P. Tabarsi,1 M. Mirsaeidi, 1 M. Amiri, 1 S. Karimi, 1 M.R. Masjedi1 and D. Mansouri1
1National Research Institute of TB and Lung Disease, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic of Iran (Correspondence to P. Tabarsi:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
Received: 14//06; accepted: 23/05/06
EMHJ, 2008, 14(5): 1217-1221
Introduction
Pneumocystis was first described in 1909 as an evolutionary phase in the life cycle of Trypanosoma cruzi by Chagas [1]. Later it was defined as a different organism [2]. Pneumocystis pathogenesis in humans was shown in 1951 for the fist time [3]. Recently, a species of Pneumocystis which afflicts humans was named Pneumocystis jiroveci [4].
Pneumocystis pneumonia (PCP) has remained as one of the most important opportunistic infections in patients infected with human immunodeficiency virus (HIV) [5,6]. In patients who have immune deficiency without HIV infection, pneumocystis is a major cause of morbidity and mortality [7,8]. In some studies, the use of steroids has been reported as a risk factor for PCP, particularly among patients suffering from cancer or connective tissue diseases [6–8]. In this article we present 2 cases of PCP that resulted from the incorrect use of corticosteroids.
Case reports
Patient 1
The patient was a 30-year-old male admitted to our hospital in January 2005 complaining of cough, sputum production, fever, chills and dyspnoea that had started 3 weeks before. He had lost 8 kg during this period. His condition had worsened 3 days before admission. The patient was married with 1 child. He had history of intravenous drug addiction but no history of imprisonment.
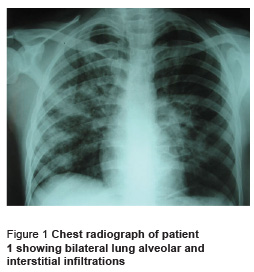
On examination, the patient had respiratory distress. Blood pressure was 110/70 mmHg, pulse 120 beats per minute, temperature 37.0 ºC and respiratory rate 40 breaths per minute. The patient had oral candidiasis. On cardiopulmonary auscultation the patient had tachycardia and fine crackles at the bases of both lungs. Blood analysis showed leukocyte count of 10 600 cells/μL (85% polymorphonuclear neutrophils, 6% lymphocytes) with total lymphocyte count of 660 cells/μL. Chest radiograph showed bilateral alveolar and interstitial infiltrations (Figure 1).
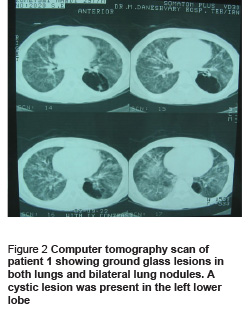
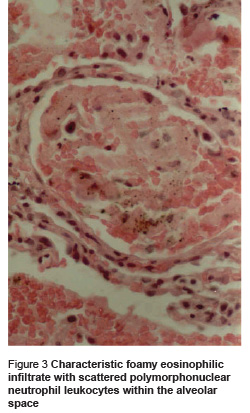
The patient was treated with ceftriaxone and erythromycin, but the next day dyspnoea worsened and oxygen saturation level reduced to 80%. Further history taking revealed that the patient has been using 200 mg prednisolone daily for 1 month before admission, for body building reasons. His therapeutic regimen was changed to 2 g intravenous ceftazidime every 8 hours, 1 g intravenous vancomycin every 12 hours and co-trimoxazole (20 mg/kg) in 4 divided doses. He was negative for HIV. Computer tomography (CT) scan showed ground glass lesions in both lungs with bilateral lung nodules. A cystic lesion was present in the left lower lobe (Figure 2). Bronchoscopy was performed and transbronchial biopsy showed eosinophilic foamy substances in some of the alveoli which were found positive for PCP with monoclonal antibody staining (Figure 3). Bronchoalveolar lavage for associated pathogens such Mycobacterium, Cytomegalovirus and Aspergillus was negative. Treatment with co-trimoxazole continued and prednisolone was added to the regimen because he was suffering from hypoxia. The patient was discharged with complete recovery after 4 weeks.
Patient 2
The patient was a 38-year-old female who presented to our hospital in March 2005 complaining of dyspnoea. She had a mild chronic cough lasting 4 months and had had several outpatient medical visits. She had been suffering from fever, chills and night sweats for 3 weeks and then progressive dyspnoea developed. Three days before admission she developed haemoptysis. The patient mentioned no history of prior illnesses. She reported using several antibiotics like co-amoxiclav and erythromycin for the recent illness.
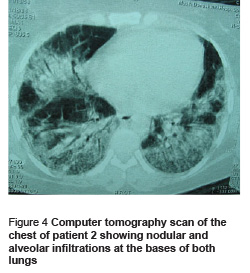
On physical examination, her temperature was 38.5 ºC, pulse 100 beats per minute and respiratory rate 15 breaths per minute. Cardiopulmonary auscultation revealed an II/VI systolic murmur and fine crackles at the base of both lungs. Chest radiograph showed nodular and alveolar infiltrations at the base of both lungs. The patient was treated with 1 g intravenous ceftriaxone every 12 hours and 400 mg erythromycin 4 times daily. Two days after admission, dyspnoea worsened and oxygen saturation level reduced to 80%. The leukocyte count was normal with 77% neutrophils and 14% lymphocytes (total lymphocytes 462 cells/μL). Complete history taking revealed that the patient had been taking 15 mg prednisolone daily for a month with the diagnosis of probable hyper-reactivity airway disease but without appropriate work up. The lung CT demonstrated alveolar and ground glass lesions in both lungs which were dominant in the base of the lungs (Figure 4).
Co-trimoxazole (20 mg/kg) in 4 divided doses and 4 mg dexamethasone every 6 hours were added to the patient’s therapeutic regimen and she was transferred to the intensive care unit. Bronchoalveolar lavage showed macrophages containing foamy substances which were found positive for PCP with monoclonal antibody staining. The patient underwent mechanical ventilation because of respiratory failure. However, despite all efforts, she died.
Discussion
PCP exclusively occurs in immunodeficient individuals; two-thirds of cases occur in HIV infected patients [9] and the other third in non-HIV patients who have haematological malignancies, solid organ tumours or are under immunosuppressive therapy [8,10,11]. Among immunosuppressive agents, the role of corticosteroids is the most prominent [12]. There is significant variability in the rate of response to steroid drugs among people [13]. Different reasons have been proposed to explain the effect of steroids in increasing the predisposition to P. jiroveci pneumonia, among them the reduction of CD4+ lymphocytes and deficient cell mediated immune activity are the most important [8,12].
PCP patients without HIV infection are often admitted because of acute respiratory failure following a decrease or increase in steroid dose [7,8]. These patients usually have a lower load of pneumocystis in the lungs compared to those with HIV infection [14]. The mortality rate of PCP is about 30% to 60% in non-HIV patients [6,15]. One of the reasons may be the fact that non-HIV patients have more neutrophils in the pulmonary interstitium which results in more severe inflammation and is associated with poor prognosis [14]. Another reason may be the delay in diagnosis of these patients because the respiratory manifestations may not be linked to the underlying disease. Therefore, in patients without HIV infection clinical suspicion is of great significance for diagnosis of P. jiroveci pneumonia.
The important feature in these 2 patients is the lack of specific underlying disease to guide the practitioner to diagnosis because neither of them mentioned the use of corticosteroids at the first visit. Nevertheless, the presence of diffuse oral candidiasis, lymphocytopenia and ground glass lesions in high resolution lung CT scans guided the physicians to the correct diagnosis. Therefore, precise history taking and thorough physical examination are fundamental diagnostic keys. At the same time, P. jiroveci pneumonia must be considered as a major differential diagnosis in the setting of oral candidiasis and peripheral blood lymphocytopenia, in patients receiving steroids who present with pulmonary complaints.
Another important point is the prevention of PCP in high-risk patients. There are certain guidelines for prevention in HIVinfected patients (fewer than 200 CD4 lymphocytes or diffuse oral candidiasis) [16]. Prophylactic drugs are also recommended in patients without HIV infection who receive immunosuppressive drugs or have primary or acquired immune deficiency [6–8]. One of the prophylactic strategies in these patients has been proposed by Sowden and Carmichael [17]. They have recommended that CD4 lymphocytes should be counted in the following circumstances:
- Steroids use > 15 mg of prednisolone daily.
- Steroids use > 3 months.
- Total lymphocytes < 600 cells/μL. If CD4 count in these circumstances is below 200 cells/μL, co-trimoxazole is recommended for prophylaxis, although more studies are needed [17].
In conclusion, this report emphasizes the importance of the proper use of steroids to prevent untoward complications as happened in our 2 patients. In addition, the role of thorough history taking must not be underestimated. Finally, we recommend considering P. jiroveci pneumonia as a major differential diagnosis in patients receiving steroids who present with pulmonary complaints associated with oral candidiasis and lymphocytopenia.
References
- Chagas C. Nova trypanosomiaza humana. Estudos sobre amorphologia eociclo evolutivo do schizotrypanuma cruzi, n. gen.N.SP, ajente etiologicode nova entidade morbida de homen [New human trypanosomiasis. Studies about the morphology and life-cycle of Schizotripanum cruzi, etiological agent of a new morbid entity of man]. Memórias do Instituto Oswaldo Cruz, 1909, 1:159–218.
- Delanoe A, Delanoe M. Sur les rapports der kystes de carinii du pulmondes rats avec Trypanosoma lewisii. Comptes rendus de l’Académie des sciences Paris, 1912, 155:658.
- Vanek J. [Atypical (interstitial) pneumonia in children caused by Pneumocystis carinii]. Casopis lekaru ceskych, 1951, 21, 90(38):1121–4.
- Stringer JR et al. A new name (Pneumocystis jiroveci) for pneumocystis from humans. Emerging infectious diseases, 2002, 8:891–6.
- Centers for Disease Control and Prevention. HIV/AIDS surveillance supplemental report, 2003, 9(3):1–20.
- Sepkowitz KA. Opportunistic infections in patients with and patients without acquired immunodeficiency syndrome. Clinical infectious diseases, 2002, 34:109–7.
- Sepkowitz KA et al. Pneumocystis carinii pneumonia among patients without AIDS at a cancer hospital. Journal of the American Medical Association, 1992, 267:832–7.
- Yale SH, Limper AH. Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illness and prior corticosteroid therapy. Mayo Clinic proceedings, 1996, 71:5–13.
- Safrin S. Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. Seminars in respiratory infections, 1993, 8:96–103.
- Roblot F et al. Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. European journal of clinical microbiology and infectious diseases, 2002, 21:523–31.
- Nuesch R, Bellini C, Zimmerli W. Pneumocystis carinii pneumonia in human immunodeficiency virus (HIV)-positive and HIV-negative immunocompromised patients. Clinical infectious diseases, 1999, 29:1519–23.
- gnibene FP et al. Pneumocystis carinii pneumonia: a major complication of immunosuppressive therapy in patients with Wegener’s granulomatosis. American journal of respiratory and critical care medicine, 1995, 151:795–9.
- Hearing SD et al. Wide variation in lymphocyte steroid sensitivity among healthy human volunteers. Journal of clinical endocrinology and metabolism, 1999, 84:4149–54.
- Limper AH et al. Pneumocystis carinii pneumonia: differences in lung parasite number and inflammation in patients with and without AIDS. American review of respiratory disease, 1989, 140:1204–9.
- Pareja JG, Garaland R, Koziel H. Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest, 1998, 113:1215–24.
- Masur H, Kaplan JE, Holmes KK. Guidelines for preventing opportunistic infections among HIV-infected persons – 2002: recommendations of the US public health service and infectious diseases society of America. Annals of internal medicine, 2002, 137:435–78.
- Sowden E, Carmichael A. Autoimmune inflammatory disorders, systemic corticosteroids and pneumocystis pneumonia: A strategy for prevention. BMC infectious diseases, 2004, 4(42):2334–42.



