Gaza Health Access
|
Click to download
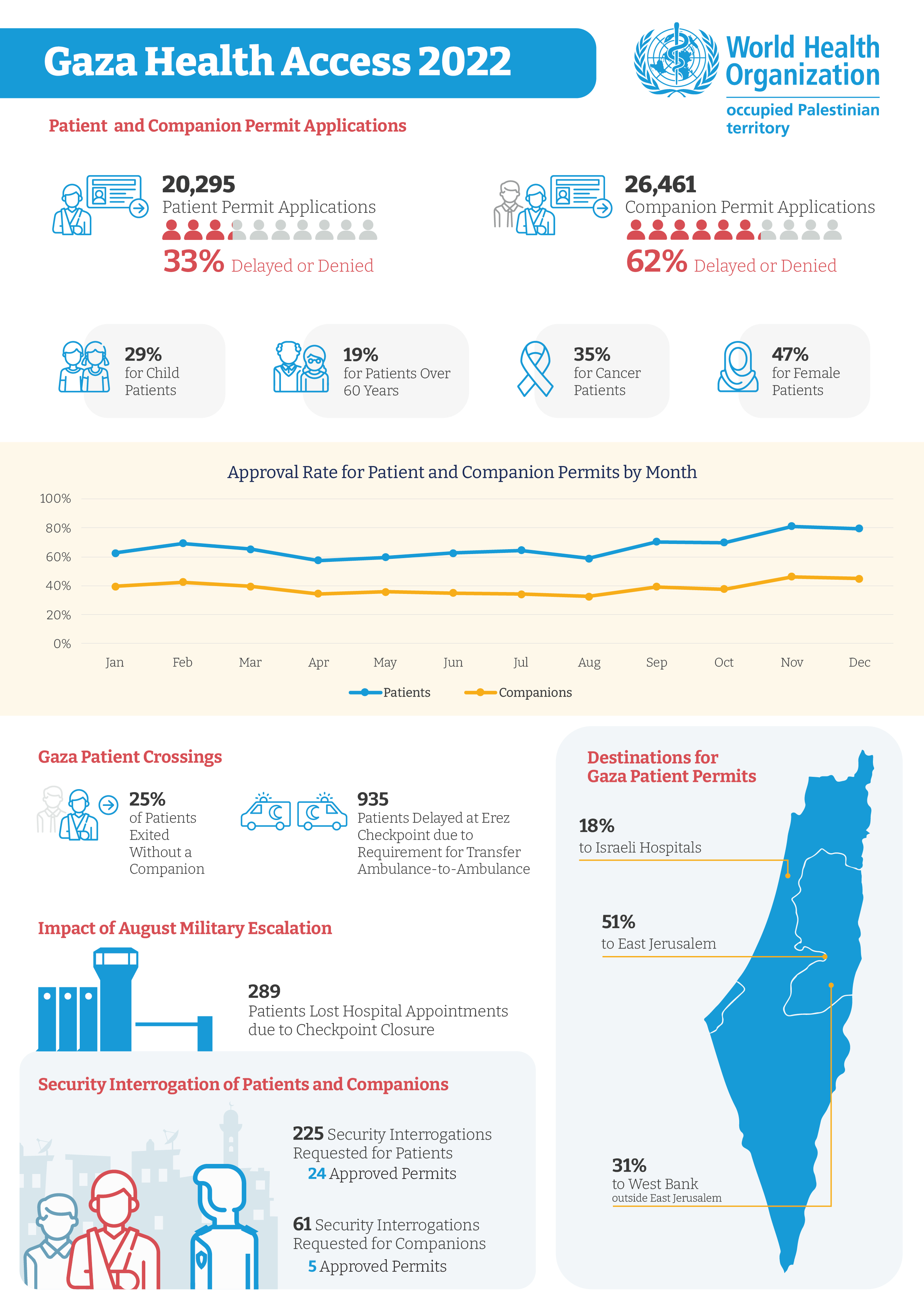
Throughout the year, WHO continued to document the impact of barriers to health access on the Palestinian people in Gaza.
Below are three of the cases documented from 2022 to 2023:
|
Khalid
“He is a patient and has the same right as any person who wants to get treatment.”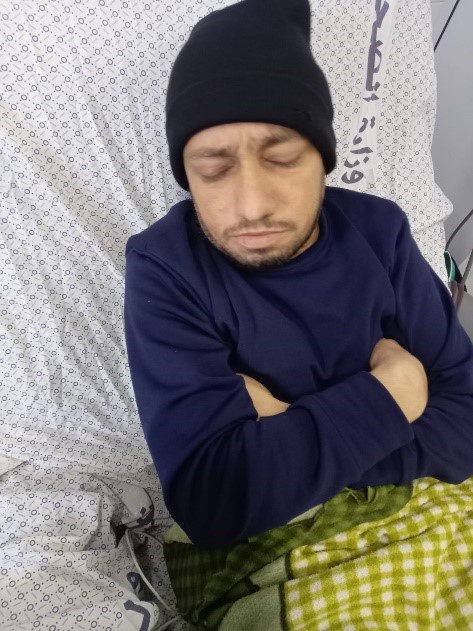
Riham, wife of Khalid
Khalid, 36 years old from Gaza city, has end stage kidney failure. For 16 years, he has been dependent on weekly haemodialysis (a procedure to remove waste and water from the blood, to perform the function of healthy kidneys).
In late 2022, Khalid required referral out of Gaza for vascular surgery so that he would be able to keep having lifesaving haemodialysis. Despite repeated surgeries in Gaza, doctors were unable to establish the vascular access needed for the procedure. At Makassed Hospital in east Jerusalem, Khalid was to receive an artificial blood vessel graft.
In total, Khalid made six permit applications to Israeli authorities. He was never approved a permit to reach Makassed Hospital but was instructed to change the destination and arrange a hospital appointment in Jordan after several appeals through human rights organizations and advocacy by the UN and partners. As of April 2023, Khalid was awaiting financial coverage from the Palestinian Ministry of Health for an appointment at a hospital in Jordan.
Table 1: Khalid’s hospital appointments, intended hospital destination, and permit outcomes
|
Amal
“I don’t know why I am prevented. I have been waiting so long! I need to have this test so the doctor can make a clear diagnosis and give me proper treatment. I suffer and worry every day.”

Amal, 38 years old from Gaza city, was found to have a brain aneurysm (a potentially life-threatening ballooning of a blood vessel) in March 2022.
On 5 June 2022, Amal was referred to An-Najah University Hospital in Nablus, in the West Bank, for brain catheterization and scan (angiography), a procedure not available in the Gaza Strip. She made one permit application for an appointment on 16 June that was delayed. Amal was approved a permit to travel on 3 August but following closure of Erez (Beit Hanoun) checkpoint by Israeli authorities on 2 August she was unable to exit the Gaza Strip to receive care.
Talking about the outcome of her first application, Amal said, “I don’t know why I am prevented, I have been waiting so long! I need to have this test so the doctor can make a clear diagnosis and give me proper treatment. I suffer and worry every day.
”Amal received a further hospital appointment at An-Najah University Hospital for 1 September. She was eagerly awaiting a text message from the Palestinian Health Liaison Office, hoping for a positive response, when WHO spoke with her the day before her appointment. She received the text at 5pm that day and called to ask, “I’ve just received a text message from the Liaison Office. It says under study. What does it mean?” After her initial disappointment, she received another message later that evening saying that she had been approved and could travel the next day.
Amal finally travelled and received the scan she needed. Doctors advised the best course of action would be to manage her condition with medicines, which she now takes daily. “I finally had the tests and I feel so grateful that I won’t need brain surgery after all. The doctors at An-Najah reassured me and prescribed me some medicines. They recommended that I will need follow up to keep an eye on things,” Amal said.
Table 1: Amal’s hospital appointments, intended destination, and permit outcomes

|
Fatma
“When I lost my daughter, I felt that there is no life anymore. I am sure my daughter is not the only one killed by this blockade... Why should my little girl have been denied medical treatment?”
Fatma’s father
Fatma was a 19-month-old girl from Khan Younis in the Gaza Strip. She died on 25 March 2022 after she was delayed access to lifesaving cardiac surgery for nearly three months. Fatma was born with a congenital heart condition known as an atrial septal defect. She needed curative surgery at Makassed Hospital in East Jerusalem and was required by Israel to obtain a permit to reach her hospital appointment. Her family applied three times for permits to reach hospital appointments on 28 December 2021, 13 February 2022, and 5 April 2022. She also received hospital appointments for 6 and 27 March, though at this stage no permit application was submitted by the Palestinian Health Liaison Office. Fatma’s father was told this was because there would not enough time for processing of the permit application.
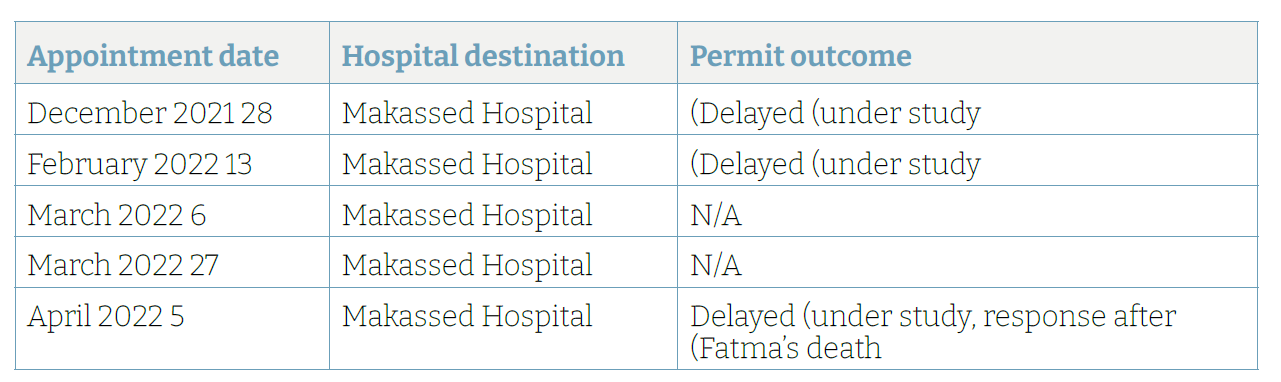
Since December 2021 and her first hospital appointment for heart surgery, Fatma’s health had been gradually deteriorating as her heart began to fail despite medical treatment and follow up by doctors in the Gaza Strip. “I was out the day Fatma died. My brother called and asked me to come home because Fatma was tired. They called an ambulance, which arrived before I got home. She died before she reached the hospital. We were in shock. I felt like I had died,” Fatma’s father said. “Everyone in the family loved Fatma dearly, she was so precious to all of us. Especially to my wife and me. She came to us after five years of fertility treatment. Our hearts are broken.” On 4 April, ten days after Fatma’s death, her family received a text message telling them that Fatma’s application for a patient permit remained under study.
Jalal, the father of Fatima added, “When I lost my daughter, I felt that there is no life anymore. I am sure my daughter is not the only one killed by this blockade. Of course, there are so many patients who have died. But why should my little girl have been denied medical treatment? Can anyone tell me why she deserved this? This killing must be stopped. This could happen to anyone who needs medical care.”
|
|
|
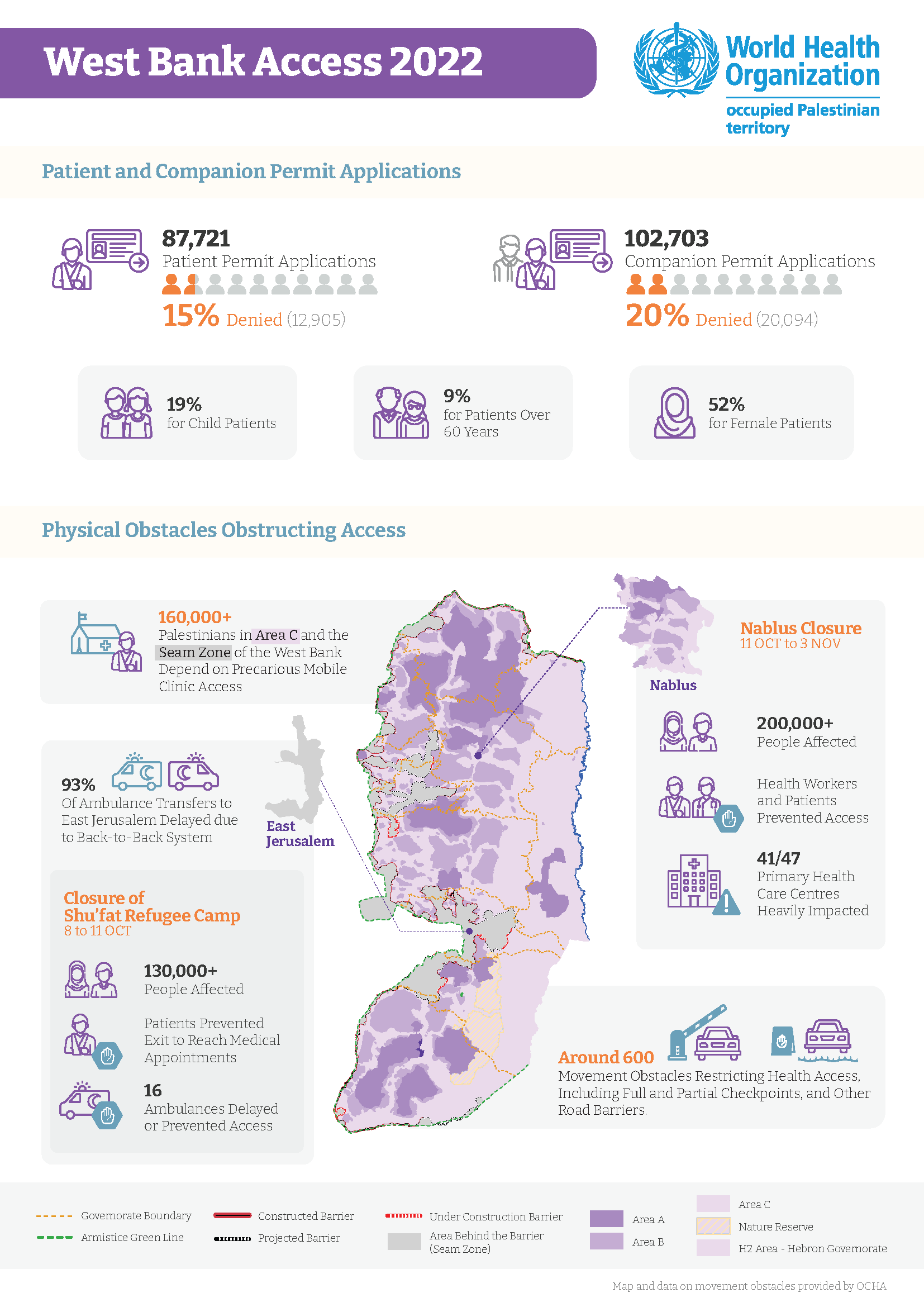
West Bank Health Access
|
Click to download
Throughout the year, WHO continued to document the impact of barriers to health access on the Palestinian people in the West Bank.
Below are three of the cases documented from 2022 to 2023:
|
Musaab
“This is so inhumane. How can this happen in any place in the world? Why are they blocking me from accompanying my son? I just want to hold his hand when he goes for surgery.”
Musaab’s father
Musaab, 21 years old, was in the third year of his university studies in Nablus, in the north of the West Bank.
In the summer of 2022, he was diagnosed with a cancer called a synovial sarcoma in his left ankle. To confirm the diagnosis and to guide the best approach to his treatment, Musaab was referred to Makassed Hospital in East Jerusalem for bone biopsy in June 2022, for an appointment on 6 July. Because of his West Bank ID, Israeli authorities required Musaab to obtain a permit to access East Jerusalem. He applied three times for a permit for his initial hospital appointment and was denied each time. The family were told that Musaab and his companions (different family members for each application) had been denied on security grounds. He eventually received a bone biopsy at Istishari Hospital in Ramallah, where he didn’t require a permit to reach his appointment.
Musaab was in Israeli prison from July 2020 to January 2021. It was during his detention that he started to feel pain in his left ankle. “He was given paracetamol, which didn’t help,” his father said. “He has been suffering a lot. He told me sometimes he felt as if his bone was being crushed.”
After his diagnosis, doctors considered to refer Musaab to Augusta Victoria Hospital, the major Palestinian cancer centre, in East Jerusalem. However, because he had been denied a permit to East Jerusalem previously, the doctors instead referred him to An-Najah University Hospital in Nablus, which meant he didn’t require an Israeli permit to reach care. Musaab received the chemotherapy he needed before he would undergo an operation. By November 2022, he was ready for surgery and his family applied for permits for him to reach Assuta Hospital in Tel Aviv. They wanted a private surgical consultation, to see the extent to which it would be possible to salvage Musaab’s leg. His three applications for a permit to reach two different appointments at the hospital were again denied.
Musaab’s father spoke with a doctor at Makassed Hospital to get advice on how to proceed. “He told me that repeatedly delaying surgery might cause bone erosion requiring leg amputation, God forbid.” The family had lost hope of obtaining a permit to access East Jerusalem, so Musaab’s father went to the Services Purchase Unit (SPU) of the Ministry of Health in Ramallah to request a change of destination to Jordan.
“Musaab and I travelled [to the Jordan border, the King Hussein Bridge] on 12 December. At the Bridge, we were asked to sit and wait. We waited about an hour, then an Israeli officer came out and asked us to go back to the West Bank. He said that we were both denied for security reasons. We refused to leave, and I requested to see the Mukhabarat [intelligence] officer. I insisted, telling them that my son has cancer and that he has the right to access health care. I asked them to let him go. After waiting another four hours, they decided to allow Musaab to cross to Jordan, but they made me return.” Although he crossed, Musaab missed his appointment at King Hussein Cancer Center in Amman, which had been for 12:30pm that day. The next available appointment was a week later.
“My son needs me beside him during these difficult times. We should see the doctor together so we can discuss the different options to help Musaab decide about the surgery.” Musaab’s father appealed through nongovernmental organizations Physicians for Human Rights Israel and Hamoked, as well as through a private lawyer, to get approval to travel to Jordan. He said, “This is so inhumane. How can this happen in any place in the world? Why are they blocking me from accompanying my son? I just want to hold his hand when he goes for surgery.”
|
Moaayd
“These communities face a lot of violations… We should be providing health services at least three times a week, but we cover communities in three districts of the Jordan Valley and there is only so much we can do.”
Moaayd
Moaayd is the driver of a mobile clinic for the Palestine Red Crescent Society (PRCS) operating in the Jordan Valley of the West Bank. He has been part of the team for 10 years, working with communities in remote areas that depend on mobile clinics for access to primary health care. The communities face obstacles to planning and development, demolition orders that make their lives and livelihoods precarious and uncertain, and the under-provision of basic services.
“These communities face a lot of violations. The Red Crescent tried four times to assist with building six houses to provide emergency shelter, but each time the houses were demolished… We should be providing health services at least three times a week, but we cover communities in three districts of the Jordan Valley and there is only so much we can do. To reach all communities, the mobile clinic needs to serve two or three communities at a time. Here in Khirbet Al-Meiteh, some people need to walk half an hour from nearby communities to reach us,” Moaayd comments.
Khirbet Al-Meiteh is a community served by Moaayd’s team, located in Wadi Al-Maleh in the northern Jordan Valley, in the governorate of Tubas. The community of 300 people is situated in Area C, where Israel maintains civil and military control. It lies in an area designated as a firing zone, meaning severe restrictions on planning and development, including for roads, schools, and health facilities. Residents rely on agriculture and pasture for their livelihoods, which are threatened by land confiscations and expanding settlements in the surroundings. There is lack of adequate protection for the communities, who experience settler- and occupation-related violence and who face loss of livelihoods due to destruction of crops and attacks against livestock.
The nearest permanent primary care facility is in Tubas, which would be around 30 minutes away by car without unpredictable checkpoint delays. Many in Khirbet Al-Meiteh do not have a vehicle, so the mobile clinic serves as a vital lifeline for the community. However, the community remains underserved, with expansion of service provision and establishment of permanent facilities needed.
“The mobile clinic covers part of the needs for our community in Wadi Al-Maleh,” says Mahdi, a member of the community council. “However, we desperately need a permanent facility. We tried to build two rooms last year to use them as clinics, but Israeli forces demolished the rooms. We’ve been unable to build them again due to lack of funding.”
The PRCS clinic Moaayd works for covers Tubas, Nablus, and Jericho. Each community or cluster of communities served by the mobile clinic receives one or two visits a month. The clinic itself operates five days a week, providing primary health care on three days and services for women’s health on two days. The team consists of a driver, nurse and doctor, with a social worker joining the team on occasion. Recently, the PRCS community service programme was able to offer additional support to the communities in Wadi Al-Maleh, training youth in the provision of first aid to offer immediate support to injured persons and responding to the high numbers of casualties during demonstrations against settlement expansion.
“As a resident of Tubas, Wadi Al-Maleh is very close to my heart,” Moaayd says. “I feel connected to the people here, and I understand their suffering because I live their experience too. When the community faced demolitions, I was there to help. Despite all our efforts, we need to do a lot more. I’m happy we can provide at least basic health services, but our communities deserve comprehensive health care like all people.”
|
|
Muhannad
“For two days I couldn’t reach work. I would leave my house on foot wearing my paramedic uniform and go to the checkpoint, but the soldiers wouldn’t let me pass.”
Muhannad
From 8 to 11 October, Israel enforced a near-complete closure of Shu’fat refugee camp and adjacent areas of Anata. The area, home to refugees and non-refugees in east Jerusalem, is surrounded by Israel’s separation barrier, which takes the form of an 8- to 9-metre-high concrete wall enclosing the camp. In addition to the existing checkpoint west of the camp, Israeli forces established a flying checkpoint to the east, controlling all movement in and out.
The closure of the camp resulted in severe restrictions on access to health care for the population of 130,000. Ambulances, patients, and health care workers were prevented passage at checkpoints. Muhannad, a paramedic with the Palestine Red Crescent Society (PRCS), was affected and unable to reach his place of work.
“For two days I couldn’t reach work. I would leave my house on foot wearing my paramedic uniform and go to the checkpoint, but the soldiers wouldn’t let me pass.”
With violence and confrontations inside the camp, Muhannad put his skills to use helping people as he could: “I have a paramedic bag from PRCS. I used to take my bag and go to help anyone who had been injured. Yet there was no way to transport them to hospital, the injured had to be treated inside homes or in small clinics. I was exposed when I was caught trying to provide medical assistance to some youth. Some soldiers came from behind and surrounded us. Even though I was wearing my vest and they could see I was holding a first aid kit I was targeted. I hid behind a piece of wood but we were still attacked with rubber bullets until a car came and helped me get out of the area.”
During the period, WHO documented the prevention of access of six ambulances attending to cases with seizures, an injury, chest pain, abdominal pain, a patient requiring kidney dialysis and a woman in delivery. There were an additional ten instances documented of severe delays in access for ambulances. Meanwhile, patients requiring access to primary care and outpatient care outside the camp were prevented from passage at checkpoints, along with health personnel requiring access to places of work.
Obstacles to movement affecting the camp are longstanding. The checkpoint to the west can only be used by residents of Shu’fat refugee camp with east Jerusalem residency. Individuals living in Shu’fat refugee camp with West Bank IDs and approved permits to reach east Jerusalem or Israeli hospitals for health care would have to exit to the east and enter the city via Qalandia checkpoint.
As well as obstacles to movement, residents of Shu’fat refugee camp experience chronic under-provision of municipal services and fragmented provision of health care. Lax building regulations mean that the area is very densely populated, with residents complaining about the quality of housing and overcrowding. Rubbish piles up in the streets due to infrequent refuse collection. Meanwhile, there is differential access to health care for residents with east Jerusalem IDs versus West Bank IDs, as well as for refugees compared to non-refugee residents. During a meeting with UN representatives at the time of the closure, community representatives called for stronger protection from the international community and an end to the severe restrictions on access to the camp.
|
|
|
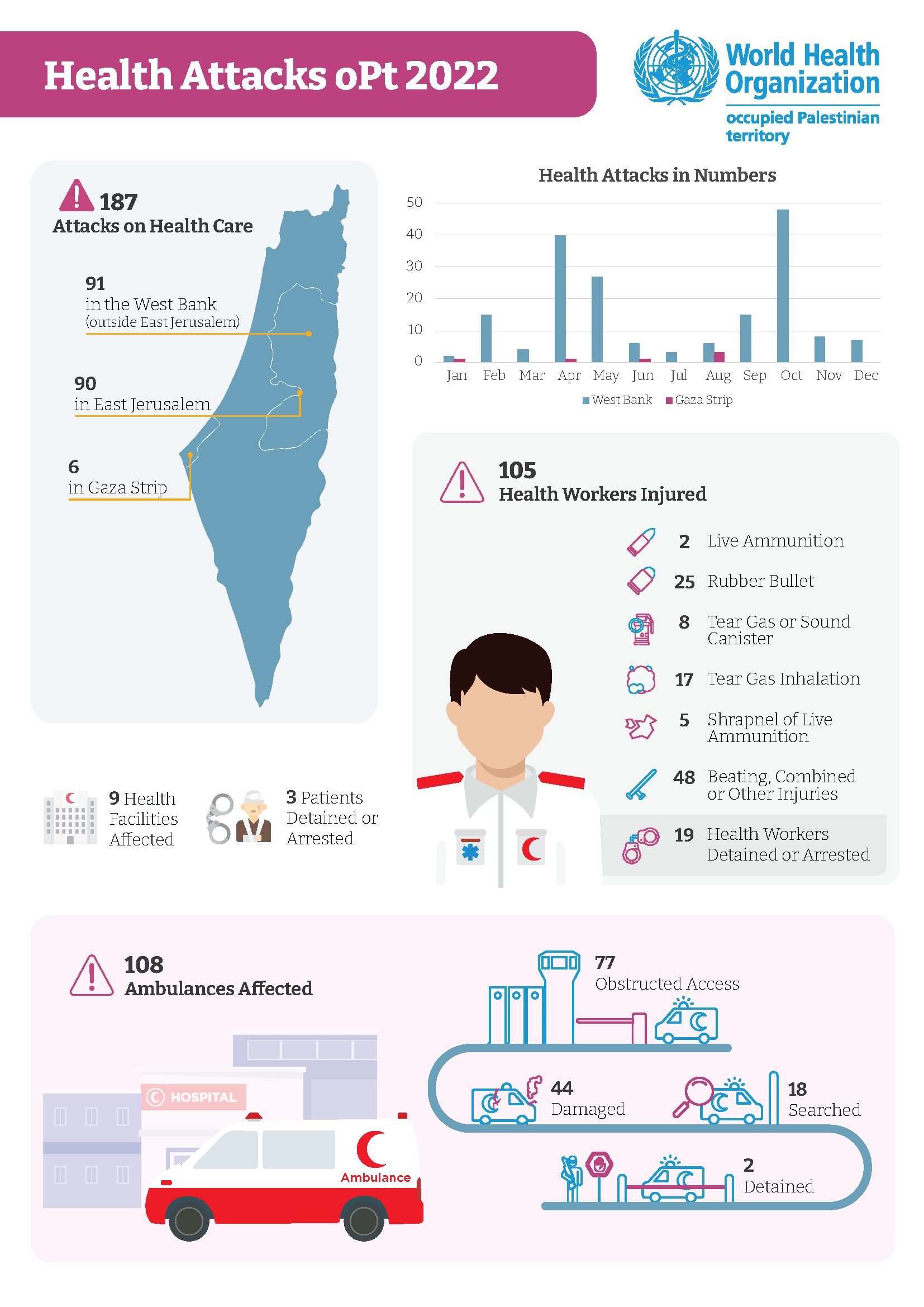
Health Attacks
|
Click to download
Throughout the year, WHO continued to document attacks on health care. Below are four of the cases documented from 2022 to 2023:
|
Ali
“When I responded that I wanted to see what he was doing, the soldier got out of the vehicle and started pushing me and kicking me, hitting me with the back of his gun and causing me to fall to the ground.”
Ali (pseudonym)
On 2 October 2022, a Palestine Red Crescent Society (PRCS) ambulance crew travelled to Beit Furik near Nablus, to provide first aid to persons injured during demonstrations against settlement expansion and incursions in the village, which is in the north of the West Bank.
Ali was driving the ambulance, while his colleague Omar1 sat beside him. They crossed the checkpoint leading to Beit Furik without obstruction. However, as the ambulance approached the entrance to the village the crew was confronted with a temporary (flying) checkpoint comprising Israeli soldiers and border guards.
“The soldiers aimed their guns towards us and were shouting at us, ordering us to stop,” said Ali, the driver. “I was driving very slowly, as we are used to doing in situations like this, and stopped behind one of the military jeeps. A soldier came to the window and told me to turn the engine off and give him the keys. He was banging at the window with the back of his gun. I tried to explain that we had information that there were people injured and we needed to reach them.
“After switching off the engine, the soldiers insisted on searching the vehicle. I offered to go to the back of the vehicle with the soldier to open the ambulance for him, but he refused. We are used to going with the soldiers to open the door. They usually want us to be in front of them when they search a vehicle, but this soldier insisted on going alone. Because of this, I was afraid he might try to plant a weapon or a knife on the vehicle and make an accusation against us. I wanted to see what he was doing, but another soldier stood by my door, aiming his weapon at me, and preventing me from leaving the vehicle or seeing behind.
“The ambulance vehicle automatically locked when the soldier tried to open it. He then shouted towards me ordering me to open the backdoor, which I did. I left the ambulance and went towards the backdoor. At this point the soldier shouted at me again, asking why I was there. When I responded that I wanted to see what he was doing, the soldier got out of the vehicle and started pushing me and kicking me, hitting me with the back of his gun and causing me to fall to the ground.
“Omar came out of the vehicle and tried to help me. Another soldier beside the ambulance came and started pushing Omar, while a further 3 soldiers joined and were surrounding us and pushing us away from the ambulance.”
At the point that Ali and Omar had been pushed away from the vehicle, someone in the nearby demonstration began recording what was happening in a video on their phone. The video shows the soldiers pushing, kicking and beating the paramedics before they are both made to kneel on the ground.
“When we were on the ground, someone was trying to call me. I answered the call on speaker so that the person on the line would know we were in danger. That person contacted the Palestinian Coordination Office, who arrived on site shortly afterwards. Following negotiation, we were released. Another ambulance came to take Omar to hospital for treatment, while I provided information to the officer from the Coordination Office. I then drove myself to hospital.”
As a result of the attack, Ali sustained injuries to his leg including tear of a cartilage in his knee, requiring treatment for the pain and physiotherapy. He returned to work after 40 days.
“Even after my injury, I will go back to the field. Even if it means that something can happen to me, this is our duty. We were raised this way; this is who we are. It’s not the first time I was exposed to violence from soldiers. I worked during the Second Intifada, when we were fired at with live ammunition. We had a female patient in the ambulance at the time. The violations against us have continued all these years. We are still prevented from reaching injured people, pushed around by soldiers, and shot at. Our safety depends on the mood of the soldiers.”
|
Hamzeh
“Around five metres before reaching the guy, I was shot in the right side of my upper body. I went back around two meters and fell to the ground. I told the other paramedics that I had been shot. I felt that my body was being torn apart from the inside.”
Hamzeh
27-year-old Hamzeh Abu Hajar is a volunteer paramedic with the Palestinian Medical Relief Society (PMRS).
In 2022, with increasing escalations across the West Bank, Hamzeh began volunteering as a PMRS first responder.
“Every time the Israeli forces would raid Nablus Old City, I would join the field team. PMRS cars would drive us to different locations where people were injured and needed our help. I always made sure to wear my vest before leaving the house, while PMRS made sure we were all wearing vests by the time we reached a location with injured people… At first, wearing the paramedic vests made us feel protected. However, as the confrontations increased the occupation forces stopped distinguishing between paramedics, journalists, and others. We all feel or show fear in different ways. Of course, I was scared when going into the field, but it wasn’t the kind of fear that would prevent me from going to help the people who depended on us.”
At around 8am on the morning of Friday 30 December, Israeli forces raided Nablus Old City. Hamzeh was called to the field to support treating the injured.
“I heard calls to help with an injury near my location. I immediately went to respond, and there were another two paramedics behind me. Around five metres before reaching the guy, I was shot in the right side of my upper body. I went back around two meters and fell to the ground. I told the other paramedics that I had been shot. I felt that my body was being torn apart from the inside. I was on the ground for several minutes until Al Razi ambulance [a private ambulance] reached me. A sniper had been shooting between the two ambulances on site and me.”
The second ambulance had been from the Palestine Red Crescent Society, which was obstructed from reaching Hamzeh. After Al Razi ambulance reached him, they transferred him to hospital. The ambulance tried to exit via the western route to Rafidia Government Hospital but was again obstructed by Israeli forces, which compelled the team to return and take a different route.
“I remember slipping in and out of consciousness. I vaguely remember being in the ambulance. I also remember my brother, doctors, some of my PMRS friends, and many other people surrounding me in the hospital. I was put in an emergency intensive care room when I reached the hospital and ten minutes later, I was transferred to the operating room.”
Hamzeh’s surgery took 4.5 hours. He stayed in the intensive care unit for 6 days, after which he was transferred to another ward for a further two days before being discharged home. The bullet had injured Hamzeh’s right lung and diaphragm, torn part of his liver and right kidney, and broken four of his ribs. He also suffered a bladder injury. After being shot, the bullet exited from his back, resulting in a tear of his muscle and an open wound around 20 to 25 centimetres in diameter. As a result of his surgery, Hamzeh had 40 stitches in his abdomen, while his back wound remains open and will require several months to heal.
Hamzeh is undergoing a slow recovery. He moves around the house and goes for follow up visits to the hospital every Tuesday. Because of his broken ribs he faces difficulties moving and sleeping. The injury of his lungs means he gets very tired whenever he tries to move around the house.
“Before my injury I witnessed some difficult cases working in the first response teams. I helped provide first aid to people who had very severe injuries. I even had to move people who had been killed. One of the hardest experiences was when I had to move a martyr who turned out to be my friend. I had been with him just a few hours before the raid. I was so shocked to see that it was my friend. Even these experiences didn’t prevent me from going back to the field. On the contrary, it gave me a stronger push to go and to support those in need, especially knowing that they depended on our help. I felt it was my duty to help them. After I fully recover, I plan to return. My mother is worried. She keeps telling me that she doesn’t want me to go back. She says the first time I was lucky, but we don’t know what will happen next time. Still, I plan to return.”
|
Abed
“When they started shooting towards me, I felt helpless. I had the capacity to help – at least to stop his bleeding until we got him to hospital. I knew there were other injuries as well, but I couldn’t reach them…”
Abed
Abed, a 28-year-old paramedic officer working with the Palestinian Medical Relief Society, (PMRS) woke at around 5am on 3 January 2023 to the sound of Israeli forces raiding Dheisheh refugee camp in Bethlehem.
“I heard loud voices near my house. I got dressed and put on my paramedic gear. As I tried to leave my house, heavy shooting toward me started. I then heard Adam Ayad shouting. He was calling for his mother. Another person, one of PMRS volunteer paramedics, was also shouting and calling me to come and help.
“When they started shooting towards me, I felt helpless. I had the capacity to help – at least to stop his bleeding until we got him to hospital. I knew there were other injuries as well, but I couldn’t reach them… I was afraid. Not only for my own safety, but for my family because there was shooting towards my house. One of the bullets hit my brother’s house, near the bedroom, and the bullet could have entered the window and hit him, his wife, or their children. Another bullet entered the bedroom of my uncle’s house… There was heavy shooting although there were no confrontations, the youth from the camp were afraid to come to the area because of the heavy shooting.”
16-year-old Adam Ayad had been shot while inside a car with two others, who were also injured in the incident. With heavy shooting towards the car, Adam got out of the vehicle and tried to hide under it, calling for help. A volunteer paramedic in the field unable to reach him due to the heavy shooting. After a delay several minutes, when the shooting stopped, Abed and the volunteer were able to reach the injured and provide first aid. The volunteer paramedic tended to Adam, while Abed treated the other two persons injured.
“During the incident we were calling for any car to come, we got two cars then I ended up using my own car as a third… We drove to the hospital. I had someone from my family sit in the back and help... He wasn’t trained in first aid, though, so if something were to happen, he would not have been able to help. Meanwhile I was driving so wouldn’t have been able to help.”
There are four first responders for PMRS in Dheisheh camp. Abed is the team leader. After so many fatalities in the camp, Abed arranged with PMRS for a social worker to talk with them. The volunteers blamed themselves for not being able to save people who had been injured, they were questioning the value of their work.
“At the time Sajed Mizher was killed [a paramedic killed in Dheisheh in 2019], we were 8 first responders in the camp. With the increased targeting of first responders and the high levels of violence during raids, people became more reluctant to go into the field during military operations. They are worried for their own safety, especially since there is no ambulance vehicle that can provide some kind of protection. Now we are four. The main fear of the volunteers is to have another person die in their hands. They feel alone.”
Adam Ayad was taken to Al Husein Hospital in Beit Jala, where he was later pronounced dead.
|
Shadi
“I call on international organizations to give us protection. Doctors, nurses, laboratory technicians and ambulances. We live under occupation, and we are exposed to the violence of occupation every day.”
Dr Shadi
On 26 February, Israeli settlers raided Huwara village near Nablus, in the north of the West Bank. Shadi, a doctor working in emergency medicine at Huwara Emergency Medical Centre, spoke about his experience on that day.
“Our team from Huwara Emergency Medical Centre was prevented from access. I wasn’t on duty when it all happened. I was at home, but I was called with other colleagues to assist the team that was on duty. We were forced to use an ambulance to help us reach the medical centre.”
WHO documented nine attacks on health care during the raid, obstruction to access of 7 ambulances and paramedic teams, as well as 8 doctors, with 2 incidents further involving verbal assault and intimidation of medical teams by both soldiers and settlers.
“The ambulances were not able to transfer the injured people or provide them with needed treatment. One of the conditions put on the first responders was that they would have to get out of the ambulance and go on foot to provide treatment in the field, where they were not allowed to evacuate the injured from the location.
“We contacted Rafidia Government Hospital and asked them to send staff to support our team. They sent a team, but the team reached us late because Israeli forces obstructed them at the checkpoint. The ambulance transferring the team was stuck at Huwara checkpoint for two hours, before they took a different route through Awarta checkpoint and reached the medical centre around 11pm.”
A 19-year-old man had suffered a major head injury and needed transfer from Huwara Emergency Medical Centre to Rafidia Government Hospital in Nablus. His transfer was delayed for more than two hours before the crew managed to get coordination for his transfer.
“So many of our staff live in Nablus. When they come to work or leave to return home they are obstructed at checkpoints. Even ambulances – where it is known internationally that they should move freely – are obstructed. I call on international organizations to give us protection. Doctors, nurses, laboratory technicians and ambulances. We live under occupation, and we are exposed to the violence of occupation every day.”
|

