R. Güven,1 H. Özcebe2 and B. Çakır2
ABSTRACT Turkey is an intermediate endemic area for hepatitis B virus infection. The study investigated the hepatitis B exposure risk and prevalence of hepatitis B infection in a group of workers of no known occupational exposure. The prevalence of seropositivity for hepatitis B surface antigen (HBsAg), hepatitis B surface antibody (anti-HBs) and hepatitis B core antibody (anti-HBc) were 6.6%, 29.9%, and 50.6% respectively. Hepatitis B infection rates were also high in the families of HBsAg-positive workers; 73.7% of family members were positive for HBsAg, anti-HBs or anti-HBc. Risk factors included ever having an injection by an unqualified practitioner (14.6%) and ever having unprotected extramarital intercourse (62.5%).
Prévalence de l’hépatite B chez des travailleurs présentant un faible risque d’exposition à l’hépatite B en Turquie
RÉSUMÉ La Turquie est une zone d’endémie intermédiaire pour l’infection par le virus de l’hépatite B. Cette étude avait pour but d’examiner le risque d’exposition à l’hépatite B et la prévalence de l’infection par le virus de l’hépatite B dans un groupe de travailleurs sans exposition professionnelle connue. La prévalence de la séropositivité pour l’antigène de surface du virus de l’hépatite B (Ag HBs), pour les anticorps dirigés contre l’antigène de surface du virus de l’hépatite B (anti-HBs) et pour les anticorps dirigés contre l’antigène central du virus de l’hépatite B (anti-HBc) s’élevait à 6,6 %, 29,9 % et 50,6 % respectivement. Les taux d’infection par le virus de l’hépatite B étaient également élevés dans les familles de travailleurs antigène HBs positif ; 73,7 % des membres de la famille étaient positifs pour l’antigène HBs, les anticorps anti-HBs ou les anticorps anti-HBc. Les facteurs de risque comprenaient le fait d’avoir déjà reçu une injection par un praticien non qualifié (14,6 %) et d’avoir déjà eu des rapports extraconjugaux non protégés (62,5 %).
1Ministry of Labour and Social Security, Ankara, Turkey (Correspondence to R. Güven:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
2Department of Public Health, Faculty of Medicine, Hacettepe University, Ankara, Turkey.
Received: 17/02/04; accepted: 11/04/05
EMHJ, 2006, 12(6): 749-757
Introduction
More than 350 million people in the world are currently estimated to be chronically infected with the hepatitis B virus (HBV), and 2 billion people have serological markers indicating present or previous infection with the virus [1]. HBV causes a number of liver diseases, ranging from acute and chronic hepatitis, cirrhosis to primary liver cancer. HBV is the most clearly identified cause of cancer after tobacco smoking [2].
The main modes of HBV transmission are perinatal, horizontal, parenteral and sexual, and the relative rates of these vary throughout the world [1,2]. Parenteral and sexual transmission predominates in industrialized countries, whereas horizontal and perinatal transmission predominates in developing countries [1]. Horizontal transmission of HBV, particularly among young children, occurs predominantly in countries of the Eastern Mediterranean Region, Africa, India and Turkey [1,3–5]. It is claimed that horizontal transmission usually occurs via inapparent percutaneous routes, through cuts and lesions [1,2].
HBV is generally associated with poor socioeconomic conditions. The regions of the world can be classified into areas of high, intermediate and low HBV endemicity. The Eastern Mediterranean Region has high and intermediate endemic areas [2,6,7]. As an intermediate endemic area, 20%–55% of Turkey’s population has serological evidence of past or current exposure to HBV infection, and the prevalence of hepatitis B surface antigen (HBsAg), the indicator of acute HBV infection, ranges between 2% and 10% [8–10]. The prevalence of HBsAg positivity in various risk groups ranges between 4% and 10% and the prevalence of hepatitis B core antibody (anti-HBc) positivity (indicating current or previous exposure to HBV infection) ranges between 26.2% and 68.8% [9]. HBV in Turkey is not only a problem for high-risk individuals, but may also be an important health risk for all members of society.
In this study in Ankara, Turkey, the prevalence of HBV infection and markers of previous exposure were investigated in a group of workers at low-risk of HBV exposure.
Methods
A cross-sectional study investigated HBV infection in a group of low-risk workers with no known professional HBV exposure. Risk of exposure to HBV was evaluated by a questionnaire and the serological markers of HBV infection or exposure were measured. The study was conducted among staff of the Provincial Directorate of Rural Services, Ankara, which provides public services to villages. These public services include protection and improvement of the soil and water and preparation and implementation of programmes and projects for rural areas. The institution includes an occupational health office, where a full-time occupational physician works.
A total of 655 workers were employed by the Provincial Directorate of Rural Services in the study year (1996). Of workers contacted for the study, 604 (92.2%) were reached, and agreed to participate (581 were males). The occupational physician at the Provincial Directorate of Rural Services completed a standardized questionnaire for each worker during a face-to-face interview and collected information on the socio-demographic characteristics of the worker and exposure to risk factors for HBV infection. The questionnaire included 63 questions on the worker’s background characteristics, the worker’s exposure to risks of HBV infection and knowledge level about HBV infection. The exposure risks were: having had an injection, medical operation or blood test, using a barber, having sexual partners before or after marriage and if so whether condoms were used or not. Data on HBV-related knowledge are not presented in this paper.
Blood samples were obtained from study participants and family members after obtaining individuals’ informed consent verbally. Each of them was aware of the aim of the study and what the blood samples were tested for. Additionally, written approval for the study was obtained from the Provincial Directorate of Rural Services. Blood sampling was supervised by the lead author, who was the occupational physician in charge at the time of study, and samples were transferred to the laboratory in a standardized manner. HBsAg, hepatitis B surface antibody (anti-HBs) and anti-HBc titres were measured by enzyme-linked immunosorbent assay (ELISA) at the Department of Clinical Microbiology of Ankara Training Hospital, which is responsible for providing health services to all workers. If the worker was positive for HBsAg, he/she was tested for hepatitis Be antigen (HBeAg), hepatitis Be antibody (HBeAb), hepatitis B immunoglobulin M antibody (HBcIgM) and hepatitis B immunoglobulin G antibody (HBcIgG). Similarly, when the worker was positive for HBsAg, blood samples were taken from his/her family members and tested for markers of hepatitis B exposure (HBsAg, anti-HBs, anti-HBc).
Following the interviews, a standardized face-to-face health education session was provided to each worker and his/her relatives (preferably with all individuals coming from the same family as a group) about HBV infection, risk factors and prevention methods. Also, a conference and two seminars on the same topic were conducted for all the workers together. A similar education was provided for family members of HbsAg-positive workers. As part of the study, all HbsAg-positive workers and family members of HBsAg-positive workers were vaccinated against HBV infection.
Statistical analyses included frequency tables, chi-squared tests for testing the significance of difference between proportions and multivariate analysis. Multivariate logistic regression analysis was conducted to study the association between exposure to HBV (i.e. past or ongoing HBV infection versus no exposure) and various risk factors. All analyses were conducted using Epi-Info, version 5.0, and SPSS, version 9.0 statistical software packages.
Results
Background characteristics
The age of workers ranged between 21 and 51 years; the mean (standard deviation) age was 41.1 (5.9) years. Almost all of them were males (96.2%). More than half of the workers (64.1%) had finished primary school, and only 3.5% had a college education. Almost all the workers (95.9%) were married with an average of 2.8 children.
Serological tests
The serological tests could be completed for 571 participants. Overall 49.2% of study participants (281/571) had never been exposed to HBV infections (Figure 1). Of the remainder who had been exposed, 6.6% (38/571) of workers were HBsAg-positive and anti-HBc-positive, indicating late acute or chronic HBV infection. Two (2) individuals had chronic HBV infection, and were contagious. One (1) worker was anti-HBs-positive who had been vaccinated for HBV infection. Both anti-HBs antibodies and anti-HBc antibodies were detected in 29.8% (170/571) of workers, while 14.2% (81/571) were positive for anti-HBc antibodies only, indicating they were healthy individuals with previous HBV infection. Thus 289/571 (50.6%) workers had current infection or exposure to HBV infection.
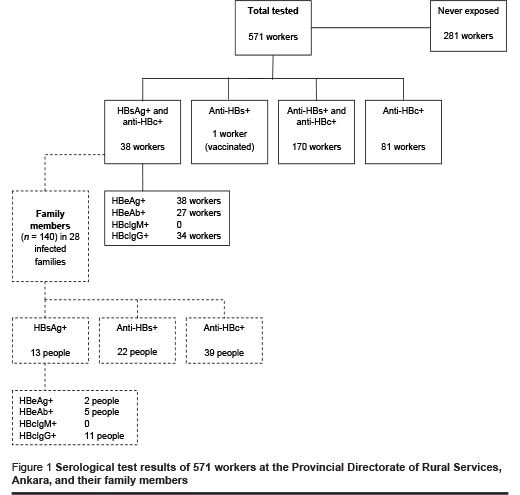
Of the 38 workers who were positive for HBsAg, 28 (73.7%) had at least one family member who was seropositive for HBV infection (i.e. HBsAg+, anti-HBs+ or anti-HBc+). The wife only was seropositive for 14 (36.8%), the wife and at least one child for 6 (15.8%), at least one child for 4 (10.5%), the wife and at least one family member for 2 (5.3%) and the wife, child and at least one family member for 2 (5.3%). Table 1 shows the serological finding for the family member of HBsAg-positive workers. Among family members of the 38 HBsAg-positive workers, 15.7%, 27.9%, and 9.3% were positive for anti-HBs, anti-HBc, and HBsAg respectively. As expected, HBV seropositivity was more prevalent among wives of the infected workers than their children, parents and other family members.
Risk behaviour
The interviews showed that although the study participants were not in any special risk group for HBV infection, 598/604 (99.0%) had been exposed to at least one HBV infection risk factor for hepatitis B infection in their lifetime (Table 2). Almost all workers had had at least one injection in their lifetime. The places they had chosen for injection varied: some people, particularly the older ones, had been injected by an inexperienced person at home or by an unlicensed pharmacist (14.6%) (Table 3).
A major risk-taking behaviour for hepatitis B transmission is unsafe sex: out of 581 male workers responding, 27.0% reported ever having extramarital sexual intercourse before marriage and 36.5% currently had extramarital intercourse. The great majority of those who had had intercourse prior to marriage (148/157; 94.3%) and of those currently having extramarital intercourse (190/212; 89.6%) reported that they never used a condom. Thus a total of 62.5% had ever had unprotected extramarital intercourse.
Logistic regression analysis
The effect of individual risk factors on seropositivity (i.e. HBsAg+, anti-HBs+ or anti-HBc+) was evaluated in multiple logistic regression analysis. In modelling the following were included as potential risk factors: age group (age above average, i.e. 42+ years versus < 42 years), shaving (yes versus no), haircut at the barber (yes versus no), using razor blade for hair trimming (yes versus no), having any surgical operation (yes versus no), ever had extramarital sexual intercourse (yes versus no). Using backward elimination (at α = 0.05), age was the only statistically significant risk factor for HBV seropositivity (P = 0.002) and risk was higher in older workers. The effect of condom use on HBV seropositivity could not be evaluated alone because condom use was only asked to individuals who had ever had extramarital sexual intercourse.
Discussion
In this study of professionals with no known HBV infection risk, the prevalence of sero-positivity for HBsAg and anti-HBc antibody was 6.6% and anti-HBs and/or anti-HBc seropositivity were detected in 44.0% of the workers respectively. These rates are higher than the reported prevalence of HBV infection in populations of industrialized countries [1,6], but similar to figures in different Middle Eastern countries [7], consistent with the fact that Turkey is located in a semi-endemic region regarding the prevalence of hepatitis B infection. Previous research in Turkey has suggested that HBsAg-seropositivity among high-risk individuals, including health personnel, haemodialysis patients and sex workers, ranges between 3.5% and 54.0%, whereas the HBsAg-seropositivity is between 4.8% and 17.4% among low-risk individuals [8–10]. Total seropositivity (i.e. HBsAg+ or anti-HBs+ or anti-HBc+) rates obtained from previous studies on the Turkish population ranged between 26.2% and 68.8%, indicating that up to two-thirds of the population is currently or previously infected with HBV [8]. The frequency of any exposure to HBV was found to be 50.6% in the study population, indicating that about 1 in 2 individuals had been infected with hepatitis virus at some point in their lives. The findings indicate that hepatitis B virus is not a problem of high-risk groups only, but that all members of society are at-risk for HBV infection.
Almost all the study participants reported exposure to at least one HBV infection risk factor and the most commonly reported risk factor was having an injection, often outside hospitals or doctors’ clinics; 14.6% of the study participants reported having had at least one injection at home by an experienced person or by an unlicensed pharmacist. Unqualified injectionists obtain their injection skills through a “master–
apprentice relation” and it is not known to what extent they are knowledgeable about blood-transmitted diseases and the need for precautions against them. Injection by experienced/unlicensed people was common practice in Turkey before the 1980s when health centres were not established throughout the country, and disposable syringes and needles were not in use. After the national vaccine campaign in 1985, use of disposable injection kits gained wide acceptance all over the country. Given the current health education activities about the risk factors for bloodborne diseases and related preventive measures, the younger generation is expected to be less at-risk of infection due to contaminated injections.
The high rate of HBV infection among the study participants could be due to the high rate of extra-marital sexual relationships (among nearly one-third of the men), and non-use of condoms in about 90% of those having extramarital intercourse. Condom use is not a common behaviour among men in Turkey, even in situations where their sexual partners are expected to have high probability of hepatitis B infection. Unsafe sex in extramarital relations is likely to increase the transmission of hepatitis B infection and could, at least partially, explain the high rates of hepatitis B infection in the study population.
In this study, occurrence of HBV infection was also investigated for family members of HBsAg positive workers. In 73.7% of HBsAg positive workers, at least one family member was also seropositive for HBV infection (i.e. HBsAg+, anti-HBs+ or anti-HBc+). This figure is higher than HBV infection rates among wives and family members of blood donors and health personnel, which has been reported as 33%–71% [3]. Kuru et al. evaluated the HBV titres in husbands and other family members of Turkish pregnant women: 59.1% of family members showed serological evidence of previous or ongoing HBV infection, and 27.1% of family members were positive for HBsAg. Kuru et al. also reported high rates of HBV infection among wives, children, and other family members of workers who were positive for hepatitis B antigen [4]. Studies conducted in the Eastern Mediterranean Region have shown evidence of horizontal transmission within families [5,7]. Horizontal transmission of HBV infection was also discussed in some studies conducted to explain the prevalence of hepatitis B among children [11,12] and among the members an American football team [13].
The likelihood of hepatitis B infection in a low-risk group was examined in this study. It was observed that the HBV exposure risk among low-risk workers and their family members was higher than expected and these rates were not significantly different than that expected for high-risk groups. This indicates that hepatitis B virus infection is a public health problem for all individuals in society, regardless of their professional risks or personal risk-taking behaviours. Recently, HBV infection has been included in the list of priority health concerns of the Turkish Ministry of Health. Risk factors for HBV infection, routes of transmission and potential preventive measures have been included in health education programmes and supported by the mass media. Hepatitis B vaccine has been included in the routine infant immunization scheme in Turkey since 1997. Risk groups such as health personnel and security forces are tested periodically and are vaccinated. However, given the high seropositivity rates of HBV infection, education about bloodborne infections and vaccination of high-risk groups/infants will not be adequate alone to control the HBV infection. Nor it is practical to advocate universal HBV screening or vaccination of all susceptible people. However, patients admitted to hospitals for any reason could be tested for HBV and if they are found to be positive, examinations could be extended to their family members. Screening of pregnant women for HBV infection should be routinely conducted during prenatal care in hospitals.
It is recommended that greater awareness is needed in society about the ways of transmission of hepatitis B infection and preventive measures should be improved. The risks of horizontal transmission of hepatitis B should be emphasized in the health education programmes in Turkey and countries of the Eastern Mediterranean Region. An increase in awareness of the population of the risks of HBV infection and of potential preventive measures will definitely improve the control of HBV infection nationwide and will eventually decrease the associated health care costs.
Acknowledgement
The authors wish to thank Dr Ali Mert, Head of Clinical Microbiology, Training Hospital of Social Insurance, for his assistance in analysis.
References
- Hepatitis B. Geneva, World Health Organization, 2000 (Factsheet No. 204). (http://www.who.int/mediacentre/factsheets/fs204/en/index.html, accessed 26 March 2006).
- Grosheide P, Van Damme P. Prevention and control of hepatitis B in the community. Geneva, WHO Viral Hepatitis Prevention Board, 1996 (Communicable Disease Series, No.1).
- Çakalglu Y et al. Horizontal transmission of hepatitis B virus infection. Journal of hepatology, 1992; 15:256–6.
- Kuru U et al. Prevalence of hepatitis B virus infection in pregnant Turkish women and their families. European journal of clinical microbiology & infectious diseases, 1996, 15:248–51.
- Zali MR et al. Epidemiology of hepatitis B in the Islamic Republic of Iran. Eastern Mediterranean health journal, 1996, 2(2):290–8.
- Fessard C et al. Hepatitis A and B prevention strategies: a single approach? Abingdon, The Medicine Group, 1996.
- Qirbi N, Hall AJ. Epidemiology of hepatitis B virus infection in the Middle East. Eastern Mediterranean health journal, 2001, 7(6):1034–45.
- Kılıçturgay K, Mıstık R. Viral hepatitis B in Turkey. In: Kılıçturgay K, ed. Viral hepatitis 94. Istanbul, Viral Hepatitle Savasım Dernegi, 1994 [in Turkish].
- Çakalglu Y, Ökten A, Yalçın S. Seroepidemiology of hepatitis B infection in Turkey. Turkish journal of gastroenterology, 1990, 1:49–53.
- Badur S. The status of viral hepatitis in Turkey. Report of the Association for the Fight Against Viral Hepatitis. In: Kılıçturgay K, ed. Viral hepatitis 94. Istanbul, Viral Hepatitle Savasım Dernegi, 1994:15–38 [in Turkish].
- Vall Mayans M et al. Risk factors for transmission of hepatitis B virus to Gambian children. Lancet, 1990, 336:1107–9.
- Botha JF et al. Hepatitis B virus carrier state in black children in Ovamboland: role of perinatal and horizontal infection. Lancet, 1984:1209–12.
- Tobe KZ et al. Horizontal transmission of hepatitis B virus among players of an American football team. Archives of internal medicine, 2000, 160:2541–9.



