N.A. Ahmadi,1,2 M. Modiri 2 and S. Mamdohi 3
المسح الأول لداء الليشمانيات الجلدي في مقاطعة بروجرد، غربيَّ جمهورية إيران الإسلامية
نايب علي أحمدي، مونا مديري، شهرام ممدوحي
الخلاصة: لم تكن منطقة لرستان في جمهورية إيران الإسلامية معروفة سابقاً كبؤرة لداء الليشمانيات الجلدي. وقد أجريت دراسات سريرية ووبائية على المرضى الذين تم تشخيص إصابتهم النشطة بداء الليشمانيات الجلدي في المختبر المركزي في مدينة بروجرد في المدَّة 1998-2010. وجرى دراسة ما مجموعه 137 مريضا تأكدت إصابتهم بداء الليشمانيات الجلدي (يبلغ متوسط معدل الوقوعات السنوي التقديري 4.36 لكل مئة ألف نسمة). وبلغت نسبة الذكور إلى الإناث أكثر من 11: 1. وتراوح عمر المرضى بين 8-63 سنة، ولكن أكثر من ٪70 منهم تراوحت أعمارهم بين 21-40 عاماً، وكان عمر حالة واحدة فقط ≥ عشرة أعوام. وكان معدل داء الليشمانيات الجلدي أعلى في سكان الريف (٪56.9)، وبين العمال (٪38.0)، والسائقين (٪32.8). وكان معدل الآفات النشطة في الأطراف العلوية (٪69.3) أعلى بكثير من سائر الأماكن. وكانت حالات القروح الجافة (٪57.7) أكثر من القروح الرطبة (٪42.3). وكان لدى غالبية المرضى (٪61.3) آفة واحدة نشطة (بمتوسط 1.8 قرحة لكل مريض). ويعد هذا هو التقرير الأول عن داء الليشمانيات الجلدي في المنطقة.
ABSTRACT Lorestan province in the Islamic Republic of Iran has not previously been known as a focus for cutaneous leishmaniasis (CL). Clinical and epidemiological studies were carried out on patients diagnosed with active CL at the central laboratory in Borujerd city during 1998–2010. A total of 137 patients with corroborated CL were studied (mean estimated annual incidence 4.36 per 100 000 inhabitants). The male:female ratio was > 11:1. Patients ranged in age from 8–63 years but > 70% were aged 21–40 years and only 1 was ≤ 10 years. The rate of CL was highest in rural residents (56.9%) and among those working as labourers (38.0%) and drivers (32.8%). The rate of active lesions on the upper limbs (69.3%) was significantly higher than other locations, and more cases were dry sores (57.7%) than wet sores (42.3%). The majority of patients (61.3%) had a single active lesion (mean 1.8 ulcers per patient). This is the first report of CL in the area.
Première enquête sur la leishmaniose cutanée dans le comté de Borudjerd (à l'ouest de la République islamique d’Iran)
RÉSUMÉ La province du Lorestan (République islamique d’Iran) n’était pas jusqu’à présent connue comme un foyer de leishmaniose cutanée. Des études cliniques et épidémiologiques ont été menées auprès de patients ayant reçu le diagnostic de leishmaniose cutanée active au laboratoire central de la ville de Borudjerd entre 1998 et 2010. Au total, les dossiers de 137 patients dont le diagnostic avait été confirmé ont été étudiés (incidence annuelle moyenne estimée à 4,36 pour 100 000 habitants). Le rapport homme-femme était supérieur à 11 pour 1. L’âge des patients se situait entre 8 et 63 ans mais plus de 70 % d’entre eux appartenaient à la tranche d’âge 21-40 ans et un seul patient avait un âge inférieur ou égal à 10 ans. Le pourcentage de leishmaniose cutanée était plus élevé chez les habitants en milieu rural (56,9 %), les cultivateurs (38,0 %) et les chauffeurs (32,8 %). Le pourcentage de lésions actives sur les membres supérieurs était nettement supérieur (69,3 %) que pour les autres sites, et les formes sèches étaient plus nombreuses (57,7 %) que les formes humides (42,3 %). La majorité des patients (61,3 %) étaient porteurs d’une seule lésion active (moyenne : 1,8 ulcère par patient). Il s’agit de la première notification de leishmaniose cutanée dans la région.
1Proteomics Research Centre; 2Department of Medical Laboratory Technology, Faculty of Paramedical Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic of Iran (Correspondence to N.A. Ahmadi:
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
;
This e-mail address is being protected from spambots. You need JavaScript enabled to view it
).
3Health Centre, Borujerd, Islamic Republic of Iran.
Received: 15/01/12; accepted: 22/05/12
EMHJ, 2013, 19(10):847-853
Introduction
Leishmaniasis is a vector-born parasitic disease caused by a protozoan, Leishmania spp. The disease is endemic in many tropical and subtropical regions in at least 88 countries of the world. The annually estimated incidence of cutaneous leishmaniasis (CL), the most common and disfiguring form of the disease, is 1–1.5 million cases and of the visceral form is 500 000 cases [1,2]. Emergence or re-emergence of CL has recently occurred in many countries [3–6]. CL has been prevalent in some provinces of the Islamic Republic of Iran, including Isfahan [7,8], Shiraz [9], Khorasan [10], Khuzestan and Kerman [11,12]. The disease has also emerged in new foci of the country during recent decades [9,13,14].
Lorestan province (particularly Borujerd county) has not previously been known as an important area for CL. However, the province is located adjacent to Khuzestan, Ilam and Isfahan provinces, where there are important endemic foci of CL. The disease is potentially a serious and increasing public health problem in the area, and in recent years cases of CL have been diagnosed in health centres and local clinics. It is important to be aware of the epidemiological features of the disease as a prerequisite for implementing control measures. Considering the lack of data on the status of CL in the region, the present study was conducted to determine the epidemiological and clinical characteristics of the disease in this new focus.
Methods
Study area and community
The investigation was carried out in Borujerd county, which is situated 100 km north-east of Khorramabad, the capital of Lorestan province, in the west of the Islamic Republic of Iran. The county is located between latitude 33°36′ N 48°27′ E to 34°6′ N 49°27′ E, with an area of 1606 km2. Borujerd city is located approximately 1670 m above sea level and has a moderate climate with cold winters. The maximum and minimum temperature recorded are 38 °C and −18 °C in July and January respectively, with the mean value annual temperature about 14.6 °C. Average annual precipitation is about 480 mm, mostly decreasing in the spring and winter.
The region had a population of 320 574 at the last census in 2006 (227 547 urban and 93 027 rural). Agricultural land in Borujerd is rich and fertile with good pasture, providing opportunities for farming and animal husbandry. The vegetation of the area includes herbs, edible fruits (apples, cherries, grapes, pears), wheat, barley, beetroot, maize, legumes, oilseed and alfalfa, and a considerable area of Borujerd county is covered with oak and juniper forests. The area is paved with highways and is a crossroads between Tehran and Khuzestan as well as Isfahan and Kermanshah provinces. Many Lurs and Bakhtiari nomads move to the foot of the surrounding Zagros mountains in summer and this migration of people from endemic to non-endemic areas of the region, for example the annual migration of nomads between this area and Khuzestan province, may be the main factors responsible for emergence of the disease.
Patients and laboratory methods
This study was carried out on all clinically suspected cases of CL referred to the central laboratory in Brojerd city for parasitological diagnosis from different parts of the county during March 1998 to February 2010. Under light microscopic examination, at least 2 Giemsa-stained slides for each patient were prepared with smears from scrapping of the edge of ulcers, and then microscopically checked for amastigote stage.
For each positive case with ulcer(s), a form was completed to record the necessary demographic data and clinical information such as age at the time of diagnosis, sex, occupation, place of residence, number of ulcer(s), clinical form and site of ulcer(s). Possible travelling experience and date of travelling to other endemic areas inside or outside the country were also recorded.
The incidence was collected on a monthly basis. This time interval was chosen as being likely to indicate any seasonal trends or variation. The annual active lesion incidence of CL (number of cases per 100 000 inhabitants) was estimated. Similarly, the proportion of cases from rural settings was compared with the proportion of the general population in rural settings.
Data analysis
The statistical significance of differences between age groups, between 2 proportions, and between ulcer location frequencies was evaluated using the chi-squared test, by calculating the Z statistic and Student t-test respectively. A P-value of < 0.05 was considered indicative of a statistically significant difference.
Results
A total of 137 patients with corroborated CL were investigated over the study period.
The annual distribution of active cases according to the place of residence and incidence per 100 000 inhabitants is shown in Table 1. The annual ulcer (active lesion) incidence of CL over the 12 years of study was estimated to be 4.36 cases per 100 000 inhabitants, varying between 1.87 per 100 000 in 2001–2002 and 8.42 cases per 100 000 in 2007–2008.
In interviews a number of patients stated that they had not travelled to other endemic areas (inside or outside the country) at least 1 year prior to their contraction of the ulcer. However, a large majority of active cases were patients who had travelled to the endemic areas of the disease such as Isfahan, Kerman province (Bam and Kerman), Khuzestan province (Bandar Imam and Ahwaz), Khorasan province, Chabahar (Sistan va Baluchestan province), Bandar Abbas and Bushehr. Rural dwellers were significantly over-represented among the cases (56.9%) as only 29.0% of the general population of Borujerd county (in the 2006 census) were living in rural areas (P < 0.001).
There were significant differences in the rate of active lesions between males (92.0%) and females (8.0%), a male:female ratio of 11.5:1 compared with 1.04:1 in the general population of Borujerd county (P < 0.001).
The mean age of patients was 30.5 years, range 8–63 years, and all age groups appeared to be susceptible to infection. The highest proportion of patients grouped within the age of 21–30 years (36.5%) and 31–40 years (35.0%). Only 1 patient (0.7%) was in the age group ≤ 10 years and 3 (2.2%) patients were > 50 years old (Table 2).
Cases of dry sores were more common than wet sores (57.7% versus 42.3%) and both types of sore were significantly more common in males than females (P < 0.05).
A total of 247 active lesions were observed among the 137 patients, i.e. an average number of 1.80 lesions per person (1.75 in males and 2.36 in females). The majority of patients (61.3%) were had only 1 ulcer, and the remaining had more than 1 ulcer The maximum number of sores was 7, occurring in 2 patients.
The rate of active lesions on the upper limbs (69.3%) was significantly higher than that of ulcers in other locations (P < 0.05). The second most frequent location was the lower limbs (44.5%) (Table 3). However, in female patients, the face and upper limbs were equally affected (6.9% and 5.8% respectively). In male patients, the pattern was very different; 62.8% of ulcers appeared on upper limbs and only 3.7% were observed on the face (Table 3).
Analysis by occupation showed that the highest rate of infection was among labourers (38%), followed by drivers (32.8%) (Figure 1). The seasonal variation showed that the highest and lowest rates of infection were observed in the spring (May, April and June) and winter (January, February and March) (32.1% and 18.2% respectively) (Figure 2).

Figure 1 Occupations of 137 confirmed cases of cutaneous leishmaniasis in Borujerd county, western Islamic Republic of Iran, 1998–2010
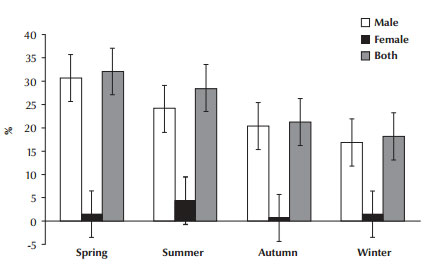
Figure 2 Seasonal incidence of confirmed cases of active cutaneous leishmaniasis in Borujerd county, western Islamic Republic of Iran, 1998–2010
Discussion
CL poses an important socioeconomic and public health problem in many areas of the world. CL is still a notifiable endemic disease in Islamic Republic of Iran and is prevalent in some provinces of the country [8,10,12,14]. At a particular geographical location where the disease was sporadic in the past, it has become endemic and/or is reaching epidemic proportions. It has even spread into new regions that previously did not report CL [9,13,14].
This is the first time that a focus of CL has been identified and reported in Borujerd county. Between the study dates of 1998–2010, the lowest incidence of infected cases was reported in 2001–02 (4.4%) and the highest in 2007–08 (19.7%). According to interview statements, the subjects had never left their residential areas, indicating that this was local transmission. This further confirms that the CL cases emerged in Borujerd county and that this is a new endemic focus in the area. However, a large majority of patients with active CL reported that they had travelled to endemic areas such as Isfahan, Kerman province (Bam and Kerman), Khuzestan province (Bandar Imam and Ahwaz), Mashhad (Khorasan province), Chabahar (Sistan va Baluchestan Province), Bandar Abbas, Bushehr. In terms of the annual numbers of CL cases presenting for diagnosis each year, the estimated incidence of ulcerative lesions for Borujerd (about 4.36 cases per 100 000) was lower than the corresponding values reported for other areas in the Islamic Republic of Iran [10,12–14], Pakistan [15], Afghanistan [16] and some other countries [3,4,17].
Although most of Borujerd’s population are urban dwelling (71% at the last census in 2006), more of the affected patients (56.9%) lived in rural areas. Therefore, rural life seems to a risk factor for CL in the region.
In the present study, the rate of active lesions among males was more than 11 times that of females, while the male:female ratio in the general population of Borujerd county was 1.04 (P < 0.001). This finding contrasts with many studies reported elsewhere, particularly in endemic areas [4,12–14], for instance, in the city of Mirjaveh (south-east Islamic Republic of Iran) and Ardestan town (central Islamic Republic of Iran), no association between the sexes and the rate of active lesions was observed [13,14]. Similarly, in Isfahan, the prevalence of acute phase disease in males and females was equal in children and in adults [7]. The higher rate of CL among males in our study was probably due to the cultural habits of the area, whereby women use well-covered dresses, which minimize the chances of sandfly bites. In addition, women are obliged to be home before evening, the onset of the period of sandfly activity, as observed by Al-Jawabreh et al. in Palestine [18] and Ullah et al. in Pakistan [19]. Men are also more likely to travel for work and women tend to be restricted to the house, which is another likely factor for the higher rate in males. Men sleep without shirts and work semi-covered during the summer, thus exposing themselves to sandflies.
Most of the infections were in individuals aged 21–40 years (36.5% in ages 21–30 years and 35.0% in ages 31–40 years), and this rate was significantly higher than in individuals aged ≤ 20 years and those in older age groups. Also, the same pattern of age differences was observed in both sexes. This observation is different to those recently made in endemic areas such as Sabzevar county (Khorasan province), where the most highly infected age group was 0–4 years and the lowest was age 20–24 years [10]. In Isfahan, the acute phase disease was more common among children aged < 5 years [7]. Fazaeli et al. reported in Mirjaveh district (Sistan va Baluchestan province) that the highest rates of active lesions were found in the age group ≤ 10 years, with significant differences compared with the older age groups [14]. The prevalence of CL was the highest in the age group 1–15 years (43.8%) in Pakistan [19] and ≤ 20 years in India [4]. The incidence of CL in children is a useful indicator of the endemicity of the disease in an area and the level of local recent transmission especially in endemic regions. This may be because adult males in the region work on farms and are exposed to the bites of infected sandflies in the evening and at night. Also, adult males (21–40 years old) were more likely to have visited endemic areas for work. Therefore, this difference is probably associated with occupation rather than age. The low rate of active CL among the age group ≤ 10 years, with only 1 case reported, therefore suggests that the disease is not currently endemic in the Borujerd area.
A comparison of the proportion of patients represented by each occupation indicated that in Borujerd county, labourers and drivers were at relatively high risk of CL. Labourers (particular building workers) and drivers (especially drivers of heavy vehicles) are, of course, commonly gender-specific occupations, and labourers and drivers are presumably at increased risk largely or entirely for the same reasons that males are at higher risk than females (as discussed above).
Due to the fact that the Phlebotomus spp. attacks the exposed areas of the body, CL lesions mostly appear on the hands, face and legs [10,19]. However, to date, no study has been done to identify the reservoirs or vectors in the region. In the present study all the lesions (except those on the trunk) were present on the exposed parts of the body, i.e. the sites available for sandfly bites. Similar results have been recorded by other research [10,19,20]. Analysis of the ulcer distribution on the body showed that upper limbs (alone or with ulcers in other sites) were the most affected location (69.3%), followed by lower limbs, face and other parts of the body. Our results were similar to some previous reports [10,20,21]. In Mirjaveh district (south-east of the Islamic Republic of Iran), however, hands were the most affected parts, followed by the face and legs [14] and Ullah et al. in Pakistan showed that lesions were more frequent on the face than the other sites of the body [19]. However, in females in our study, the face and upper limbs were equally affected (6.6% and 5.8% respectively), while in males the pattern was different; 62.8% of ulcers appeared on the upper limbs and only 3.7% on the face (Table 3). The reason for this difference between males and females is not clearly understood. One interesting hypothesis is that the bearded faces of male may inhibit sandflies from biting.
The average number of ulcers was 1.8 per person, with a maximum of 7 lesions. In another study in the Islamic Republic of Iran, an average of 2.14 ulcers per person were found [14] and in Pakistan the reported number of lesions ranged from 1–11 with a mean of 2.3 lesions [19]. The appearance of multiple lesions is also reported to be more frequent with L. major infection than L. tropica, although in some endemic areas single lesions are more predominant [3,7]. We observed that the majority of patients had either a single ulcer (61.3%) or double ulcers (22.6%); only 16.1% showed 3 or more active lesions. The rate of ulcers per person in this study was close to the rates reported previously from the Islamic Republic of Iran [14] and Pakistan [19,21].
Classification of CL based on the clinical presentation and theoretical variations in Leishmania spp. has been made in several studies [22,23]. In order to distinguish between the different types, most authors have divided CL into 2 major forms (“wet” and “dry”), without considering the pathogenesis [2]. Though both dry and wet CL has been reported in the region, the dry type was more frequently observed than the wet type in our study (57.7% versus 42.3%). Wet CL is found in many rural foci of Isfahan [7,8], Khuzestan [11], Shiraz [9] and Khorasan provinces [10], while dry CL is endemic in many large and small cities including Bam and Kerman in the south-east and Shiraz and other cities in Fars province [11,12].
The present data showed seasonal fluctuations in the incidence of CL, with occurrence of the CL ulcers increasing in the spring, followed by the summer. This is more characteristic of the dry form of CL due to factors such as seasonal activity of its parasite vectors and the incubation period of infection with L. tropica. The above characteristics suggest that the CL in the study area is somewhat similar to the typical dry CL; however, it is similar to the wet CL in some characteristics. This observation is different to those recently made in endemic areas such as Mirjaveh district (south-east of Islamic Republic of Iran), where the highest rates of rural CL were found in fall and winter.
Conclusion
The present survey provides preliminary baseline data for the future monitoring of this potentially important parasitic disease in the region. In areas with a longer history of leishmaniasis endemicity, children can be more vulnerable to infection than adults due to adults’ acquired immunity following past parasite exposure. In the study area, however, which is a new focus, this was not the case. Observation of the lowest rate of active CL among the age group ≤ 10 years and the highest rates of active lesions in labourers and drivers travelling to endemic areas indicates that the disease is not currently endemic in Borujerd area, but does not preclude the region potentially becoming an important endemic area of CL in the west of the country. Therefore, active steps are needed by health authorities in order to prevent and control CL, including raising the awareness of local health professionals and the community about the risk of CL and preventive strategies against the disease. Our findings show that Borujerd county now can be added to the list of CL foci in the Islamic Republic of Iran. Further investigations are required to identify the relevant sandfly species, Leishmania spp. and the specific reservoirs of infection in the region.
Acknowledgements
The authors thank all their colleagues who cooperated in this investigation, particularly the staff of the health centre in Borujerd city.
Funding: This investigation was supported by the office of the Vice-Chancellor for Research in the Faculty of Paramedical Sciences, Shahid Beheshti University of Medical Sciences, Islamic Republic of Iran.
Competing interest: None declared.
References
- Control of the leishmaniases. Report of a WHO Expert Committee. Geneva, World Health Organization, 1990:159 (WHO Technical Report Series No. 793).
- Akilov OE, Khachemoune A, Hasan T. Clinical manifestations and classification of Old World cutaneous leishmaniasis. International Journal of Dermatology, 2007, 46:132–142.
- Ashford RW. The leishmaniases as emerging and reemerging zoonoses. International Journal for Parasitology, 2000, 30:1269–1281.
- Sharma NL, Mahajan VK, Negi AK. Epidemiology of a new focus of localized cutaneous leishmaniasis in Himachal Pradesh. Journal of Communicable Diseases, 2005, 37:275–279.
- Aytekin S et al. Clinico-epidemiologic study of cutaneous leishmaniasis in Diyarbakir Turkey. Dermatology, 2006, 12(3):14.
- Rastogi V, Nirwan PS. Cutaneous leishmaniasis: an emerging infection in a non-endemic area and a brief update. Indian Journal of Medical Microbiology, 2007, 25:272–275.
- Momeni AZ, Aminjavaheri M. Clinical picture of cutaneous leishmaniasis in Isfahan, Iran. International Journal of Dermatology, 1994, 33:260–265.
- Salimi M. A clinical and epidemiological comparison on the cutaneous leishmaniasis in the city and villages of Isfahan. Iranian Journal of Public Health, 2000, 2:214–219.
- Razmjou S et al. A new focus of zoonotic cutaneous leishmaniasis in Shiraz, Iran. Transactions of the Royal Society of Tropical Medicine and Hygiene, 2009, 103:727–730.
- Yaghoobi-Ershadi MR et al. Epidemiological study in a new focus of cutaneous leishmaniasis in the Islamic Republic of Iran. Eastern Mediterranean Health Journal, 2003, 9:816–826.
- Nadim A, Seyedi-Rashti MA. A brief review of the epidemiology of various types of leishmaniasis in Iran. Acta Medica Iranica, 1971, 8:99–106.
- Sharifi I et al. Cutaneous leishmaniasis in primary school children in the south-eastern Iranian city of Bam, 1994–95. Bulletin of the World Health Organization, 1998, 76:289–293.
- Yaghoobi-Ershadi MR et al. Epidemiological study in a new focus of cutaneous leishmaniosis due to Leishmania major in Ardestan town, central Iran. Acta Tropica, 2001, 79:115–121.
- Fazaeli A, Fouladi B, Sharifi I. Emergence of cutaneous leishmaniasis in a border area at south-east of Iran: an epidemiological survey. Journal of Vector Borne Diseases, 2009, 46:36–42.
- Brooker S et al. Leishmaniasis in refugee and local Pakistani populations. Emerging Infectious Diseases, 2004, 10:1681–1684.
- Reithinger R et al. Anthroponotic cutaneous leishmaniasis, Kabul, Afghanistan. Emerging Infectious Diseases, 2003, 9:727–729.
- Gurel MS, Ulukanligil M, Ozbilge H. Cutaneous leishmaniasis in Sanliurfa: epidemiologic and clinical features of the last four years (1997–2000). Journal of Dermatology, 2002, 41:32–37.
- Al-Jawabreh A et al. Epidemiology of cutaneous leishmaniasis in the endemic area of Jericho, Palestine. Eastern Mediterranean Health Journal, 2003, 9:805–815.
- Ullah S et al. Prevalence of cutaneous leishmaniasis in Lower Dir District (NWFP), Pakistan. Journal of the Pakistan Association of Dermatologists, 2009, 19:212–215.
- Bosan AH et al. The efficacy of intralesional treatment of cutaneous leishmaniasis with glucantime. Pakistan Journal of Medical Research, 2002, 41:54–57.
- Bari AU et al. Clinico-epidemiological pattern of cutaneous leishmaniasis in armed forces personnel fighting war against terrorism in Khyber Pakhtunkhwa Province and Fata regions. Journal of Pakistan Association of Dermatologists, 2011, 21:10–15.
- Bhutto AM et al. Detection of new endemic areas of cutaneous leishmaniasis in Pakistan: a 6-year study. Journal of Dermatology, 2003, 42:543–548.
- Mujtaba G, Khalid M. Cutaneous leishmaniasis in Multan, Pakistan. International Journal of Dermatology, 1998, 37:843–845.



