M.T. Taher,1 S.M.H. Hashemi,1 M. Mohammadi 1 and F. Hashemi 1
1Infectious Diseases Unit, Department of Internal Medicine, Firoozgar University Hospital, Tehran, Islamic Republic of Iran (Correspondence to M.T. Taher:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
Received: 07/01/07; accepted: 12/06/07
EMHJ, 2009, 15(6):1617-1620
Introduction
Tuberculosis (TB) is a common disease in developing countries. According to a World Health Organization (WHO) report, the population of the Islamic Republic of Iran was 71 208 384 in 2007, with an estimated incidence of TB (all cases) of 22/100 000 population/year [1]. In 1999, the highest and lowest TB rates in the provinces of the country were 137/100 000 (Sistan va Baluchestan) and 10/100 000 (Khorasan) respectively [2]. The development of abdominal TB is independent of the pulmonary disease, with a reported incidence of co-existing disease varying from 5% to 36% [3]. Intra-abdominal TB usually involves the liver, spleen, bowel, peritoneum and mesenteric lymph nodes. Unusual presentations of digestive tract TB are more likely in immunocompromised patients [4].
Pancreatic TB is an extremely rare clinical entity [5]. We report here a case of pancreatic TB in a patient who presented with a pancreatic mass. To the best of our knowledge, the first report from the Islamic Republic of Iran.
Case report
A 51-year-old woman was referred to Firoozgar Teaching Hospital in February 2006 with epigastric pain unrelated to meals, fever, anorexia and weight loss: she had lost 3 kg over the previous 2 months. There was no history of pulmonary TB and physical examination was unremarkable.
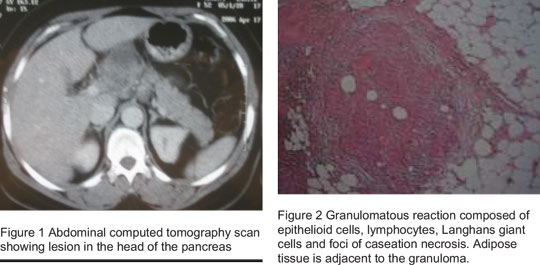
Laboratory evaluation revealed an increased erythrocyte sedimentation rate (80 mm/hr) and alanine aminotransferase (125 U/L), alkaline phosphatase was elevated (650 IU/L), tuberculin skin test with purified protein derivative 5 units giving an induration of 17 mm, HIV test was negative. Serum electrolyte, blood urea nitrogen, creatinine, bilirubin, amylase, lipase and chest radiography were all normal. Ultrasound of the abdomen revealed a mass in the region of the head of the pancreas. Abdominal computed tomography with contrast showed a heterogeneous mass with necrosis in the head and body of the pancreas and peripancreatic lymph nodes (Figure 1). The patient was referred for endo-ultrasonography and fine needle aspiration for a tissue diagnosis. This revealed a heterogeneous mass that was atypical for a malignancy. Fine needle aspiration was performed and revealed inflammatory cells with degenerative changes but neoplastic malformation could not be ruled out. The patient underwent exploratory surgery for diagnosis, and a mass with necrosis was seen in the head and body of the pancreas with multiple nodes seen in peripancreatic and perihepatic regions. Biopsies of the pancreas and lymph nodes showed inflammatory changes with multiple granuloma and caseous necrosis without evidence of malignancy (Figure 2). Staining for acid-fast bacilli and fungal organisms was negative. Based on these pathological findings, a diagnosis of pancreatic TB was made and the patient was put on antitubercular therapy (isoniazid, rifampin, pyrazinamide and ethambutol for 2 months followed by isoniazid and rifampin for the next 4 months).
On follow-up at 4 months, the patient was doing well, the fever and anorexia had gone and she had gained weight.
Discussion
Extrapulmonary TB is a diagnostic problem, especially when an unusual organ such as the pancreas is involved [6]. It is biologically protected from infection by Mycobacterium tuberculosis, probably because of the presence of pancreatic enzymes. Most cases of pancreatic TB arise from contiguous infection from peripancreatic lymph nodes or rarely from haematogenous spread [7].
Isolated pancreatic TB is rare in immunocompetent individuals. Auerback reviewed 1656 autopsies performed on TB patients and did not find any cases of isolated TB of the pancreas [8]. Bhansali reported no cases of pancreatic TB in a series of 300 cases of abdominal tuberculosis in India [9]. Xia and colleagues reported 16 patients from China with TB of the pancreas and peripancreatic lymph nodes; the predominant symptoms were abdominal pain (75%–100%), anorexia, weight loss (69%), malaise, weakness (64%), fever and night sweats (50%) [10]. Infrequently, pancreatic TB may present as acute pancreatitis with radiographic findings of pancreatic enlargement and oedema [11,12]. Other unusual presentations include obstructive jaundice, gastrointestinal bleeding, pancreatic abscess, chronic pancreatitis, diabetes and splenic vein thrombosis [13–18]. Laboratory abnormalities include anaemia, lymphocytopenia, hypertransaminasaemia and elevated alkaline phosphatase in approximately 50% of cases [10].
Our patient had no history of TB, her chest X-ray was normal, she had no other detectable foci of TB and acid-fast staining was negative. A culture of the pancreatic and lymph node tissue was not performed because tuberculosis was not initially suspected and the sample was sent to the pathology department for identification of malignant cells; however, bacteriological confirmation has been reported in only half of cases with extrapulmonary TB [19].
As the clinical and radiographic presentation mimics pancreatic cancer, preoperative diagnosis of pancreatic TB is rare. Most reported cases have been diagnosed at laparotomy, while there have been several cases diagnosed by the percutaneous fine-needle aspiration technique [20]. There is little experience in this technique in the Islamic Republic of Iran and unfortunately our patient underwent surgery. Diagnosis was based on the pathology and because the most common etiology of granulomatous disease in our country is TB. The patient was put on antitubercular therapy and she is doing well on follow-up of 4 months.
In conclusion, this case is important to report because there was no suspicion of TB before or during the operative period, and appropriate bacteriological testing was not carried out. In a developing country like the Islamic Republic of Iran, all physicians should be aware of the clinical features of pancreatic TB and conduct appropriate investigation (staining, culture and even polymerase chain reaction to detect mycobacteria). It is also necessary to increase experience in endo-ultrasonography and fine needle aspiration in our country.
References
- TB situation in the Region. Country profiles [website]. Cairo, World Health Organization Regional Office for the Eastern Mediterranean (http://www.emro.who.int/stb/pdf/CountryProfile-ira-07.pdf, accessed 10 February 2009).
- Sotoudeh Maram E, Fararoei M. Incidence of TB in cities of Fars. Journal of Qazvin University, 1999, 11:74–8.
- Hulnick DH et al. Abdominal tuberculosis: CT evaluation. Radiology, 1985, 157:199–204.
- Sunderam G et al. Tuberculosis as a manifestation of acquired immune deficiency syndrome (AIDS). Journal of the American Medical Association, 1986, 256:362–6.
- Kaushik N, Schoedel K, McGrath K. Isolated pancreatic tuberculosis of the pancreas diagnosed by endoscopic ultrasound-guided fine needle aspiration: a case report. Journal of the pancreas, 2006, 7(2):205–10.
- Hari S et al. Isolated tuberculosis of the pancreas diagnosed with needle aspiration: a case report and review of the literature. Tropical gastroenterology, 2005, 26 (3):141–3.
- Franco-Paredes C et al. Tuberculosis of the pancreas: report of two cases and review of literature. American journal of the medical sciences, 2002, 323:54–8.
- Auerback O. Acute generalized military tuberculosis. American journal of pathology, 1944, 20:121–36.
- Bhansali SK. Abdominal tuberculosis experience with 300 cases. American journal of gastroenterology, 1977, 67:324–37.
- Xia F et al. Tuberculosis of pancreas and peripancreatic lymph nodes in immunocompetent patients: experience from China. World journal of gastroenterology, 2003, 9(6):1361–4.
- Mourad FH, Mclean A, Farthing MJ. Tuberculous pancreatitis: a diagnostic problem. Case report and review of literature. Journal of clinical gastroenterology, 1995, 20:237–40.
- Rushing JL, Hanna CJ, Selecky PA. Pancreatitis as the presenting manifestation of miliary tuberculosis. West journal of medicine, 1978, 129:432–6.
- Crowson MC, Perry M, Burden E. Tuberculosis of the pancreas: a rare cause of obstructive jaundice. British journal of surgery, 1984, 71:239.
- Rolny P, Falk A, Olofsson J. Obstructive jaundice due to isolated tuberculosis of the pancreas: endoscopic treatment instead of surgery? Endoscopy, 2006, 38(1):90–2.
- Schaprio RH, Maher MM, Misdraji J. Case records of the Massachusetts General Hospital. Case 3-2006. A 63-year-old woman with jaundice and a pancreatic mass. New England journal of medicine, 2006, 354(4):398–406.
- Fan ST et al. Tuberculosis of the pancreas: a rare cause of massive gastrointestinal bleeding. British journal of surgery, 1986, 73:373.
- Stambler JB et al. Tuberculous abscess of the pancreas. Gastroenterology, 1982, 83:922–5.
- Patankar T, Prasad S, Laxminarayan R. Diabetes mellitus: an uncommon manifestation of pancreatic tuberculosis. Journal of the Association of Physicians of India, 1999, 47:938–9.
- Faver LS. Lowell AM, Meador MP. Extrapulmonary tuberculosis in the United States. American journal of epidemiology, 1979, 109:205–15.
- D’cruz S et al. Fine needle aspiration diagnosis of isolated pancreatic tuberculosis. A case report and review of literature. Journal of the pancreas, 2003, 4(4):158–62.



