميرلاك، مطيرو أزيموخاي، أدكونلي داوودو، كنث داوسن، جوز كوشييل، ليث توماس، عبد الشكور عبدول
الخلاصـة: يوجد عوز المغذيات الزهيدة المقدار لدى النسوة في سن الإنجاب في الإمارات العربية المتحدة، إلا أن تأثير عوز المغذيات الزهيدة المقدار على نمو الأجنة لم يحظ بالتوثيق الجيد. ولاستقصاء الترابط بين المغذيات الزهيدة المقدار ووزن الوليد عند الولادة، أجرى الباحثون قياساً وتسجيلاً للمغذيات الزهيدة المقدار في الدم لدى الأم وفي الحبل السري للوليد (فيتامين A وC وD وE، والفريتين) لدى 84 وليداً، ممن وُلِد بمفرده، في تمام الحمل، من أم تتمتع بالصحة، عربية ومن جنوب شرق آسيا، في مستشفى العين. وقد كان وسطي تركيز حمض الأسكوربيك (فيتامين C) و25 هيدروكسي فيتامين D في المصل منخفضاً لدى الأمهات ولدى أطفالهن الرضَّع. ولدى التحليل المتعدد التفاوت، كان هناك ارتباط إيجابي بين تركيز 25 هيدروكسي فيتامين D والوزن عند الولادة، فيما لوحظ ترابط سلبي بين الفريتين في مصل الأمهات وبين وزن الوليد عند الولادة.
ABSTRACT Micronutrient deficiencies exist among women of childbearing age in the United Arab Emirates but the effects of maternal micronutrient deficiency on fetal growth are not well documented. To investigate the association between micronutrients and birth weight, we measured maternal and cord blood micronutrients (vitamin A, C, D, and E) and ferritin in 84 term, singleton infants born to healthy Arab and South Asian women at Al-Ain hospital. Median serum ascorbic acid and 25-hydroxyvitamin D (25-OHD) concentrations were low in mothers and infants. In multivariate analysis, maternal serum 25-OHD correlated positively with birth weight while serum ferritin showed a negative correlation.
Situation actuelle en matière de micronutriments chez le couple mère-enfant et effets sur le poids à la naissance aux Émirats arabes unis
RÉSUMÉ Les carences en micronutriments existent chez les femmes en âge de procréer aux Émirats arabes unis, mais les effets de la carence maternelle en micronutriments sur la croissance fœtale n’ont pas fait l’objet de nombreuses recherches. Afin d’étudier l’association entre les micronutriments et le poids à la naissance, nous avons mesuré les micronutriments (vitamine A, C, D et E) et la ferritine dans le sang maternel et du cordon chez 84 enfants uniques nés à terme de femmes arabes et originaires d’Asie du Sud en bonne santé à l’hôpital d’Al-Ain. Les concentrations sériques médianes d’acide ascorbique et de 25-hydroxyvitamine D (25-OHD) étaient faibles chez les mères et leurs nourrissons. Dans une analyse multivariée, le taux de 25-OHD sérique de la mère était positivement corrélé au poids à la naissance alors que dans le cas de la ferritine sérique, cette corrélation était négative.
1Department of Paediatrics; 2Department of Obstetrics and Gynaecology; 4Department of Internal Medicine, Faculty of Medicine and Health Sciences, United Arab Emirates University, Al-Ain, United Arab Emirates (Correspondence to I. Amirlak:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
3Cincinnati Children’s Hospital Medical Centre and University of Cincinnati College of Medicine, Cincinnati, Ohio, United States of America.
Received: 05/03/07; accepted: 08/07/07
EMHJ, 2009, 15(6):1399-1406.
Introduction
Maternal micronutrient status affects pregnancy outcome [1,2] and maternal micronutrient deficiency has been reported to be an important cause of intrauterine growth retardation [1]. Combined folic acid and iron supplementation was associated with an increase in birth weight similar to that with multiple micronutrient supplementation (containing vitamin A, folic acid, iron, zinc, vitamin D, vitamin C, vitamin E and 9 other micronutrients), while vitamin A supplementation alone had no effect on birth weight [1,3]. However, there are only a few studies on the effect of other individual maternal micronutrients on fetal growth [2–5]. Recent reports have shown positive correlations between individual maternal micronutrient levels [4,5] or micronutrient intake [6] and birth weight but the contributions of other micronutrients that could possibly affect birth weight are unknown.
In the last 2 decades, the United Arab Emirates (UAE) has witnessed rapid socioeconomic development which has focused attention on nutritional assessment in the country [7]. Previous reports from the UAE indicate that multiple micronutrient deficiencies exist in women of childbearing age [8,9]. However, there are no published studies investigating the effect of maternal
micronutrient status on fetal growth. The aim of this observational study was to determine the current micronutrient status of mother and infant pairs at birth. Furthermore, we examined the relationships between maternal and infant micronutrient status and infant birth weight.
Methods
Study setting and sample
The study hospital, Al-Ain Hospital, has about 4000 annual deliveries which represent about 60% of the births in the Al-Ain medical district [7]. Prenatal multivitamin supplements are routinely prescribed for the obstetric population, but compliance is generally poor.
The study period was 12 December 2000–12 September 2002. A convenience sample of 84 healthy Arab and South Asian women who delivered at term (37–42 weeks) following uncomplicated singleton pregnancy at Al-Ain Hospital and who agreed to participate in the study were recruited consecutively on admission for delivery.
Exclusion criteria were multiple pregnancies, complications of pregnancy such as hypertension, pre-eclampsia, anaemia and chronic cardiac and pulmonary disease. Mothers were also excluded if they had disorders such as renal, liver and gastrointestinal diseases that are likely to affect micronutrient status.
The research ethics committee of the Faculty of Medicine of the UAE University approved the study. Informed consent was obtained from each mother before entry into the study.
Data collection
Data collected included mother’s age and parity, infant’s birth weight and gestation and the results of maternal and cord blood biochemical analysis. Umbilical cord blood measurements were used as surrogates of infant’s micronutrient status at birth.
At birth, a venous blood sample was drawn from each mother and from the umbilical vein. The blood samples were protected from light and centrifuged. The serum samples were kept frozen at –80 ºC until analysed.
The serum concentrations of retinol (vitamin A) [10], 25-hydroxy vitamin D (25-OHD) [11] and α-tocopherol (vitamin E) [12] were determined using high-performance liquid chromatography (HPLC).
The details of these methods have been described in previous publications [8,13]. For the determination of serum ascorbic acid (vitamin C) levels, the deproteinized plasma was treated with acetate buffer and ascorbate oxidase and further derivatized by orthophenyl diamine before estimation using HPLC [14]. Serum ferritin concentration was measured by immunoradiometric assay kit (Diagnostic Product Corporation, Los Angeles, California). Normal ranges for each parameter used in this study are shown on Table 1.
Analysis
The results are presented as mean and standard deviation (SD) or median and interquartile range. Statistical analyses were carried out using nonparametric tests as most of the data were not normally distributed. The correlations between micronutrient status and birth weight were examined using correlation coefficients. P-value < 0.05 was considered significant.
Results
The median age of the women was 27 years (interquartile range 23; 31) and the median parity was 2 (interquartile range 1; 4). The mean gestation period was 39.6 (SD 0.99) weeks and the mean birth weight of infants was 3317 (SD 510) g. Of the 84 women in the sample, 68 (81%) were of Arab origin and the others were of South-East Asian ethnic origin (Indian and Pakistani). Although the exact number of mothers who delivered at term during the study period was not recorded, the mothers who participated in the study were of similar ethnic and cultural background to the general obstetric population, around 70% of whom are Arabs [unpublished observation].
The maternal serum retinol, 25-OHD and α-tocopherol values were significantly higher than those of the cord blood, while the cord blood ascorbic acid and ferritin levels were higher than the maternal values (Table 1).
The only significant positive correlations were between maternal serum 25-OHD and cord blood 25-OHD concentrations (r = 0.61, P = 0.001) and between maternal ascorbic and cord blood ascorbic acid concentrations (r = 0.56, P = 0.001).
The median serum ascorbic acid and 25-OHD concentrations were very low while the serum retinol and α-tocopherol concentrations were normal. The median maternal serum ferritin concentration was in the lower normal range. A total of 77% of the mothers and 31% of the infants had serum ascorbic acid concentrations below the lower cut-off value, while 71% of the mothers and 93% of the infants had serum 25-OHD concentrations below the lower cut-off point.
There were positive correlations between mother’s vitamin D levels and infant’s birth weight (r = 0.23, P < 0.05) and between umbilical cord retinol concentrations and infant’s birth weight (r = 0.21, P < 0.05). Maternal serum ferritin correlated negatively with birth weight (r = –0.24,P < 0.05). There were no significant correlations between any of the other micronutrients studied and maternal age and parity.
In order to identify the potential impact of any of the other measured variables on birth weight, we included in a multivariate analysis the variables that were related to birth weight with P-value ≤ 0.1 (cord blood vitamin A, maternal vitamin D and ferritin concentrations). In this model, maternal vitamin D status showed an independent positive effect while maternal ferritin showed a negative effect on birth weight (Table 2). A 1-unit increase in maternal serum 25-OHD concentration was associated with a 12 g increase in birth weight and 1-unit increase in maternal serum ferritin was associated with a 7 g reduction in birth weight. The correlation between maternal vitamin D status and birth weight is shown in Figure 1.
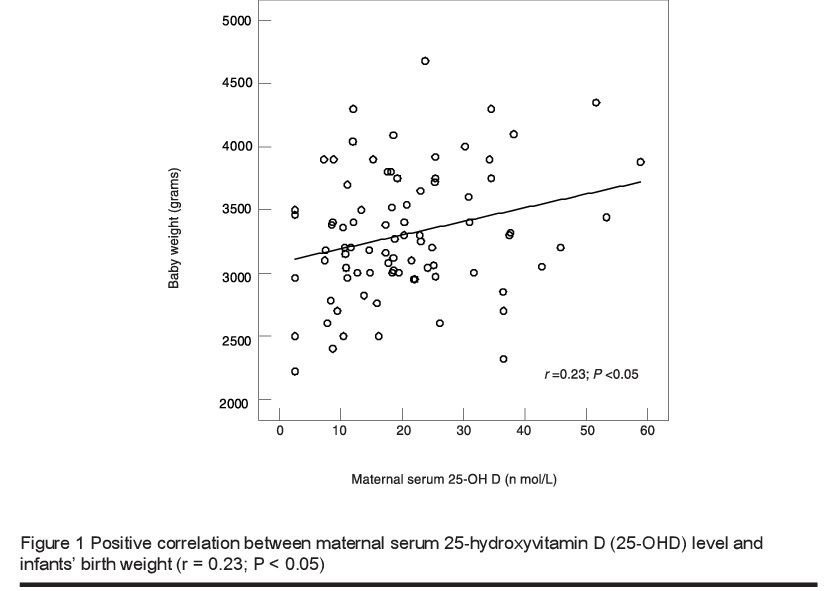
The mean birth weight of infants born to mothers with vitamin D status in the top quartiles (75th or above) was higher than those of infants born to mothers with vitamin D status in the lower quartiles (25th or less) [3441 (SD 465) g versus 3057 (SD 564) g] (P = 0.019).
Discussion
The results of this pilot study indicate that maternal deficiencies of vitamins C and D still exist in this community. Smaller sample size studies from the Middle East have also found multiple micronutrient deficiencies which included vitamins C and D and ferritin in women of childbearing age [8,9]. The high prevalence of maternal vitamin D and C deficiencies in this hospital-based study is similar to the figures previously reported in mothers and children about a decade ago from this community [8] and suggests no significant change in the prevalence of maternal micronutrient deficiencies. The correspondingly high prevalence of low serum ascorbic acid and 25-OHD concentrations in infants at birth is a reflection that the fetus depends on the mother for these micronutrients. The major risk factors in this community for deficiencies of these vitamins include inadequate dietary intake and in the case of vitamin D, lack of sunshine exposure which limits endogenous synthesis of vitamin D [8,9,13]. Despite the improvements in socioeconomic status in the UAE, these risk factors are still to be addressed [A. Dawodu, unpublished observation]. Educational activities to encourage moderate sun exposure and improve dietary intake of vitamins D and C should be intensified to improve the stores of these micronutrients in women.
In this population with a high prevalence of vitamin D deficiency, we demonstrated a positive correlation between maternal vitamin D status and birth weight of term infants. In a randomized controlled study reported about 2 decades ago, prenatal vitamin D supplementation increased maternal weight gain and reduced the risk of intrauterine growth retardation [15]. A study from India also demonstrated the beneficial effect of vitamin D supplementation on infant birth weight [16]. In our study, each 1 nmol/L increase in serum 25-OHD, which theoretically would require a daily intake of 1.4 μg vitamin D3 [17], was associated with 12 g increase in birth weight. A recent study from Canada among a population with high risk of vitamin D deficiency showed a positive correlation between vitamin D intake during pregnancy and birth weight, with an 11 g increase for each additional 1 μg/day vitamin D intake [6].
We speculate that vitamin D sufficiency during pregnancy, based on the currently recommended normal adult serum 25-OHD concentrations [18], may significantly improve fetal growth, especially in populations with a high prevalence of vitamin D deficiency. Randomized controlled trials are urgently needed to test such a hypothesis.
The impact of maternal vitamin A supplementation on fetal growth is controversial [1]. Studies in rural Nepal indicate that maternal micronutrient supplementation of vitamin A alone had no effect on birth weight, while multiple micronutrient supplements which included vitamin A increased birth weight [3,19]. In our study, there was a positive correlation between cord blood vitamin A and birth weight on bivariate analysis but not in a multivariate analysis which included parity and maternal vitamin D status. Previous studies from the Middle East found a positive correlation between cord blood retinol levels and birth weight [5] and other studies from the United Kingdom [20] and Brazil [21] also demonstrated positive correlations between cord blood vitamin A status and birth weight, length and head and chest circumference. However, these studies did not examine the possible influence of maternal vitamin D status, which could also affect fetal growth [15,16].
We did not show a positive correlation between maternal or umbilical cord vitamin C levels and birth weight. This is contrary to other findings which showed direct correlations between maternal and umbilical vein ascorbic acid levels and birth weight in infants with gestational age 24–42 weeks [22]. The difference could be due to the fact that we only studied term infants with gestational age 37–42 weeks and therefore could have missed the possible effects at shorter gestation.
The negative association between maternal serum ferritin and birth weight found in the present study is consistent with findings in other studies which showed that high maternal serum ferritin levels were associated with asymmetrical fetal growth retardation [23]. The reason for the negative effect of high maternal serum ferritin is not clear. Some authors have suggested that the high maternal serum ferritin level might indicate exposure to infections or a noninfectious inflammatory condition with negative effects on fetal growth [23]. More research is needed on the relationship between high maternal serum ferritin and fetal growth. The prevalence of low maternal serum ferritin levels (21%) was greater than the 4.4% reported from Brazil [24]. Further, the prevalence of 13% for low serum ferritin concentration in healthy term infants in this study is more than 2-fold higher than the 5% reported in a study in the United States of America [25]. The high prevalence of low ferritin status at birth in our study could be contributory to the high prevalence of iron-deficiency anaemia in infancy reported recently from this community [26] because low serum ferritin at birth has been associated with increased risk of iron-deficiency anaemia later in infancy [25].
A limitation of this study was the lack of control for relevant confounding factors, such as dietary intake and maternal nutritional status that would affect birth weight. The results, however, indicate that multiple micronutrient deficiencies still exist in mothers and their offspring in the UAE. Research is indicated to assess the effect of adequate maternal vitamin D supplementation on fetal growth as well as the relationship between maternal ferritin during pregnancy and fetal growth.
Acknowledgement
This study was supported by a Faculty of Medicine and Health Sciences, United Arab Emirates University Research grant.
References
- Christian P. Micronutrients and reproductive health issues: an international perspective. Journal of nutrition, 2003, 133:1969S–73S.
- Costello AM, Osrin D. Micronutrient status during pregnancy and outcomes for newborn infants in developing countries. Journal of nutrition, 2003, 133:1757S–64S.
- Christian P et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. British medical journal, 2003, 326:571–6.
- Hininger I et al. Effects of a combined micronutrient supplementation on maternal biological status and newborn anthropometrics measurements: a randomized double-blind, placebo-controlled trial in apparently healthy pregnant women. European journal of clinical nutrition, 2004, 58:52–9.
- Gazala E et al. Retinol concentration in maternal and cord serum: its relation to birth weight in healthy mother–infant pairs. Early human development, 2003, 71:19–28.
- Mannion CA, Gray-Donald K, Koski KG. Association of low intake of milk and vitamin D during pregnancy with decreased birth weight. Canadian Medical Association journal, 2006, 174:1273–7.
- Annual report 1992. Abu Dhabi, United Arab Emirates Ministry of Health, 1992:132–4.
- Dawson KP et al. Current nutritional status of mothers and children in Al Ain, United Arab Emirates. Eastern Mediterranean health journal, 1996, 2:224–8.
- Dawodu A et al. Diet, clothing, sunshine exposure and micronutrient status of Arab infants and young children. Annals of tropical paediatrics, 2001, 21:39–44.
- Shearer MJ. Vitamins. In: Lim CK, ed. HPLC of small molecules—a practical approach. Oxford, IRL Press, 1986:157–218.
- Horst RL, Reinhardt TA, Hollis BW. Improved methodology for the analysis of plasma vitamin D metabolites. Kidney international. Supplement, 1990, 29:S28–35.
- Bieri JG, Tolliver TJ, Catignani GL. Simultaneous determination of alpha tocopherol and retinol in plasma or red cells by high performance liquid chromatographpy. American journal of clinical nutrition, 1979, 32:2143–9.
- Dawodu A et al. Hypovitaminosis D and vitamin D deficiency in exclusively breast-feeding infants and their mothers in summer: a justification for vitamin D supplementation of breast-feeding infants. Journal of pediatrics, 2003, 142:169–73.
- Dawson KP, Kochiyil J, Hughes P. Leucocyte ascorbic acid levels in the cord blood of UAE infants. Current paediatric research, 1996, 1:1–3.
- Brooke DG et al. Vitamin D supplements in pregnant Asian women: effects on calcium status and fetal growth. British medical journal, 1980, 280:751–4.
- Marya RK et al. Effects of vitamin D supplementation in pregnancy. Gynecologic and obstetric investigation, 1981, 12:155–61.
- Heaney RP et al. Human serum 25-hydroxy-cholecalciferol response to extended oral dosing with cholecalciferol. American journal of clinical nutrition, 2003, 77:204–10.
- Hollis BW. Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. Journal of nutrition, 2005, 135:317–2.
- West KP Jr et al. Double blind, cluster randomised trial of low dose supplementation with vitamin A or beta carotene on mortality related to pregnancy in Nepal. The NNIPS-2 Study Group. British medical journal, 1999, 318:570–5.
- Ghebremeskel K et al. Vitamin A and related essential nutrients in cord blood: relationships with anthropometric measurements at birth. Early human development, 1994, 39:177–88.
- Rondo PH, Abbott R, Tomkins AM. Vitamin A and neonatal anthropometry. Journal of tropical pediatrics, 2001, 47:307–10.
- Guajardo L et al. Ascorbic acid concentrations in umbilical cord veins and arteries of preterm and term newborns. Biology of the neonate, 1995, 68:1–9.
- Hou J et al. Maternal serum ferritin and fetal growth. Obstetrics and gynecology, 2000, 95:447–52.
- Rondo PH et al. Vitamin A, folate, and iron concentrations in cord and maternal blood of intra-uterine growth retarded and appropriate birth weight babies. European journal of clinical nutrition 1995, 49:391–9.
- Georgieff MK et al. Iron status at 9 months of infants with low iron stores at birth. Journal of pediatrics, 2002, 141:405–9.
- Hossain MM et al. The prevalence and correlates of anaemia among young children and women of childbearing age in Al-Ain, United Arab Emirates. Annals of tropical paediatrics, 1995, 15:227–35.



